CHRONIC KIDNEY DISEASE THREATENS RURAL COMMUNITIES
Chronic kidney disease (CKD) is a global public health problem due to its high prevalence in both initial and final (renal failure) stages, and to the high cost and poor results of treatment.[1] Epidemiological studies of the adult population in several countries report CKD prevalence of 9%–11%: USA 11% (NHANES III),[2] Spain 9.1% (EPIRCE),[3] and the Netherlands 10.6% (PREVEND).[4] These studies used albuminuria (a renal damage marker) or glomerular filtration rate (GFR) < 60 mL/min/1.73 m2 body surface area to diagnose CKD. Higher prevalences were seen in studies that added hematuria as a third criterion: Australia 16% (AusDiab Kidney Study)[5] and Cuba 20.8% (ISYS).[6] Prevalence of GFR < 60 mL/min/1.73 m2 is 4.9% in USA,[2] 6.8% in Spain,[3] 5.5% in the Netherlands,[4] and 1.1% in Cuba.[6] In general, prevalence is higher in women than men: USA 5.3% and 3.5%, respectively,[2] and Spain 7.7% and 6.2%, respectively.[3] CKD prevalence increases with age, and is highest at ages >60 years.[2–6] Main CKD causes reported in US predialysis patients include diabetes (49.1%), hypertension (28%) and glomerulonephritis (4.7%).[7] Diabetes is also the main cause of CKD (58%–60%) in new renal replacement therapy (RRT) patients in Malaysia, Morelos and Jalisco (Mexico), Thailand, New Zealand, Hong Kong, Japan, USA and other countries.[7] CKD mortality rates have been increasing globally, from 9.6 per 100,000 population in 1999 to 11.1 per 100,000 in 2010.[8]
Nevertheless, there is substantial regional variation in CKD prevalence, patient demographics and associated risk factors. Historically, the main causes of CKD are diabetes and hypertension, associated with aging and obesity in developed countries, and now in some developing countries. In addition to these “traditional” causes, glomerular and tubulointerstitial diseases due to infections, nephrotoxic drugs and herbal medications, environmental toxins and occupational exposure to pesticides—the so-called “nontraditional” causes—contribute to CKD burden in developing countries.[1,9,10] From the 1990s, an increase in CKD prevalence[2–4] and emergence of a CKD of unknown etiology (CKDu) was observed in several countries: El Salvador,[11–15] Nicaragua,[16,17] Costa Rica,[18] Sri Lanka,[19–22] Egypt[23–25] and India.[26,27] This new disease has different epidemiological characteristics than traditional CKD—most notably its predominance in young male farmworkers—and has become an important health problem. The purpose of this essay is to examine CKDu’s case definition(s), epidemiology and causal hypotheses in reports of CKDu epidemics in agricultural communities globally.
APPROACH
We conducted a MEDLINE search using the following terms: chronic kidney (renal) disease, chronic renal failure, chronic kidney disease of unknown origin, epidemiology, prevalence, risk factors. Supplementary sources were obtained from bibliographies of retrieved articles selected. Publications and workshop reports on CKDu from scientific societies, health ministries and national and international organizations and from regional workshops on CKDu were also reviewed, notably:
- Recommendations from the First Workshop on Renal Health of the Ministry of Public Health and Social Assistance of El Salvador, 2010[28]
- Report from the First International Research Workshop on Mesoamerican Nephropathy (MeN), 2012[29]
- Declaration of Roatán, Honduras, 2013 (Nephrology Societies of Central America and the Caribbean)[30]
- San Salvador Declaration: Comprehensive Management of Chronic Tubulointerstitial Kidney Disease of Central America (CTKDC) that Predominantly Affects Agricultural Communities, El Salvador, 2013 (Ministers of Health of Central America and the Dominican Republic)[31]
- Chronic kidney disease in agricultural communities in Central America, 2013 (PAHO Document CE152/25. 152nd Session of the Executive Committee)[32]
Publications on CKDu are limited in some countries and the available information comes from documents and reports in the grey literature that usually do not provide details on study methods. For this reason, we pooled all available information, selecting those that provided evidence and used internationally accepted CKD diagnostic criteria: presence of structural or functional kidney alterations for ≥3 months. CKD is classified in stages by glomerular filtrate rate (GFR, in mL/min/1.73 m2 body surface area): stage 1, >90 with renal damage markers; stage 2, 60–89, with renal damage markers; stage 3a, 45–59; stage 3b, 30–44; stage 4, 15–29; and stage 5, < 15.[33,34] All articles were reviewed that provided pertinent information, according to their methodologies (such as population-based epidemiological studies, clinical descriptive studies and case-control studies).
FINDINGS
Case definition As yet, there is no consensus on a case definition for CKDu; diagnosis is by exclusion. In general, such diagnosis is presumed when patients fulfilled CKD criteria,[33,34] without evidence that it is due to diabetes, hypertension, glomerular proteinuric disease, polycystic kidneys, obstructive uropathy or other recognized causes. In Sri Lanka it is defined as CKD in the absence of past history of diabetes, chronic or severe arterial hypertension, snake bite, glomerulonephritis or other urinary tract disease; and with normal glycosylated hemoglobin (< 6.5%) and blood pressure < 160/100 mmHg in untreated patients or < 140/90 mmHg in patients receiving up to 2 antihypertensive drugs.[35] A case definition for Mesoamerican nephropathy was proposed at the 2012 workshop: abnormal renal function by international standards in persons who live in Mesoamerica and have no known CKD cause.[29] In general, CKDu patients belong to agricultural communities in specific high-prevalence areas and are mainly young male farmworkers (women are also affected). Levels of proteinuria and albuminuria tend to be low.[11–17]
Nomenclature Different terms have been used to label CKDu in the medical literature: chronic kidney disease of unknown origin; chronic kidney disease of uncertain origin; chronic kidney disease of unknown etiology. In some cases, it is named for the region or country where it appears: Central American nephropathy;[28] Salvadoran agricultural nephropathy;[13] Mesoamerican epidemic nephropathy;[29] chronic tubulointerstitial kidney disease of Central America;[31] Udhanam endemic nephropathy (India);[27] or Sri Lankan agricultural nephropathy.[36]
Epidemiology of CKDu in agricultural communities We examined reports of CKDu from El Salvador, Nicaragua, Costa Rica, Sri Lanka, Egypt and India to determine whether the epidemiologic pattern is local or global.[11–27]
Central America Growing numbers of CKD patients and increased CKD mortality have been observed in this region over the last two decades, particularly in Nicaragua and El Salvador.[37,38] PAHO has reported CKD-specific mortality (deaths per 100,000 population associated with CKD stages 3a, 3b, 4 and 5) in the region: Nicaragua (42.8), El Salvador (41.9), Guatemala (13.6) and Panama (12.3).[32] CKD mortality rates in Nicaragua and El Salvador are 4 times global CKD mortality rates[8] and 17 times the lowest CKD mortality reported in the Americas region. Mortality rates in men are three times those of women.[32]
El Salvador. The Salvadoran Ministry of Health’s (MINSAL) 2012–2013 annual report cited “genitourinary disease, mainly end-stage renal disease (ESRD),” as first cause of hospital mortality overall, and first cause of hospital deaths in men. Mortality rates per 100,000 population for CKD increased in most of the country’s departments compared to 2011, with rates of 6.7–28 for the 14 departments; the highest rates were observed in the departments of Usulután (28.8), San Miguel (25.6), La Unión (19.9) and La Paz (16.3). Hospital case fatality was 12.6%.[39] An RRT study found prevalence of 12.5 per 100,000 population nationally, with highest in La Paz (25.3), San Miguel (18.1), San Vicente (18), San Salvador (15.4) and Usulután (12.7). Prevalence was higher in men than women (18.1 vs. 7), and most patients were aged 20–60 years; 67% reported no previous pathology at time of CKD diagnosis.[40]
One of the first publications to sound the alarm on CKDu was a hospital study of 205 new dialysis patients (1999–2000). For 135 of these, CKD cause was unknown; it was unassociated with diabetes, hypertension, primary glomerular diseases or obstructive uropathy. Patients were predominantly men (118/87.4% vs. 17/12.6% women); mean age was 51±16.1 years; 63% worked in agriculture; and 73.3% had been exposed to agrochemicals. Authors suggested exposure to such toxic chemicals as a possible causal factor.[11]
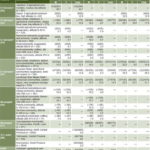
Various methods have been used for population studies to analyze frequency and distribution of CKD and its risk factors. In one study of 291 men in two communities (one at low altitude on the Pacific coast, the other at higher altitude, 500 m), proteinuria prevalence was 45.7% and 12.9%, respectively (Table 1). Of patients with proteinuria and increased serum creatinine (≥1.5 mg/dL), 62.2% had no known cause of CKD. Living close to sea level was an important risk factor (OR 8.04), but no association was found between proteinuria and working in agriculture, pesticide exposure or alcohol use.[12]
Another CKD prevalence study was done in five communities at different altitudes and dependent on differing economic activities, to assess effects of occupational and environmental exposure and heat stress. A total of 664 adults aged 20–60 years were studied. Two communities were on the coast (altitude 0–50 m), one a rural community dedicated to sugarcane production, the other a semirural community producing sugarcane and providing services. In both, prevalence of reduced GFR (<60 mL/min/1.73 m2) was higher in men than in women (18.9% vs. 7.9% and 18.3% vs. 8.1%, respectively). [14]
Prevalence was much lower in the other three communities at higher altitudes: sugarcane community at >500 m (1.8% in men, 3.1% women); coffee-producing community at 1650 m (0% men, 1.2% women); and an urban community at 650 m (0% men, 2.4% women) (Table 1). Main findings were increased prevalence of reduced GFR in sugarcane-producing communities at lower altitudes (ergo with higher temperatures); and male predominance, but also measurable risk of reduced renal function in women. A long history of working in sugarcane or cotton increased risk in both sexes. No increased risk was seen in sugarcane workers at higher altitudes, hence the authors’ suggestions that arduous work in hot environments, with repeated dehydration, may be associated with higher risk for reduced kidney function in both sexes.[14]
A 2009 study of CKD and CKDu prevalence and risk factors in adults in three agricultural communities involved 775 persons aged ≥18 years (343 men, 432 women[13]). High CKD prevalences were reported: 17.9% overall, 25.7% in men and 11.8% in women (Table 1). For both sexes, CKDu prevalence was higher than that of CKD associated with traditional causes; 54.7% of those with CKD had no diabetes, hypertension or primary glomerular disease. Prevalence of GFR < 60 mL/min/1.73 m2, was also high, at 9.8% (men 17%, women 4.1%). An early decline in renal function was seen, and associations were found between CKD and age, male sex, hypertension, and family history of CKD. Authors suggested that male farmworkers bear a multiple burden of risk factors, traditional and nontraditional, occupational and environmental, that might act synergistically to damage the kidneys. Exposure to agrochemicals had a significant effect in univariate but not multivariate analysis.[13] Other studies in the communities of Bajo Lempa, Guayapa Abajo and Las Brisas reported CKD prevalences of 15.4%, 20.5% and 21.1% respectively; and reduced GFR prevalences of 8.8%, 13.3% and 13.3% respectively (Table 1); in 51.9% of CKD patients, traditional causes did not explain their diagnosis.[15]
Table 1: Prevalence of CKD in rural adults, by geographical distribution
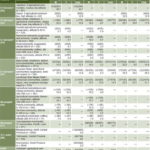
— Data not provided in source article CKD: chronic kidney disease GFR: glomerular filtration rate
a Diagnosis confirmed after 3 months
b <60 mL/min/1.73 m2 body surface area
c Single sample, without diagnostic confirmation
Nicaragua. A 2009 review of CKD epidemiology in Nicaragua found mortality associated with CKD rose from 4.5 to 10.9 per 100,000 habitants between 1992 and 2005, with greatest increases in León and Chinandega departments. Prevalences reported ranged from 0 to13.1% (median 8.7%), with prevalence >8% in communities growing sugarcane and bananas, and in mining areas. Young men were the most affected (prevalence 3.1%–38.1%). Prevalence was lower in coffee-growing communities and those providing services. The studies reported positive associations between CKD and agricultural work, pesticide exposure, dehydration, hypertension, drinking lija (homemade alcohol) and a family history of CKD.[41]
A 2007 study of 1096 persons aged 20–60 years was conducted in 5 small towns in northeastern Nicaragua, located at different altitudes and dependent on different economic activities. The prevalence of GFR<60 mL/min/1.73 m2 was higher in men than in women in the towns dedicated to gold mining and subsistence farming (altitude 200–300 m); banana and sugarcane cultivation (altitude 100–200 m); fishing towns (altitude 0–100 m); and coffee cultivation (altitude 200–675 m). Neither sex had reduced GFR in the sea-level service town (Table 1). The authors stressed as new findings the high prevalence of reduced renal function in male small-scale production workers, construction workers and miners, and in female farmworkers. Since there was no increase in renal pathology in service towns at 0–100 m, authors concluded that low altitude was not a risk factor for CKD. The weak association found between reduced renal function and the conventional risk factors led authors to hypothesize that work overload at high temperatures produces chronic dehydration and kidney damage.[16]
Another prevalence study was done in a sample of 771 residents aged >18 years in Quetzalguaque, a Pacific coastal municipality with 22 communities in León Department. Some 80% of participants lived at <500 m, of whom 13% (98) had reduced GFR. The median age of CKD patients was 57 years, and prevalence in men was 2.6 times that in women. No association was found with diabetes.[17]
Boston University researchers reported results from CKD studies in western Nicaragua in 2009–2012. Urine levels of NGAL and NAG, markers of tubulointerstitial damage, were determined in 248 workers aged 20–59 years—some from the San Antonio sugar plantation and others who had never worked in sugar, but rather in other industries (mining, construction and ports). Results suggested that primary renal damage was tubulointerstitial. Prevalence of CKD stages 3 and 4 was 8% in dockworkers, 6% in miners, 6% in cane cutters and 3% in construction workers, all higher than expected in a population of young men. Increased NGAL and NAG were significantly associated with reduced GFR. The authors concluded that workers in these and other industries suffer tubulointerstitial injury that may increase CKD risk.[42]
To determine if renal damage preceded occupational exposure, the same researchers studied 200 adolescents (aged 12–19 years) from 4 schools in areas located at different altitudes and with different CKD mortality rates. Investigators assessed urinary markers of tubular damage (NGAL, NAG, IL-18) and glomerular damage (albumin/creatinine ratio, ACR). There was no evidence of glomerular damage. High IL-18 values were detected in all age groups and both sexes, consistent with CKD involving tubular damage, which authors inferred was the central pathology of the epidemic. Girls had higher levels of all markers than boys. Researchers concluded that renal damage occurred at early ages, but did not draw final conclusions, because the study was preliminary and sample size small.[42]
Costa Rica. A CKD epidemic has been reported in Guanacaste, in northern Costa Rica, in which the disease did not follow traditional epidemiological patterns found in the rest of the country. The disease appeared in men aged 20–40 years who worked for long periods on sugarcane plantations. Clinical presentation and histopathology were compatible with chronic interstitial nephritis and authors suggested exploring the work environment for possible associated risk factors.[18]
In summary, in Central America, the most important new findings regarding CKD’s epidemiological behavior have come from studies in El Salvador, Nicaragua and Costa Rica; we found no related publications from other countries in the region. Population prevalence studies have relied on different criteria, with prevalences ranging from 17.9% to 21.1% when diagnosis was confirmed at 3 months.[13,15] Prevalence of GFR <60 mL/min/1.73 m2 in a single sample varies between 0% and 20.1% in men and from 0% to 8.1% in women (Table 1),[12,14,16,17] higher than reported internationally for CKD of traditional causes (men 3.5%–6.2%, women 5.3%–7.7%).[2,3] In agricultural communities at low altitudes, mainly sugarcane-growing areas, prevalence in men was 16.9%–20.1% and in women 4%–8.1%, lower at higher altitudes: 0%–7.5% in men and 1.2%–5.4% in women. In service communities at lower altitudes and an urban community at higher altitude, CKD was not seen in men, and prevalence in women ranged from 0% to 2.4%.[13,14,16,17] In 57.4%–66.8% of patients, the cause remained unknown.[11,13]
CKDu in Central America affects mainly young men, between the third and fifth decades of life, working in agriculture (mainly sugarcane or other agricultural activities at lower altitudes and consequent higher temperatures). Women are less affected than men, but CKDu prevalence in women is higher than CKD prevalence seen in international studies.[2,3] Further research is needed on CKDu in women who do not work in agriculture,[15] as well as in adolescents before entering the workforce, who nevertheless present evidence of tubular damage.[42]
Clinically, CKDu is characterized by minor or no proteinuria or albuminuria; patients are identified late, mainly by reduced GFR without other urinary markers of renal damage. Clinical data suggest chronic interstitial nephropathy, which has been corroborated by renal biopsies in Costa Rica[18] and more recently in El Salvador.[43] Another study of eight patients with CKDu in the same country, however, found lesions in both structures, glomerular and tubular.[44]
Although CKDu etiology in Central America remains unclear, it appears to be multicausal. Two hypotheses have emerged. One identifies the trigger as exposure to agrochemicals—whether higher in farmworkers and associated with other occupational risk factors such as exhaustion and dehydration, or contaminating the physical environment, water and food, possibly explaining CKDu’s occurrence in women and adolescents not working in agriculture. This hypothesis also includes negative social determinants in these disadvantaged populations.
A study of 46 CKDu patients in El Salvador found additional extrarenal manifestations (such as reflex abnormalities and sensorineural hearing loss) from early CKD stages, not explicable by uremia observed in ESRD. This suggests generalized toxicity affecting different organs and systems, with renal damage just one element in a systemic pathology. The kidney is hit doubly hard because of the concentration of renally-excreted toxins, a situation that may worsen further with dehydration in situations of profuse sweating and low fluid intake in hot working environments.[45]
A second hypothesis emphasizes the critical effect of heat stress, complicated by strenuous labor and insufficient fluid intake, triggering repeated episodes of acute subclinical renal injury that could lead to chronic kidney damage. CKDu in miners—who work in exhausting conditions at low altitudes and are exposed to high temperatures—supports this hypothesis. Several authors nevertheless do not rule out agrochemicals as a cofactor.[14,16,46]
Other countries Sri Lanka. CKD is an important health problem in some regions of Sri Lanka, where it was first detected in the 1990s in North Central Province. A retrospective study (2000–2002) of 492 CKD patients in 2 hospitals reported CKD unassociated with traditional risk factors in 54% and 82% of patients, respectively. Most patients were young men of low socioeconomic status from agricultural communities in North Central Province.[19]
In another study of 6153 persons aged >19 years in 3 regions of Sri Lanka, morning urine samples were analyzed for proteinuria by dipstick.[20] Cases were identified as proteinuric CKD when 2 of 3 samples taken at ≥3-week intervals over 3 months were +1 or higher (>30 mg/dL), with confirmation of proteinuria by sulfosalicylic test. Serum creatinine was analyzed and GFR calculated in positive cases. CKD prevalences are displayed in Table 1. Regression analysis of pooled data from the three regions yielded as risk factors age >60 years, agricultural work, family history of CKD and exposure to agrochemicals. However, upon analysis by region, the proportion of CKD patients with CKDu in Medawachchiya, North Central Province (84%), was substantially higher than in Hambantota (9.1%) and Yatinawara (2.9%), located in South and Central provinces respectively. In Medawachchiya, a high proportion of CKDu patients were young male farmworkers, and both young age and agricultural work were independently associated with CKDu.[20] Renal biopsy was performed on 26 Medawachchiya patients (19 in CKD stages 1–3) and revealed chronic tubulointerstitial nephritis.[20] Another study of renal biopsies from 57 CKDu patients also concluded that the primary renal pathology was tubulointerstitial.[21]
Several environmental contaminants have been studied by Sri Lanka’s Ministry of Health in collaboration with WHO and Sri Lanka’s National Science Foundation, searching for etiological agents. Findings showed a 15% prevalence of CKDu in the population aged 15–70 years in North Central and Uva provinces, with men most affected. Patients’ urine contained high levels of arsenic and cadmium, both of which, plus lead, were found in agrochemicals sampled. It was hypothesized that the population could be exposed to these contaminants through food and drinking water, and that water hardness could play a role. Thus, it has been proposed that such routes of environmental exposure to combinations of nephrotoxic agents (rather than just a single substance), acting with predisposing factors, could lead to development of CKDu.[20,35]
Egypt. Between 2002 and 2007, ESRD prevalence increased from 250 to 367 per million population in Egypt’s El Minia Governorate, the cause unknown in 27% of patients.[23,24] A case-control study of ESRD patients found an association with rural residence (76% vs. 57% nonrural, p <0.001), unsafe drinking water (72% vs. 48%, p <0.001), family history of CKD (10% vs. 4%, p <0.001), pesticide exposure (52% vs. 14%, p <0.001), and medicinal plant use (34% vs. 6%, p <0.001). The authors concluded that the disease may be attributed to environmental factors.[25]
India. India’s CKD registry reported diabetic nephropathy in 31.3% of 52,273 CKD patients in 2006–2010, making it the leading cause of CKD; CKDu, found in 16% of CKD patients, was second. According to the report, there is no published information about CKDu from the 1990s, when it is surmised that the disease begin to emerge. CKDu is most frequent in young, low-income patients, and is characterized clinically by no or mild hypertension and proteinuria. Since there are few symptoms, it is usually diagnosed at advanced stages.[26]
Another study in the Udhanam coastal region (Andhra Pradesh District) revealed proteinuria prevalence of 15.3% (54/354) in an agricultural community dedicated primarily to cultivating coconuts, as well as rice, jackfruit and cashews—higher in men than women (20% vs. 12% respectively). Prevalences of CKD and reduced GFR are displayed in Table 1. Proteinuria in younger age groups was mild to moderate. Renal pathology studies revealed chronic tubulointerstitial nephritis. The author considered environmental exposure to toxic agents the most likely cause.[27]
Unresolved global questions In Sri Lanka, Egypt and India, CKDu has similar epidemiological, clinical, and histopathological characteristics as those described in Central America, suggesting a more generalized problem. However, if it is a global disease: When did it begin in these countries? Did it appear in all at the same time? Are there countries where it exists but has not yet been detected? According to available information, the disease was first detected in the 1990s. Since the populations most seriously affected live in rural areas with limited economic resources and often little access to health services, it may be that CKDu was present well before detected. The first alerts came from dialysis services in some countries, and such services have limited coverage because of their high cost. On the other hand, if the disease was not present before the decade of the 90s, then what new factors have been introduced, or what existing factors have changed that might promote emergence in specific communities? Responses to these as-yet unanswered questions should provide important clues to possible causal factors.
Public health perspective The scientific community and international health organizations recognize CKDu as an urgent health problem.[28–32,35,46–49] Thus far, we do know that it primarily affects socially vulnerable groups from rural communities, mainly young male farmworkers. We surmise that it might be caused by a combination of environmental and occupational factors, such as exposures to toxins and high temperatures, inadequate fluid intake and dehydration.
Common themes among the many recommendations made are the need for more research, and for a more comprehensive approach to addressing CKDu. Although science has not yet provided conclusive answers to etiology, the hypothesized causal factors are potentially preventable, and there is scope for intersectoral action on social and environmental determinants, workplace health and safety, health promotion at individual and community levels, early detection and timely treatment. Furthermore, it is critically important to strengthen health service networks, with models that ensure quality of care and patient safety, as well as availability of human resources, medications, health technologies and, critically, adequate financing. Finally, surveillance systems must be reinforced, in order to assess CKDu trends and intervention impacts.
CONCLUSIONS
Since the multifactorial conditions associated with CKDu development are already present in many countries’ poor agricultural communities, it is crucial to coordinate efforts to identify etiological factors as well as to develop proactive and comprehensive approaches to prevent and treat the disease.