INTRODUCTION
From 2000 to 2050, the number of people aged ≥60 years will increase from 600 million to 2 billion, and by 2050 will make up 22% of the world’s population. Four fifths of these older adults will live in Asia, Africa and Latin America.[1] Population aging is associated with the current epidemic of chronic diseases, explaining their greater disease burden in these regions.[2,3]
According to the World Alzheimer Report 2016 there were 47 million people living with dementia,[4] and the World Alzheimer Report 2015 estimated 9.9 million new cases every year.[5] In 2001, 60% of persons with dementia were living in developing countries, and this percentage is predicted to increase to 71% by 2040. Currently, 1.8 million people in Latin America have dementia, and the number is expected to climb to 4.1 million by 2020 and 9.1 million by 2040 similar to the number of people with dementia in the USA and Canada predicted for 2040.[5]
Dementia is responsible for 11.2% of years lived with disability in persons aged ≥60 years, a higher percentage than cerebrovascular disease (9.5%), musculoskeletal diseases (8.9%), cardiovascular disease (5.0%) and cancer (2.4%).[3] Furthermore, the annual cost of caring for people with dementia is estimated to be 818 billion dollars worldwide; 70% of these expenditures will be in the USA, Canada and Europe.[6] The enormous costs of dementia and the challenge posed by increasing numbers of older adults will lead to substantial changes in health care systems around the world. As the number of people with dementia is doubling every 20 years,[5] costs can be expected to increase proportionally. However, the greatest cost of dementia is human, and its dimensions are inestimable.
Cuba is currently the “oldest” country in Latin America, with 2,180,000 persons aged ≥60 years, just over 19% of its population in 2015. This proportion will grow to 25% by 2020, when it is projected that 400,000 people will be aged ≥80 years.[7]
Longitudinal studies facilitate investigation of determinants of life expectancy, risk factors for chronic diseases and states such as dependency and frailty, and their association with mortality. There is growing interest in studying frailty and its risk factors, due to its importance for designing preventive interventions to alter the processes of aging, dependency and mortality.
Aging and Alzheimer is a prospective, longitudinal study of 2944 older Cuban adults, two phases of which have been completed.
The study began in 2003, with the purpose of (a) ascertaining the prevalence and incidence of dementia and its most frequent type, Alzheimer disease, (b) identifying risk factors for dementia and their association with other chronic non-communicable diseases in this age group (cerebrovascular disease, diabetes, hypertension), and (c) doing an in-depth study of their risk and genetic markers, and their impact in terms of needs for care, disability and caregiver psychological morbidity. The project also contemplates a third phase to learn about trends in dementia and evaluate the impact of a community intervention strategy, for which the first two phases have laid the statistical and operational groundwork.
This article describes lessons learned in the Aging and Alzheimer longitudinal study, begun in 2003, starting with its planning and design. The study has revealed the high prevalence of dementia in Cuba, its risk factors and its consequences in terms of caregiver burden and need for care. It also describes experiences that lay the groundwork for design and implementation of a community intervention strategy.
INTERVENTION
Study design Aging and Alzheimer is a prospective cohort study involving 2944 adults aged ≥65 years. Methodology and design are detailed in other publications.[8,9] The study involved participation of primary, secondary and tertiary health institutions; health professionals from various specialties, including medical and psychology students; and volunteers, groups and family associations that helped to recruit and encourage participants and their families.
Of the 2944 participants in the study, 2043 came from seven Havana Province polyclinic health areas and 901 from Milanés Polyclinic in the city of Matanzas. Polyclinics are primary health care institutions to which a number of family doctor-and-nurse offices report and that provide services in primary care specialties, including pediatrics, gynecology, psychiatry, internal medicine, psychology, rehabilitation, imaging, clinical laboratory and dentistry.[10] Participating polyclinics in Havana Province (municipality in parentheses) were: 19 de Abril (Plaza); Ana Betancourt (Playa); Cristóbal Labra (La Lisa); 27 de Noviembre, Ramón González Coro and José M. Portuondo (all in Marianao); and 14 de Junio Polyclinic (10 de Octubre).
Instruments The assessment protocol was based on the 10/66 Dementia Research Group questionnaire involving a structured interview covering sociodemographic characteristics, health status, lifestyles and risk factors;[8,9] a physical exam, which included a neurological study; and an interview with a reliable informant (who, in the judgment of the family and surveyor, best knew the participant, and who in most cases was a relative living in the home, and the primary caretaker). All materials, questionnaires and assessments had been previously validated to permit their utilization in populations with different cultures and educational levels. The final version was reviewed by a steering committee (project head and principal investigators for content areas). A procedural manual and a training video for physical and neurological exams were prepared. In each phase, all researchers and participants from the health area received an intensive one-week training given by the senior researcher on use of the instruments and surveys. Instruments were administered by these trained medical specialists, with support from psychology and medical students.[9]
Interviews and questionnaire administration were done in participants’ homes, lasting an average of 1½–2 hours. A specialist in the research group reviewed 5% of interviews, randomly selected, for quality control. Interviews and physical exams were done in a single visit. Table 1 shows the main variables and instruments used in the two previous assessments and for the assessments to be done in 2016–2018, incorporating lessons learned.
Data processing and analysis Interviewers entered questionnaire data and responses in Epidat (version 3.1) software, and then exported the information to SPSS (version 18).
Table 1: Variables and aspects probed in assessments for the Aging and Alzheimer Study, by study phase

*Measurements to be considered in the 2016–2018 assessment
CERAD: The Consortium to Establish a Registry for Alzheimer’s Disease
CSI‘D’: Community Screening Instrument for Dementia
DEMQOL: Dementia quality of life questionnaire
GMS: Geriatric Mental State Examination
HAS: History and Aetiology Schedule
MCH: mean corpuscular hemoglobin
MCHC: mean corpuscular hemoglobin concentration
MCV: mean cell volume
NPI: Neuropsychiatric Inventory
WHODAS: World Health Organization Disability Assessment Schedule
Ethics The study protocol was approved by the Medical University of Havana’s Ethics Committee and by those of each polyclinic. During home visits, participants and their families received information sheets that explained the study, benefits of participation, absence of risk, and data confidentiality, and assured them that they could withdraw from the study at any time without affecting relations with their health care team. Once so informed, participants and family members provided written consent.
LESSONS LEARNED
To our knowledge, the Aging and Alzheimer project is the largest longitudinal study of older adults in the Cuban population. It has produced estimates of prevalence, incidence and risk factors for dementia and associated comorbidities (including cerebrovascular disease, diabetes mellitus, ischemic heart disease and hypertension), and conditions such as frailty, disability and dependency.
Sociodemographic characteristics and results of the first assessment done in 2003–2006 of 2944 participants have been published.[9,18] Using 10/66 criteria, prevalence of dementia syndrome in adults aged ≥65 years was estimated to be 10.8% (women 11.6%, 95% CI 10.3%–13.1%; men 9.2%, 95% CI 7.6%–11.2%). Using DSM-IV criteria, overall prevalence was estimated to be 6.4% (women 7.1%, 95% CI 6.1%–8.4%; men 5.2%, 95% CI 4.0%–6.7).
Alzheimer disease is the most frequent cause of dementia, followed by vascular dementias. Age-specific DSM-IV prevalence rates are slightly higher in Cuba (with an age- and sex-standardized morbidity ratio of 1.08) than those reported in the EURODEM study, a meta-analysis of 14 European studies.[18]
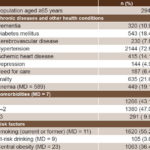
Prevalence of chronic non-communicable diseases in participating older adults is high (Table 2); in decreasing order of frequency, they are: hypertension, diabetes mellitus, ischemic heart disease, dementia and cerebrovascular disease. A little over one-fifth of patients were diagnosed as frail, 19.1% were anemic and 6.4% needed care most of the time; 56.9% of interviewees had ≥1 illness.[19]
Table 2: Chronic non-communicable diseases and other health conditions in the first assessment
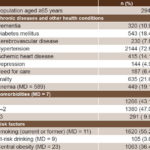
MD: missing data
In 2007–2011 a second assessment was done of the cohort, composed of 2010 surviving participants from the first assessment who gave their consent, with 4.1 years of followup. Annual dementia incidence was 21.2 per 1000 population aged ≥65 years. Dementia was associated with different risk factors, in particular: advanced age (RR 1.79, 95% CI 1.37%–2.39%), hypertension (RR 1.35, 95% CI 1.02%–2.37%), cerebrovascular disease (RR 2.84, 95% CI 1.20%–6.72%), carrying one or two alleles of the ApoE4 gene (RR 1.93, 95% CI 1.03%–3.81%), Parkinsonian signs (RR 1.18, 95% CI 1.05%–1.33%) and mild cognitive impairment (RR 2.21, 95% CI 1.12%–4.93%). Higher educational level was a protective factor (RR 0.77, 95% CI 0.67%–0.98%).[18] Dementia incidence was similar to that reported by the Canadian Study of Health and Aging, the most extensive longitudinal study of adults aged ≥65 years in the world, which reported an annual incidence of 21.8 per 1000 women and 19.1 per 1000 men.[20]
In 2011–2013, the study analyzed, among other variables, frailty and dependency associated with dementia and other chronic diseases of aging, as well as mortality. Prevalence of frailty syndrome was 21.6% (95% CI 17.9%–23.8%). This syndrome was associated with increasing age, anemia and comorbidity. Incidence of dependency was 33.1 per 1000 population/year (95% CI 29.1%–37.6%) and mortality was 55.1 per 1000 population/year. Advanced age, male sex, lower lifetime occupational status, dependency, frailty syndrome, dementia, depression, cerebrovascular disease and diabetes were associated with higher risk of death.[21]
More than any other physical or mental illness, dementia has two important consequences that in turn have a social impact on older adults: need for care, and family members being obliged to stop working to assume the caregiver role. It is also the source of great psychological strain on caregivers.[18]
One limitation of the study is that its results cannot be generalized to all of Cuba. However, the strategy of surveying the entire population in selected areas increases the response rate (above 95% for both the first and second assessments) and facilitates longitudinal followup. Having specialized personnel administer a standardized questionnaire in a single visit is a strength of the study. This protocol was validated for the Cuban population and case followup confirmed reliability and validity of the diagnosis and information obtained.[19] This enabled us to obtain detailed information on participants’ physical and mental health, risk factors, need for care and impact on families and on society.
The results have contributed to better knowledge of dementia and associated comorbidity patterns in the older adults, at a time when we are seeing accelerated demographic aging and an epidemiological transition in Cuba. They imply the urgent need to implement intervention and prevention strategies for various age-related conditions, in particular, disability, frailty and dependency. The demonstration of feasibility and validity of a design free of transcultural or educational bias in a one-phase diagnostic protocol for epidemiological studies of dementias is unprecedented in Cuba.
Furthermore, having evidence of the number of ill people in a community and the impact this has, has raised awareness among the public and policymakers responsible for addressing this growing health problem.
The study demonstrates that levels of stress and burden on caregivers of people with dementia are as high as those typically reported in developed countries, despite strong traditions and extended families in Cuban society.[19] A five-session education and training intervention program for caregivers has been developed, particularly useful because it can be taught by nurses, medical students and social workers; it is expected to be validated in phase three of the study.
Cognitive stimulation therapy for people with mild cognitive impairment and early-stage dementia has been provided as part of these population studies. Also, as part of the project, two university extension programs were created (the Alois Alzheimer Program at the Medical University of Havana and the “Healthy Mind in a Healthy Body” Integration program at the Medical University of Matanzas) that link students to research and community intervention not only for dementias, but also for other frequent diseases and conditions of aging, including their prevention, early diagnosis and help for families.
As a result of lessons learned, a third assessment will be conducted in 2016–2018, in the same study areas. Using a new census, 3000 persons aged ≥65 years will be selected, including earlier study participants who are still alive. The protocol will be similar to the one used for the preceding assessments, with the addition of tests to diagnose frailty syndrome (dynamometry, spirometry), along with blood sampling for supplementary testing and detection of biological markers for dementia, frailty and immunosenescence. The objective of the study’s third phase is to learn about changes in dementia prevalence a decade after the baseline study and to provide more in-depth study of conditions such as frailty and dependency and their relationship to Cuba’s demographic aging and health transition.
Another lesson learned is the need to evaluate the effectiveness of a community intervention strategy for primary health care for frail and dependent older adults, to address illnesses and conditions that predispose to dementia, frailty and dependency in older adults. This is why older adults diagnosed as frail and dependent will receive a care program. This will be a horizontal intervention delivered by nurses and nonprofessional health workers (including medical students) under the supervision of primary care physicians. It will target disabilities (immobility/inactivity syndrome, malnutrition, incontinence, impaired vision and hearing, behavioral symptoms and depression) that coexist with other comorbidities and chronic non-communicable diseases.