INTRODUCTION
The physical changes accompanying arrival of puberty and the beginning of adolescence can be disconcerting for these young people and the adults close to them. Adolescents are required to make a series of adjustments to function interpersonally and within their environment, adjustments modulated by the social and cultural milieu in which they develop. The vulnerability of adolescence is especially evident in the sphere of sexuality.[1–4]
Faced with issues of sexuality—including types of sexual activities or behaviors, recognizing love, avoiding unwanted pregnancies and defining sexual roles—adolescents may be exposed to substantial risks and dilemmas. Add to this that they often have insufficient information about sexuality, which can lead to using it as a mode of rebellion, unaware of the risks of pregnancy, sexual transmitted infections (STI) and other problems.[1–5] Thus, these youth need guidance and support for informed decision-making; and sex education that provides them with a better understanding of sexuality and facilitates adoption of health promoting behaviors.[3,4] All this applies to diabetic adolescents, complicated by their disease.
Diabetes mellitus (DM) is a chronic non-communicable disease that constitutes an important health problem because of its high disease burden, risk of comorbidities and mortality, and ensuing social and economic costs.[6] Type 1 DM onset is acute in children and adolescents and evolves rapidly; in this phase the often difficult treatment goal is to maintain the best possible metabolic control to enable normal growth and development, assisting patients to adopt a new lifestyle (behavioral change) that helps them take responsibility for their own DM management.[6] A combination of diet, medication, exercise and education can offer the prompt, active and effective approach needed to prevent or postpone complications, both acute and chronic, and improve prognosis and patient quality of life.[7–9]
Education is a mainstay of comprehensive DM management,[4] particularly among adolescents, as the disease can interfere with the profound physical and psychological changes during this period, affecting social relations and leading to psychosocial problems. The literature reports decreases in amputations and length of hospital stays, as well as marked improvement in glycemic control, among patients who have participated in educational programs.[10] This can be accomplished either one-on-one or in groups, and involve children or adolescents, their parents and broader social circles.
The educational process should begin at disease onset, reinforced in every medical appointment and hospital visit;[10,11] it should be adapted to DM’s natural course, providing basic information at onset that is expanded systematically over the lifespan. Like any other therapeutic tool, it should be organized and integrated into overall disease management. The team treating diabetics should receive appropriate training in educational methods and negotiate reasonable and attainable objectives with their patients. Periodic evaluation of these programs is essential.[11–13]
For diabetic adolescents, the focus should be on developments specific to this age group, including sexuality, as this is when responsibility for management progressively shifts to patients themselves. Thus, in addition to general DM education, risk of chronic complications from STIs should be addressed in educational programs. STIs present an even greater risk for diabetic adolescents than for their nondiabetic peers, because of the added problem of altered metabolic control.[14–16]
In 1995, 4% of reported STI cases (including HIV/AIDS) in Latin America occurred in adolescents.[17] Compared to the period 1980–2000, the first decade of this century has witnessed increases in reports of the number of people living with HIV/AIDS globally and in Cuba,[18,19] as well as in STIs generally.[18] In Cuba, the National Program for Prevention and Control of Sexually Transmitted Diseases and HIV/AIDS was established in 1986 with the main goal of preventing the infection–disease process from becoming a major population health problem.[19–22]
In light of the responsibility that diabetic adolescents have for progressively managing their disease and the real possibility of complications from illnesses typical of this age, such as STIs, our team undertook a sex education intervention with diabetic adolescents treated at the community-based Pediatric Specialty Polyclinic (PEPC, the Spanish acronym) in the city of Camagüey, capital of the province of the same name.
INTERVENTION
Objective Raise awareness about specific aspects of sex education and STIs among type 1 diabetic adolescents treated at the pediatric DM clinic of PEPC’s endocrinology service.
Justification In caring for diabetic adolescents, the authors have observed gaps in their knowledge of particular dangers presented by STIs. Diabetic adolescents’ increased risk from STIs makes guidance an essential part of their medical management.[14–16] Addressing the knowledge gap is therefore a major objective of our preventive efforts.
Participants A random sample of 20 adolescents (aged 12–19 years ) with type 1 DM of the 57 receiving treatment in PEPC’s pediatric DM clinic in 2012. The sample size was chosen because such interventions are more successful with small groups.[14] The adolescents were in junior high (grades 7–9) and high school (grades 10–12). They and their guardians provided written informed consent to participate in the educational program and its evaluation; the study was approved by the research ethics committee of the Eduardo Agramonte Piña Pediatric Clinical-Surgical Teaching Hospital.
Activities Like other intervention efforts, the program followed three well-defined steps: diagnosis, the intervention itself and evaluation.
Diagnosis A survey was applied (see Appendix) designed by the authors to identify participants’ sociodemographic characteristics and knowledge of sexuality and STIs. Questions covered age, sex, sexual experience, age at initiation of sexual relations, sources of information on sex, birth control and knowledge of STIs. The latter included concept (Q4 in Appendix), main STIs (Q5), risk behaviors (Q6), transmission routes (Q7), clinical signs (Q8), prevention (Q9, Q10), STI effects on DM (Q11), and what to do in the event of an STI (Q12). Each of the nine questions was assigned 10 points; the number of correct answers varied among questions, so the percentage for each was calculated and converted to the nearest whole point out of ten. The maximum number of possible points for the questionnaire was 90; overall knowledge was considered satisfactory if there were ≥70% correct responses (≥63 of 90 points).
Intervention The authors offered a course in the PEPC pediatric diabetes clinic over a six-week period ending in May 2012. There were six weekly one-hour sessions that included a workshop using productive teaching methodology and participatory techniques such as brainstorming.[23] The model also included a DM day camp (a week of day-long educational and recreational activities for young diabetics and their parents or guardians) in the Camagüey Diabetic Care Center.
Evaluation Three months after the intervention, the same questionnaire was again administered to measure knowledge acquisition. SPPS version 10.0 and Word Office XP were used to process data and compare pre- and post-intervention knowledge.
RESULTS
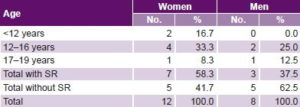
The 20 adolescents in the study included 12 women and 8 men; 7 women (58.3%) had initiated sexual relations—2 (16.7%) when they were aged <12 years—and 3 men (37.5%) (Table 1).
Table 1: Diabetic adolescents’ age at initiation of sexual relations (n = 20)
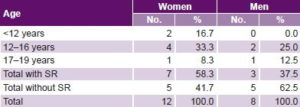
SR: sexual relations
Sources of information on sexuality in descending order of frequency were: school (65%), friends (50%), television (45%), family (40%), medical team (30%) and radio (15%).
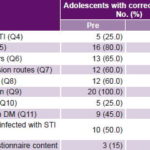
Before the intervention, only five adolescents (25%) demonstrated understanding of the concept of STIs (Q4), compared with 16 (80%) afterwards. Prior to the educational intervention, only two items elicited >70% correct responses. 16 (80%) were able to correctly identify STIs (Q5) from a list of diseases and 20 (100%) were able to identify which methods of birth control prevent STIs. Percentages of correct responses for other questions ranged from 25% to 65%. In contrast, following the intervention, at least 70% of adolescents gave correct responses to all questions, and 100% were able to correctly identify STIs (Table 2).
Table 2: Knowledge of STIs in diabetic adolescents pre- and post intervention (n = 20)
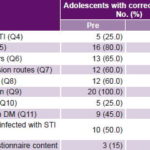
STI: sexually transmitted infection
Before the intervention, only 9 (45%) knew that STIs can cause acute DM complications (Q11), even though such effects can potentially be lethal. The number increased to 16 (80%) after the intervention (Table 2). Prior to the intervention only 3 (15%) adolescents scored ≥70% on the questionnaire; all participants scored ≥70% afterwards.
LESSONS LEARNED
There was substantial improvement, measurable at three months, in adolescents’ knowledge of sexual topics such as risk behaviors and how to prevent STIs, and even more important, how STIs can affect and complicate DM. The fact that before the intervention fewer than half were aware of their particular vulnerability to STIs underlines the need for systematic education in this patient group. The intervention—a course with participatory techniques for small groups of diabetic adolescents—proved useful in educating these patients about their health and provided them greater knowledge, favoring adoption of healthy behaviors. We recommend establishing systematic sex education interventions as part of DM education for type 1 diabetic adolescents, including those recently diagnosed.
APPENDIX
Sex Education for Diabetic Adolescents: Pre- and Postintervention Questionnaire |
|
Q1. Sex:
1.1__Male 1.2__Female
Q2. Grade__
Q3. General information
3.1 Do you know about sexually transmitted infections (STI) and HIV-AIDS?
Yes__ No__
3.2 Where do you get your information about them?
__radio __TV __school
__family __friends __medical team
3.3 (a) Have you had sexual relations? Yes__ No__ (age) ___
(b) Did you use birth control? Yes__ No__
3.4 Have you ever had an STI? Yes__ No
Which?_____________________
Q4. Mark True or False:
4.1__STIs are transmitted only through sexual contact.
4.2__STIs have other transmission routes.
4.3__STIs are those that are transmitted through sex games.
| Q5. Which of the following are STIs? (Mark True or False): |
| 5.1__Hepatitis B |
5.8 __Herpes simplex type 1 |
| 5.2__Common cold |
5.9 __Chickenpox |
| 5.3__Syphilis |
5.10__Genital warts |
| 5.4__Gonorrhea |
5.11__Intestinal parasites |
| 5.5__Leptospirosis |
5.12__Trichomonas |
| 5.6__HIV/AIDS |
5.13__Leprosy |
| 5.7__Chlamydia |
|
Q6. Mark an X beside all the following statements that are True:
6.1__Having multiple partners puts one at risk for contracting STIs.
6.2__Anal sex prevents STI infections.
6.3__Reducing the number of sexual partners reduces risk of contracting STIs.
6.4__Monogamy ensures safer sex.
6.5__Casual sexual encounters increase the risk of contracting STIs.
6.6__Everyone who has unprotected sexual relations is at risk of contracting STIs.
Q7. Mark an X beside the ways STIs can be contracted:
7.1__Contact with your partner’s personal objects
7.2__Penetration of the penis in the vagina
7.3__Anal coitus
7.4__Kisses, sweat, saliva or tears from infected individuals
7.5__Pregnancy (mother to fetus before or during birth)
7.6__Blood transfusions
7.7__Insect bites
Q8. Mark True or False:
8.1 __Secretion is an important clinical manifestation of
gonorrhea in men.
|
8.2 __Syphilis begins with a genital sore.
8.3 __A baby can be born with an STI.
8.4 __Some STIs are asymptomatic in women.
8.5 __Syphilis affects only the genital organs.
8.6 __HIV/AIDS is almost always associated with skin sores.
8.7 __A wart in the genital area makes us suspect an STI.
8.8__Warning signs of STIs include secretions from the penis or
vagina, sores, and warts or peeling skin around the anus,
vagina or mouth.
Q9. Mark an X beside all the following that are ways to prevent STIs:
9.1__Sexual relations without exchange of saliva, secretions or
genital contact
9.2__Oral birth control
9.3__Condoms
9.4__Diaphragm
9.5__Abstention from sexual relations
9.6__Rhythm method
Q10. Mark an X beside all the following statements that are True:
10.1__Birth control methods provide safer sex.
10.2__Birth control methods are those that are used to prevent pregnancies.
10.3__Selecting a couple’s birth control method is a decision made by a single partner.
10.4__The ideal birth control method should be inexpensive, easy to use and free of side effects.
10.5__IUDs always cause infections and bleeding in women.
10.6__Condoms protect against STIs and help prevent pregnancy.
Q11. Mark True or False:
11.1__STIs do not affect control of type 1 diabetes mellitus.
11.2__STIs cause acute complications such as hyperglycemia.
11.3__STIs do not aggravate the chronic complications of diabetes mellitus.
Q12. If you contracted a sexually transmitted infection, what would you do first? (Mark with an X):
12.1__Begin antibiotic treatment
12.2__Consult your partner
12.3__Use birth control
12.4__Consult your medical team
12.5__Abstain from sexual relations
12.6__Consult your parents
12.7__Consult your best friend
| Scoring guide |
| Item |
Correct response |
| 4 |
4.2 |
| 5 |
5.1, .3, .4, .6, .7, .10, .12 |
| 6 |
6.1, .3, .4, .5, .6 |
| 7 |
7.2, .3, .5, .6 |
| 8 |
8.1, .2, .3, .4, .6, .8 |
| 9 |
9.1. .3, .4, .5 |
| 10 |
10.1. .2, .4, .6 |
| 11 |
11.2 |
| 12 |
12.4 |
|