INTRODUCTION
Atherosclerosis and related diseases are leading causes of death in countries where infections are not predominant.[1] Research focused on identifying atherogenic risk factors in children and adolescents shows that significant atherosclerosis precursors in adults are established early in life. This is when patterns of unhealthy diet, physical inactivity and smoking are formed, difficult to change later.[2,3]
Progression and severity of cardiovascular diseases are related to these risk factors and their persistence over time. Furthermore, longitudinal studies in pediatric populations show the tendency of cardiovascular risk factors to persist.[4] Such studies enable identification of persons at risk for cardiovascular diseases based on measurements made early in life. These risk factors may be useful as early screening targets, while care should be taken to correct abnormal values.[5]
Predisposition to atherosclerosis may already exist in childhood, induced by biological factors—both hereditary and nonhereditary—and environmental factors. All of the following in childhood are associated with coronary artery calcification and early cardiovascular disease: obesity, physical inactivity, hypertension (HT), high serum cholesterol, smoking and diabetes.[6]
Study of early signs of atherogenesis has been one of the main objectives of the Havana Atherosclerosis Research and Reference Center (CIRAH) since its creation. Between 1986 and 1996, WHO conducted a multinational research project entitled Pathobiological Determinants of Atherosclerosis in Youth,[6] and Cuba was one of 18 countries involved. Participation in this project led to a number of epidemiological studies demonstrating signs of early atherogenesis (most frequently overweight and HT) in children and adolescents.[7,8]
Hypertension is a major cardiovascular risk factor and is increasing worldwide, provoking extremely important health, social and economic problems. Reported prevalence in Cuban adults is about 30%.[9] Global prevalence in children is not known precisely.[10,11] However, several studies have reported a high frequency of HT and pre-HT in Cuban children and adolescents. Fernández-Britto found 4.7% primary HT and 9.7% pre-HT in a sample of 1026 secondary school (grades 7 to 9) students of both sexes in Havana.[12] Álvarez reported similar findings in Havana,[13] while Suárez identified 9.3% of adolescents as hypertensive in Santiago de Cuba Municipality.[14] Despite these findings, the subject remains to be fully addressed in pediatrics.
Longitudinal studies in children and adolescents demonstrate that high blood pressure persists over time and can predict adult HT.[4,5] Clinical perspectives on blood pressure in children have changed in recent years as a result of improved knowledge of normal values and systematic blood pressure measurement in well child visits. Thus, the importance of including regular blood pressure measurement in clinical practice is now widely recognized, both for early detection of asymptomatic HT in children and adolescents, and because HT early in life constitutes a risk marker for this condition in adulthood.[14] In 2009, the European Society of Hypertension declared HT in children a major and growing health problem requiring organized strategies to address it.[15]
Despite evidence showing the relationship between childhood and adult HT, research conclusions are inconsistent. Explanations of these inconsistencies include differences in cutoff points used, age groups selected, different followup times, and different methods for tracking blood pressure.[16]
Longitudinal studies describing evolution of atherogenic risk factors in children and adolescents are rare in Cuba. The purpose of our research was to describe blood pressure evolution and factors influencing HT persistence and progression in a cohort of Havana adolescents. Study outcomes will expand our knowledge on the subject and provide essential inputs for designing effective interventions at the primary health care level.
METHODS
A longitudinal study was conducted with two cross-sectional cuts, the first in 2004 and the second in 2008. The universe comprised 323 adolescents aged 12–15 years from the catchment area of Héroes del Moncada Polyclinic in Plaza de la Revolución Municipality, Havana, assessed in January–December 2004. Of these, 252 completed the second assessment in December 2008, constituting the study population (22% loss to followup).
Exclusion criteria Residence outside the polyclinic catchment area or absence at the time of the study; obesity or secondary HT; pregnancy or recent childbirth.
Variables These are described in Table 1.
Table 1: Variables

BMI: body mass index / DBP: diastolic blood pressure / HT: hypertension / SBP: systolic blood pressure
Procedures Before the study began, researchers visited each site—the family-doctor-and-nurse office corresponding to each participant—to ensure that measurement conditions were satisfactory. In addition, one of the authors was present at each session to monitor compliance with accuracy standards. Each child was interviewed and examined in the presence of his/her family in order to avoid omission bias regarding family history and birth weight. Data were collected using CIRAH’s primary data collection form.
Anthropometric measurements including weight, height and waist circumference were performed in both assessments. For body mass index, the Quetelet index [weight in kg/(height in m)2] was used. Equipment was calibrated and monitored in accordance with International Biological Program standards.[21] Research team members at each site received training on study procedures, and measurements were taken by the same research team on both study dates.
Initial anthropometric measurements taken at each assessment were replicated twice, for a total of three measurements on the same day, and the average was calculated. As a data quality control procedure, five adolescents were randomly selected and all measurements were repeated. This process included calculation of technical measurement error and reliability index.
Systolic and diastolic blood pressure were taken after subjects had rested for five minutes, each sitting upright with the right arm positioned at heart level,[19] and without having smoked or taken medication that day. An aneroid blood pressure cuff and calibrated stethoscope (SMIC, China) were used. Repeated measurements were taken at five-minute intervals.
Statistical analysis Data were processed with SPSS for Windows, version 18.0. Persistence was analyzed by building dual-entry tables to relate blood pressure classification on initial assessment with that of final assessment. Odds ratios and 95% confidence intervals were calculated for blood pressure alteration at age 16–19 years. Classification trees were used as prognostic models for pre-HT and HT at final assessment, based on factors identified initially. The classification trees allowed us to identify which independent variables were most important as predictors of blood pressure alterations at age 16–19 years. They are also a practical, easily interpreted method for determining HT persistence and establishing optimal cutoff points for the sample. The chi-square automatic interaction detection method was used.[22] The classification trees were constructed with ordinal variables, and also with continuous variables in order to find optimal cutoff points according to their original measurements. Two variants were used for continuous variables: as continuous variables and as categorical synthetic variables. In practice, the latter may be a preferred option because it provides simpler prediction algorithms, while the former is more informative analytically, since it further proposes optimal cutoff points and allows for inclusion of possible nonlinear relationships among predictors and risk, thereby producing more sensitive forecasts.
Ethical considerations The study was reviewed and approved by the CIRAH ethics committee. Written informed consent was obtained from the participants and their parents or guardians.
RESULTS
Mean participant age was 13.2 years at the first assessment, and 17.1 years at the second. Sex composition was balanced.
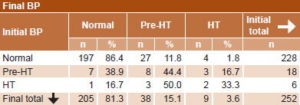
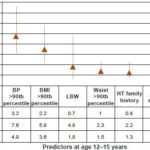
HT was detected in six teenagers in the initial assessment, of whom only one moved to a lower percentile after four years. Of the 18 prehypertensive teens, 8 (44.4%) persisted as such, and 3 (16.7%) progressed to HT (Table 2). The OR for HT in the second measurement was 4.9 for adolescents with blood pressure >90th percentile at age 12–15 years. Next, in order of importance, came BMI >90th percentile (OR 3.6), low birth weight, and waist circumference >90th percentile (Figure 1).
Table 2: Relationship between initial and final BP classifications
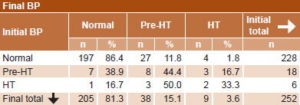
BP: blood pressure / HT: hypertension / Pre-HT: pre-hypertension
Figure 1: Risk of abnormal BP at age 16–19 according to predictors at age 12–15 years
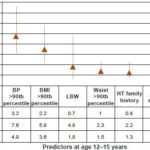
BMI: body mass index / BP: blood pressure / CI: confidence interval / HT: hypertension / LBW: low birth weight
At each step, the chi-square automatic interaction detection classification tree effected different partitions, choosing from among all independent variables entered into the model the one showing the strongest interaction with the dependent variable. Blood pressure classification in the initial assessment at the beginning of the study, nutritional assessment classification, waist circumference, and family history of HT and smoking were introduced into the model. Blood pressure classification at the beginning of the study was selected by the model as the most important variable for predicting being prehypertensive or hypertensive at the second assessment. Figure 2 shows the classification tree with blood pressure as a categorical variable. Teens who initially had altered blood pressure had a 66.7% risk of being hypertensive or prehypertensive by age 16–19.
Figure 2: Prediction of BP at age 16–19 years by BP at age 12–15 years (CHAID classification tree, categorical variable)

BP1: blood pressure at age 12–15 years / BP2: blood pressure at age 16–19 years / CHAID: chi-square automatic interaction detection
By introducing as predictors the independent variables SBP, DBP, waist circumference and BMI treated as continuous, the model made two partitions, selecting first SBP and then BMI. When SBP at age 12–15 years was >110 mmHg, risk of becoming prehypertensive or hypertensive was about 50%. If SBP was between 98–110 mmHg, with a BMI >20.4, risk was almost 30% (Figure 3).
When stratified by sex, different effects of continuous variables were observed for male and female subjects. The most important variable for male subjects was SBP, followed by BMI. When SBP values at age 12–15 were >110 mmHg, the probability of becoming hypertensive or prehypertensive in 4 years’ time was 68%. For female subjects, however, the tree structure changed completely, especially in the terminal nodes, showing waist circumference as the main variable, followed by DBP, with a risk of 24% if waist circumference was >68 cm, increasing to 36.7% if DBP >60 mmHg was also present at the beginning of the study (Figure 4).
DISCUSSION
Adolescence is a complex stage of human development because the growth that has occurred continuously from conception is combined with signs of maturity apparent with the onset of puberty. During this stage, behavioral patterns are established and some risk factors come to light that influence health at the beginning of adulthood.
Blood pressure values in childhood tend to remain on the same growth curve over time, which means that children in higher blood pressure percentiles will remain in that range into adulthood. This tracking pattern starts early on, which supports the hypothesis that primary HT begins in childhood.[23]
Although information regarding progression from pre-HT to HT among adolescents is limited, the persistence of HT observed in this study is in line with research suggesting that children and adolescents with blood pressure at the high end of the distribution tend to have HT as young adults.[5,16,23]
Figure 3: Prediction of BP at age 16–19 years by BP at age 12–15 years (CHAID classification tree, continuous variable)

BMI1: body mass index at age 12–15 SBP1: systolic blood pressure at age 12–15 years
BP2: blood pressure at age 16–19 CHAID: chi-square automatic interaction detection
Data from a US study to determine the consequences of HT in adolescence suggest that progression from pre-HT to HT (based on a single measurement) is approximately 7% per year, and that pre-HT carries a high risk of progression to HT in adolescence.[10] It is estimated that individuals with DBP near 90 mmHg when aged 15 years are twice as likely to have DBP >90 mmHg at age 35 years as those with lower initial values.[24–26]
Field reported a risk of developing altered blood pressure 5.1 times higher in children with BMI >85th percentile.[27] The classification trees in our study confirmed the persistence of HT through adolescence. Furthermore, results showed that BMI at age 12–15 years is associated with alterations in blood pressure later in adolescence. This relationship could be explained by three main pathophysiological mechanisms: impaired autonomic function, insulin resistance, and abnormalities in vascular structure and function. This link may be mediated by the sympathetic nervous system, with a hyperactive state that has been confirmed in different studies involving obese children and adolescents.[28]
Lower vascular compliance has been found in obese children, similar to that of children with diabetes and familial hypercholesterolemia. Endothelial dysfunction has also been suggested as a problem associated with obesity. Recent research links obesity, C-reactive protein and SBP, suggesting a possible pathophysiological mechanism: impaired vascular function caused by chronic inflammation in obese children as a predictor for developing HT.[29,30]
A cohort study of Brazilian children who were followed for 17 years to adulthood showed that sustained elevated blood pressure was associated with a more unfavorable cardiovascular risk profile, with higher prevalence of HT, overweight/obesity, lipid and glucose abnormalities, and metabolic syndrome in adulthood,[31] confirming the need for preventive measures beginning early in life.
Figure 4: Prediction of BP at age 16–19 years by BP at age 12–15 years (classification trees, continuous variables), by sex

BMI1: body mass index at age 12–15 years SBP1: systolic blood pressure at age 12–15 years
BP2: blood pressure at age 16–19 years DBP1: diastolic blood pressure at age 12–15 years
Waist1: waist circumference at age 12–15 years
Sex differences found in the classification trees highlight the behavior of this variable as an effect modifier. It should be borne in mind that in the first stage of the research, children were between early and middle adolescence, which coincides with a period of rapid growth. Increases in blood pressure with age are related to body size and can differ by sex, since puberty occurs at different ages for boys and girls. Puberty is a time of important anthropometric, hormonal and lipid changes associated with sexual maturation, which contribute to differences in cardiovascular risk factors between the sexes.[23,32,33]
Evidence suggests that elevated blood pressure in childhood is a predictor for HT in adulthood and that some lifestyle-related risk factors, such as unhealthy diet and physical inactivity, remain stable from childhood on; hence prevention is more effective if lifestyles are changed early in life.[33]
While some research conducted in Cuba shows early atherogenic signs in children and adolescents, few studies aim at understanding its progression.[1,7,8,12–14] Pérez addressed the question of progression to HT in a longitudinal study involving prehypertensive children in the city of Santa Clara. He concluded that the interaction from adolescence to adulthood of such factors as age at onset of pre-HT, birth weight, family obesity and an unfavorable family environment contributed to progression from pre-HT to HT.[34]
This study describes the progression of HT in a cohort of adolescents. Within its scope, it was possible to identify early signs of atherogenesis in a group of adolescents who appeared healthy when first examined. This research demonstrates the need for appropriate blood pressure screening and management in order to avoid adverse health outcomes later in life.
CONCLUSION
The high persistence and the progression of HT in adolescence highlight the need for systematic screening at the primary health care level as well as adoption of primary prevention strategies from an early age.