INTRODUCTION
Worldwide, it is estimated that more than 160,000 children aged <14 years are diagnosed with cancer every year, although this figure may be low given lack of reliable data, even in developed countries. An estimated 80% of these children live in developing countries, a proportion expected to increase with improved prevention and control of infectious diseases.[1] In Cuba, cancer is the second leading cause of death in the population aged 1–19 years and the main cause of years of potential life lost (17.5 years in 2008).[2]
The main reason estimates of childhood cancer incidence are imprecise is that many countries—developed as well as undeveloping—do not have national cancer registries.[1,3-5] Analyzing reported incidence rates is further complicated by the lack of a uniform definition of childhood with standard age limits in different countries, registries and studies.[6] Childhood cancer incidence is often reported per population aged <15 years; this age cutoff makes registration of cases diagnosed in adolescents difficult, creating in turn a major problem for epidemiological analysis of cancer in the population aged 15–19 years.
Neoplasms in children are classified by morphology (histology), according to the International Classification of Childhood Cancer (ICCC), whereas in adults, they are classified primarily by topography (site), according to the International Classification of Diseases for Oncology (ICD-O).[7] In children aged <15 years, 92% of neoplasms are non-epithelial and only 8% epithelial. Between the ages of 15 and 19 years, a transition towards an inverse situation begins, so that between the ages of 30 and 45 years, 80% of neoplasms are epithelial, reaching 90% with increasing age.[8]
The ICCC classifies neoplasms into 12 diagnostic groups and 47 subgroups. The 12 main groups are: I) leukemias; II) lymphomas and reticuloendothelial neoplasms; III) central nervous system (CNS) and miscellaneous intracranial and intraspinal neoplasms; IV) neuroblastoma and other peripheral nervous cell tumors; V) retinoblastoma; VI) renal tumors; VII) hepatic tumors; VIII) malignant bone tumors; IX) soft tissue and other extraosseous sarcomas; X) germ cell tumors, trophoblastic tumors, and neoplasms of gonads; XI) other malignant epithelial neoplasms and malignant melanomas; and XII) other and unspecified malignant neoplasms.[7]
Several authors have proposed that the group aged 15–19 years be included in reports of childhood cancer data.[5,9–12] The World Health Organization (WHO) has also recommended that adolescence be considered age 10–19 years, divided for statistical purposes into 2 groups: early adolescence (age 10–14 years) and late adolescence (age 15–19 years).[13]
Cuba has maintained a National Cancer Registry (NCR) since 1964. Cancer incidence data is continuously and systematically gathered and processed, and used for statistical analysis applied to cancer control efforts and evaluation of the disease’s impact on the community.[14,15] In the national public health system, all patients aged ≤19 years are cared for in pediatric hospitals throughout the country, and all cases diagnosed and/or treated in Cuba’s 9 pediatric oncology centers are classified according to the ICCC and reported to the NCR.
Nevertheless, in the Ministry of Public Health’s Statistical Yearbook, cancer incidence in children aged <15 years (calculated using NCR provisional or definitive data) is described using the ICCC, and incidence in the population aged ≥15 years is described by topography,[2] thus preventing an accurate epidemiological analysis of cancer risk in the “late adolescent” group (aged 15–19). In the present study, the population aged 15–19 years is included for the first time in an analysis of childhood cancer incidence in Cuba.
The objectives of this study are to describe childhood cancer incidence in the Cuban population aged ≤19 years in 2001–2003 using the International Classification of Childhood Cancer, and to describe geographic distribution of incidence of childhood cancer in Cuba by sex and by the three diagnostic groups with highest incidence.
METHODS
A descriptive study of childhood cancer incidence was conducted using National Cancer Registry data for 2001–2003, the most recent period for which definitive figures are available. A 3-year period was selected to facilitate obtaining more precise estimates and to minimize the effect of random fluctuations from one year to another when calculating adjusted rates.
Incidence was analyzed by age group, and 5 age groups were established: <1, 1–4, 5–9, 10–14 and 15–19 years. Tumors were classified according to ICCC diagnostic groups and subgroups. Total number of cases registered in each diagnostic group during the study period was recorded, and the corresponding percentages of overall childhood cancer was calculated. Number of cases in each diagnostic group and subgroup was also recorded by age group, and the age-specific rate per 100,000 population aged ≤19 years (ASR) was calculated by age group, as well as the age-adjusted rate to the standard world population aged ≤19 years (AAR), using the direct standardization method.[15]
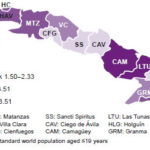
Once leukemias, lymphomas and CNS tumors were defined as the three diagnostic groups with highest childhood cancer incidence in Cuba, their AAR were used to analyze childhood cancer risk by sex and geographical distribution in the country’s 14 provinces and Isle of Youth Special Municipality. AAR percentiles (P25, P50, P75) were calculated to establish 4 risk levels: low risk, P<25; intermediate risk, P25–50; high risk P51–75 and very high risk, P>75.
Incidence was presented in tables by diagnostic group and age group, and risk levels were represented by keyed shading of territories in a political map of Cuba.
RESULTS
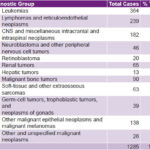
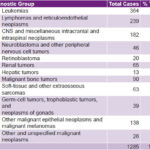
In Cuba, 87,634 new cancer cases were reported to the National Cancer Registry in 2001–2003, of which 1285 were childhood cancers (Table 1). Cancer in the population aged ≤19 years accounted for 1.5% of total cancer (annual average about 400 cases).
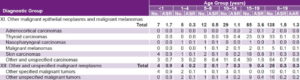
Table 1: Incidence of Childhood Cancer* in Cuba, 2001–2003

* Diagnostic Groups I-XII ASR: Age-specific rate per 100,000 population aged ≤19 years. AAR: Age-adjusted rate, standard world population aged ≤19 years. Source: National Cancer Registry of Cuba
During the period analyzed, overall incidence was 13.9 per 100,000 population aged ≤19 years (AAR). Highest risk was found in children aged <1 year with an ASR of 21.9 per 100,000 population aged ≤19 years (Table 1).
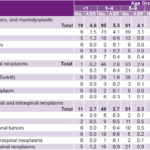
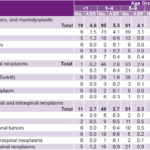
Frequency was highest (61.1%) in the three primary diagnostic groups: leukemias (Group I, 28.3%), lymphomas (Group II, 18.6%) and CNS tumors (Group III, 14.2%) (Table 2). Among leukemias—the diagnostic group with highest incidence (AAR 4.0)—the subgroup with highest incidence was lymphoid leukemias (AAR 2.7), predominantly in the group aged 1–4 years (ASR 4.1) (Table 3).
Table 2: Childhood Cancer by Diagnostic Group, Cuba, 2001–2003
Source: National Cancer Registry of Cuba
Incidence of Diagnostic Group II cancers (lymphomas and reticuloendothelial neoplasms) was 2.5 (AAR). The group at highest risk was aged 15–19 years (ASR 3.2), and the diagnostic subgroup with highest incidence was non-Hodgkin lymphomas (AAR 1.2), predominantly in the groups aged 5–9 years (ASR 1.7) and 1–4 years (ASR 1.6). In the Hodgkin lymphoma subgroup, the group aged 15–19 years also had an ASR of 1.7 (Table 3).
Table 3: Incidence of Childhood Cancer in Cuba. Diagnostic Groups I–III, 2001–2003
ASR: Age-specific rate per 100,000 population aged ≤19 years. AAR: Age-adjusted rate, standard world population aged ≤19 years. Source: National Cancer Registry of Cuba
Diagnostic Group III (CNS neoplasms) had the third highest incidence (AAR 2.0). Two age groups, aged 1–4 years and < 1 year, shared highest risk (ASR 2.7 for both). Among the diagnostic subgroups, unspecified neoplasms had highest incidence (AAR 0.8), predominantly in children aged < 1 year (ASR 1.2) (Table 3).
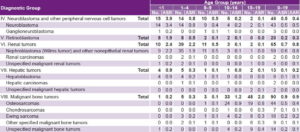
Incidence of diagnostic Group IV cancers (neuroblastoma and other peripheral nervous cell tumors) was 0.4 (AAR). Children aged <1 year were at highest risk overall (ASR 3.9) and for neuroblastoma (ASR 3.4), the subgroup with highest incidence (AAR 0.5). Incidence of retinoblastomas (Group V, AAR 0.3) was also highest in the same age group (ASR 1.9) (Table 4).
Table 4: Incidence of Childhood Cancer in Cuba. Diagnostic Groups IV–VIII, 2001–2003
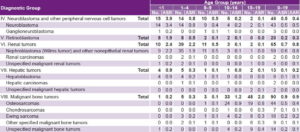
ASR: Age-specific rate per 100,000 population aged ≤19 years. AAR: Age-adjusted rate, standard world population aged ≤19 years. Source: National Cancer Registry of Cuba
In Group VI (renal tumors), nephroblastoma (Wilms tumor) constituted the majority of cases (59/65 total) with an incidence of 0.8 (AAR) in both the diagnostic group and this subgroup. The group at highest risk for both was aged <1 year (ASR 2.4 and 2.2, respectively).
Hepatic tumors (Group VII) was the diagnostic group with lowest incidence (AAR 0.2), affecting predominantly children aged <1 year with hepatoblastoma (ASR 0.9 overall and for this subgroup) (Table 4).
Malignant bone tumors (Group VIII) was the diagnostic group with fifth highest incidence (AAR 0.9), and the group most at risk was aged 15–19 years (ASR 2.0). Osteosarcoma was the diagnostic subgroup with highest incidence (AAR 0.4), predominantly in groups aged 10–14 (ASR 0.9) and 15–19 (ASR 0.8) (Table 4).
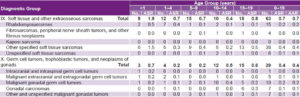
Soft tissue sarcomas (Group IX) had an incidence of 0.7 (AAR) with highest risk in the group aged <1 year (ASR 1.9). The diagnostic subgroups with highest incidence were other specified soft tissue sarcomas (AAR 0.4) followed by rhabdomyosarcomas (AAR 0.2). The group at highest risk for both other specified soft tissue sarcomas and rhabdomyosarcomas was aged <1 year (ASR 1.5 and 0.5, respectively) (Table 5).
Table 5: Incidence of Childhood Cancer in Cuba. Diagnostic Groups IX–X, 2001–2003
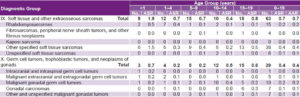
ASR: Age-specific rate per 100,000 population aged ≤19 years. AAR: Age-adjusted rate, standard world population aged ≤19 years. Source: National Cancer Registry of Cuba
Incidence of germ cell tumors, trophoblastic tumors and neoplasms of gonads (Group X) was 0.4 (AAR) and the age groups most at risk were children aged <1 year (ASR 0.7) and 15–19 years (ASR 0.6). Malignant gonadal germ cell tumors was the diagnostic subgroup with highest incidence (AAR 0.2), predominantly in the group aged 10–14 years (0.4 ASR) (Table 5).
Group XI (other malignant epithelial neoplasms and malignant melanomas) was the diagnostic group with fourth highest overall incidence (AAR 1.3) and primary incidence in the group aged 15–19 years (ASR 3.6). The diagnostic subgroup with highest incidence was other and unspecified carcinomas (AAR 0.6), predominantly in the group aged 15–19 years (ASR 1.6) (Table 6).
Table 6: Incidence of Childhood Cancer in Cuba, Diagnostic Groups XI–XII, 2001–2003
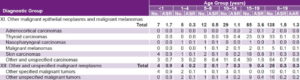
ASR: Age-specific rate per 100,000 population aged ≤19 years. AAR: Age-adjusted rate, standard world population aged ≤19 years. Source: National Cancer Registry of Cuba
The last diagnostic group, other and unspecified malignant neoplasms (Group XII), had an incidence of 0.3 (AAR), with highest risk in the group aged <1 year (0.9 ASR). The diagnostic subgroup with highest incidence, however, was unspecified malignant tumors (0.2 AAR), predominantly in the group aged 15–19 years (0.4 ASR), while the group aged <1 year had higher risk of developing other specified malignant tumors (0.9 ASR).
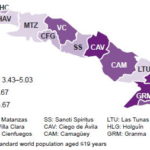
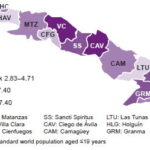
Geographic distribution of the three childhood cancer diagnostic groups with highest incidence—leukemias, lymphomas and CNS tumors—varied by sex. Overall risk among males aged ≤19 years was very high (AAR >24.94) in Ciego de Avila and Villa Clara Provinces and the Isle of Youth Special Municipality, and low (AAR <21.30) in Guantánamo, Granma, Cienfuegos and Havana Provinces (Figure 1). Among females in the same age group, risk was very high (AAR >26.41) in Sancti Spíritus, Villa Clara and Cienfuegos Provinces, and low (AAR <17.99) in Las Tunas, Havana and Guantánamo Provinces, and the Isle of Youth Special Municipality (Figure 2).
Incidence of leukemias in males was very high (AAR >8.27) in Villa Clara, Santiago de Cuba and the Isle of Youth, and low (AAR <4.87) in Las Tunas, Sancti Spíritus, Havana City and Pinar del Río (Figure 3). Among females, leukemia incidence was very high (AAR >5.67) in Granma, Holguín and Ciego de Avila, and low (AAR <3.42) in Havana, Matanzas, Las Tunas and the Isle of Youth (Figure 4).
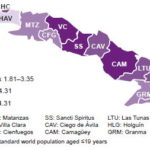
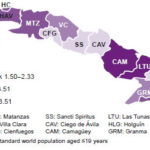
Lymphoma risk was very high for males (AAR >7.40) in Pinar del Río, Villa Clara and Ciego de Avila, and low (AAR <2.82) in Guantánamo, Las Tunas, Cienfuegos and Havana (Figure 5); for females, lymphoma risk was very high (AAR >4.31) in Camagüey, Sancti Spíritus and Villa Clara, and low (AAR <1.80) in Guantánamo, Havana, Pinar del Río and the Isle of Youth (Figure 6).
Risk of central nervous system tumors in males was very high (AAR >3.51) in Camagüey, Las Tunas and the Isle of Youth, and low (AAR <1.49) in Holguín, Ciego de Avila, Sancti Spíritus and Cienfuegos (Figure 7). In females, risk was very high (AAR >3.27) in Camagüey, Santiago de Cuba and Cienfuegos, and low (AAR <0.94) in Las Tunas, Havana, Pinar del Río and the Isle of Youth (Figure 8).
Figure 1: Geographic Distribution of Childhood Cancer Incidence in Cuban Males, 2001 to 2003

Figure 2: Geographic Distribution of Childhood Cancer Incidence in Cuban Females, 2001 to 2003

Figure 3: Geographic Distribution of Leukemia Incidence in Cuban Males Aged ≤19 Years, 2001 to 2003

Figure 4: Geographic Distribution of Leukemia Incidence in Cuban Females Aged ≤19 Years, 2001 to 2003
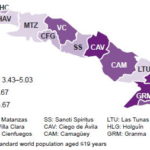
Figure 5: Geographic Distribution of Lymphoma and Reticuloendothelial Neoplasm Incidence in Cuban Males Aged ≤19 Years, 2001 to 2003
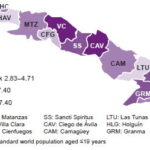
Figure 6: Geographic Distribution of Lymphoma and Reticuloendothelial Neoplasm Incidence in Cuban Females Aged ≤19 Years, 2001 to 2003
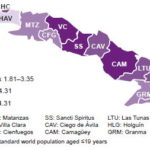
Figure 7: Geographic Distribution of CNS Tumor Incidence in Cuban Males Aged ≤19 Years, 2001 to 2003
DISCUSSION
The proportion of childhood cancer to total cancer found in this study is within the 1%–2% range considered normal internationally,[8,15] and incidence rates, overall and by diagnostic group, are similar to those reported in the international literature.[16–28] According to the International Agency for Research on Cancer (IARC), annual incidence worldwide is 100–150 per million population aged ≤19 years with rates in Europe varying between 109 per million in England, 137 per million in France, 141 per million in Italy, 138 per million in Denmark. In Latin America, incidence is 91–106 per million aged <15 years.[8] In the United States 8700 cases are reported annually in children aged <15 years and 12,400 cases in children and adolescents aged <20 years, equivalent to annual rates of 134 per million population aged <15 years and 149 per million population aged <20 years.[9] In some developing countries, rates as low as 45 per million population aged <15 years have been recorded, suggesting significant underreporting.[8]
Rates in Cuba differed from those reported internationally only in three diagnostic subgroups. Predominance of renal carcinomas has been reported internationally in the group aged 15–19 years,[8,9] while in this study, incidence was very low, and the only cases registered were in the group aged 1–4 years. Other authors have reported that incidence of soft tissue sarcomas is highest in children aged <10 years with peaks at age 3–6 years for rhabdomyosarcoma and 15–19 years for other specified soft tissue sarcomas.[6,10,29] These subgroups had highest incidence in Cuba, but predominantly in the group aged <1 year.
The three diagnostic groups found to have highest incidence in Cuba correspond to the three most frequent childhood cancers worldwide,[1,30] and the order of frequency—leukemias first, lymphomas second, and CNS tumors third—matches the pattern most commonly found in Latin America.[6,8] Incidence patterns differ in other geographic regions, notably Europe and the United States, and Africa. In the former regions, leukemias are most common, followed by CNS tumors and lymphomas. In the United States, for example, these three diagnostic groups account for 63% of all cancers reported in children aged <15 years, in the following order: leukemias 30.2%, CNS tumors 21.7%, and lymphomas 10.9%.[9] In Africa, however, lymphomas are the primary diagnostic group.[8]
Geographical and ethnic variations in childhood cancer incidence may be an expression of environmental risks or genetic factors, although family aggregation explains a very small number of cases. Such differences stand out in CNS tumors, which range from 10–40 cases per million population aged <15 years, appearing much more frequently in whites and in high socioeconomically developed countries (especially in the Nordic European countries and the United States) than in blacks (in the United States and other developed countries), Asians, Hispanics, Africans, and in developing countries. Although risk factors to explain these differences have yet to be determined, it has been suggested that higher incidence of CNS tumors in developed countries is chiefly due to availability of more advanced diagnostic methods, whereas detection of these tumors is much lower in developing countries lacking diagnostic capacity.[1,31] Other variables, such as co-morbidity, variations in disease classification, and uncertainty about the reference population, may influence data quality in different geographic locations.[5,6,8,10,29,31]
Describing incidence of childhood cancer by skin color was not an objective of the present study because it was not reported with 2001–2003 data. This fact and differences found in childhood cancer risk in different parts of the country point to the need for more sociodemographic and biological research examining possible risk factors in order to develop adequate prevention strategies. A thorough analysis of cancer incidence and mortality trends in the Cuban population aged ≤19 years is recommended.