ABSTRACT
Introduction In recent years, several reports have appeared in the international literature concerning evolution and prognosis for obstetric patients whose illnesses have led to admission to intensive care units (ICUs). The term severe maternal morbidity has been proposed to refer to life-threatening complications that occur during pregnancy, delivery or postpartum.
Objective Characterize severe maternal morbidity in obstetric patients admitted to the ICU of the Enrique Cabrera General Teaching Hospital in Havana from 1998 to 2004.
Methods From 1998 to 2004, we conducted a prospective, descriptive, and observational study of 312 patients admitted to the ICU of the Enrique Cabrera General Teaching Hospital in Havana, Cuba. Patients were included whose length of stay was >24 hours, and whose family members provided written informed consent. A data collection form was developed to record general characteristics, personal and family medical history, cause of ICU admission, diagnosis, obstetric condition at the onset of illness and at admission, pregnancy outcome, surgeries performed and patient’s ICU discharge status (survivor or non-survivor), the latter a dependent variable. An Excel database was compiled and processed using SPSS 13.0. Percentages were used to summarize qualitative variables. A Chi-square test was used for univariate analysis between these qualitative variables and patient discharge status; t-test was used for quantitative analyses. Results Overall mortality in the cohort was 7.4% (23 patients), greater among women aged <20 years, those with a history of previous illnesses, and those subjected to several surgical interventions. Obstetric hemorrhage, pre-eclampsia/eclampsia, and postpartum sepsis were the most commonly diagnosed obstetric disorders. Non-obstetric disorders diagnosed included severe asthma, pneumonia and peritonitis. Amniotic fluid embolism, postpartum sepsis, early postpartum hemorrhage and pre-eclampsia/eclampsia were associated with the highest hospital case fatality rates in women with obstetric disorders; while acute chest syndrome, promyelocytic leukemia and pulmonary embolism were associated with the highest hospital case fatality rates among women with non-obstetric disorders.
Conclusions Our results concur with most of those published on severe maternal morbidity in ICUs, including a high incidence of hemorrhagic disorders, pre-eclampsia and postpartum sepsis. The number of patients with hematological disorders accounts for the difference between the results of our study and others concerning morbidity and mortality among this patient group. A significant correlation was observed between history of previous illnesses and patient discharge status. Prognosis was worse for patients subjected to several surgical interventions, which can be attributed to the higher risk of complications and the severity of the underlying illness.
Keywords Maternal mortality, maternal morbidity, intensive care, critical care, postpartum hemorrhage, pre-eclampsia, eclampsia, postpartum sepsis
INTRODUCTION
In recent years, several reports have appeared in the international literature concerning the evolution and prognosis of illnesses leading to admission of pregnant and postpartum women in intensive care units (ICUs). Acute respiratory failure, hypertensive disorders of pregnancy, infections, disseminated intravascular coagulation (DIC), hemodynamic instability due to hypovolemic shock and acute renal insufficiency, among others, are the most common causes for obstetric and postpartum patient ICU admission.[1-37] These illnesses can produce sequential organ failure leading to multiple organ dysfunction syndrome (MODS), associated with high mortality.
In this context, the term severe maternal morbidity has been proposed to refer to complications occurring during pregnancy, delivery, or postpartum, which may be life-threatening without adequate medical attention.[7,34-37] Included in this category are all women admitted to ICUs during pregnancy or postpartum that require intensive life-saving treatment.[34]
The main objective of ICU admission for pregnant or postpartum women is to minimize the associated risk of morbidity and mortality for both the mother and the child.[31-41] It is essential that medical teams responsible for these women’s care be familiar with the multiple illnesses that interfere with physiological adaptations during pregnancy and postpartum, as well as their influence on underlying diseases.[40,41]
Maternal mortality is considered an important indicator for measuring the socioeconomic level and health status of a country’s population. But more than its relevance as a statistic, a maternal death dramatically affects the stability of both her family and community.[31-33,39,42-44] In 1994, Lewinsohn et al.[1] published the results of a study conducted on 58 patients, with a mortality rate of 10.5%. Two years later, el-Solh and Grant,[2] in a study of 93 women in New York, reported a maternal mortality rate of 10.8%, similar to findings by Bhagwanjee et al.[3] in South Africa (10.5%). Also in South Africa, Taylor and Richards[4] published a study of 61 critical patients hospitalized between 1985 and 1996, with notably high mortality (38%). Olarra,[10] reported a mortality of 7.5% among 149 patients hospitalized over seven years in Spain, while Afessa[9] observed mortality of only 2.7%, which was considered very low by Olarra in a comparative analysis.[10] Later, a five-year study by Cheng and Raman[13] on post-surgical postpartum women, found mortality at a low 4.7%. In a six-year study in Mexico, Estrada Altamirano et al.[12] reported a maternal mortality rate of 7.34%.
Results published from studies of ICU obstetric patients in various developing countries between 2003 and 2004 showed dissimilar results. Demirkiran et al.[14] in Istanbul, Turkey, reported 13 deaths (10.4%) in a series of 125 patients. Okafor and Aniebue[16] in Nigeria observed a mortality rate of 33.3%, while Karnad et al.[17] in Mumbai, India, published a 21.6% mortality rate from their study. These results indicate a wide range in ICU mate rnal mortality, reflecting varying access to medical services and other characteristics of each region.
In 2005, Munnur et al.[25] published an interesting paper comparing two teaching hospitals, one in India and the other in the United States. The authors reported a significantly higher mortality rate among Indian patients (25.0%) when compared to US patients (2.3%).The authors suggested this result is a reflection of the socio-economic disparities between the two countries. Oladapo et al.[26] in Nigeria reported the death of 17.3% of their cases, while Al-Suleiman et al.[27] in Saudi Arabia reported a mortality rate of only 9.4%.
For Cuba, the Health Statistics Yearbook[45] indicates that in 2004 direct maternal mortality (per 100,000 live births) was 21.2; the indirect rate was 17.3; and the overall rate was 38.5. Urbay Ruiz[30] reported a mortality rate of 6.5% (11.4% among adolescents) in a nine-year study of 275 obstetric patients admitted to the ICU of the Arnaldo Milian Castro Provincial Teaching Hospital in Villa Clara Province.
The objective of this article is to describe severe maternal morbidity in the ICU at the Enrique Cabrera General Teaching Hospital of Havana , Cuba, from January 199 8 to December 2004.
MATERIALS AND METHODS
Cohort: Our study included 312 obstetric patie nts ad mitted to Havana’s Enrique Cabrera General Teaching Hospital ICU from January 1, 1998 through December 31, 2004. Patients were included whose length of stay in ICU was >24 hours, and who were not transferred to another hospital or facility.
Hospital: The Enrique Cabrera General Teaching Hospital is a 512-bed urban facility located in the Havana municipality of Boyeros. The National Hematology and Immunology Institute is a lso located in the hospital. The ICU is a multi-purpose unit with 17 beds. One of its distinctive features is that it receives patients with hema tological illnesses referred from other parts of the country. Th ere are also two wards for coronary and stroke patients.
Type of Study: This is a prospective, descriptive, and observational cohort study. The research was approved by the Scientific Council and the Research Ethics Committee of the Enrique Cabrera Medical School. Due to the critical con dition of the patients admitted to the ICU, written informed consent was obtained from each patient’s next-of-kin for inclusion in the study.
Data Collection and Processing: General patient information was recorded on a data collection form: medical history, reason for admission , diagnosis on arrival and final diagnosis, obstetric status at the time of illness and at time of ICU admission, outcome of pregnancy, and surgical interventions. Patient status at discharge from the ICU (survivor or non-survivor) was also recorded and considered a dependent variable. Information was collected daily on each patient, updated with information from the patient’s chart and from daily case discussions by the medical team and the commission in charge of critically ill obstetric patients. Causes of death were grouped according to the International Classification of Diseases (ICD).[46]
An Excel database was developed, and data was processed with the SPSS 13.0 system for Windows. Percentages were used to summarize qualitative variables. The Chi-square test was used for univariate analysis of qualitative variables related to patient discharge status; and the t-test was used for quantitative variables. In each case, a value of p<0.05 was considered significant. The results were plotted in a figure and tables.
RESULTS
Over the 7-year study, of the 312 patients who met the inclusion criteria referenced above, 289 survived (92.6%), while 23 died (7.4%) (Figure 1).
Figure 1: ICU Maternal Mortality, Enrique Cabrera General Teaching Hospital, January 1998 to December 2004 Source: Data collection form, Enrique Cabrera General Teaching Hospital. Peer Reviewed

Source: Data collection form, Enrique Cabrera General Teaching Hospital.
Table 1: Obstetric ICU Patients: Socio-demographic Characteristics, Length of Stay and Discharge Status, 1998-2004

* Figures based on total number of patients; (x): mean; SD: Standard deviation; CI 95%: 95% confidence interval. Source: Data collection form, Enrique Cabrera General Teaching Hospital.
An analysis of patients’ socio-demographic characteristics (Table 1) reveals that the mean age of surviving patients was 27.8 ± 6.5, and that of deceased patients slightly higher at 28.7 ± 7.2.
Analysis of age distribution showed that the largest group of patients were those aged 30-34 years (77 patients); however, the highest mortality rate was observed in women aged <20 years (13.5%), followed by those aged =35 years (11.1%), and the lowest mortality was found in women aged 20-24 years (2.8%).
Among the 136 women of color, mortality was only slightly higher (8.1%) than for the 176 white patients (6.8%), a difference that did not prove statistically significant (x 2 =0.043; p=0.8439). The mean number of previous pregnancies was slightly higher among deceased patients at 2.56 (95% CI 1.97-3.16) than for those who survived at 2.10 (95% CI 1.96-2.27). Finally, length of stay was longer for those patients who died than for those who survived, and a 5.3-day mean length of stay for all patients was recorded.
The three most frequently reported pre-existing illnesses among all patients (Table 2) were bronchial asthma, sickle cell disease, and hypertension, accounting together for over two-thirds of the illnesses described. Twelve patients had other illnesses, which were grouped under “other”, since the number was not significant, and these cases were not associated with a negative prognosis. There was a strong association between mortality and illnesses such as myelocytic leukemia, hypertension, diabetes mellitus, and sickle cell disease.
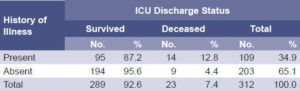
Analysis of pre-existing illnesses associated with ICU discharge status (Table 3) reveals that 14 patients with such illnesses died (12.8%) while only nine died (4.4%) in the group reporting no prior illnesses (x 2 : 7.347; p=0.007). A total of 34.9% of the patients referred to a personal history of chronic disease.
Table 2: Pre-existing Illnesses and Patient ICU Discharge Status, 1998-2004

Source: Data collection form, Enrique Cabrera General Teaching Hospital.
Table 3: History of Illness and Patient ICU Discharge Status, 1998-2004
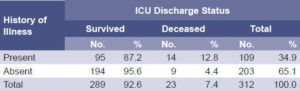
x2: 7.347 (p = 0.007). Source: Data collection form, Enrique Cabrera General Teaching Hospital.
Of the 312 patients studied, 143 were pregnant at the onset of illness, and 169 were postpartum (Table 4). Although mortality was somewhat higher in the latter group when compared to the first (8.9% and 5.6%, respectively), there was not a strong statistical association between the obstetric status at the onset of the illness and patient discharge status.
The same results were observed in patients admitted to the ICU, where the mortality rate among postpartum patients was much higher than that of pregnant patients (8.7% and 3.7%, respectively). However, no statistical association was demonstrated between obstetric status upon admission to the ICU and patient discharge status.
Table 4: Obstetric Status and Patient ICU Discharge Status, 1998-2004.
* x2 = 1.245 (p = 0.264; NS). † x2 = 2.461 (p = 0.117; NS) NS: Not significant. Source: Data collection form, Enrique Cabrera General Teaching Hospital.
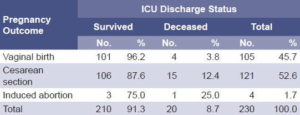
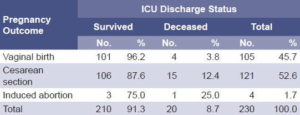
Most pregnancies (52.6%) of the 230 postpartum patients admitted to the ICU ended with cesarean sections (Table 5), with a higher mortality rate than those women who delivered vaginally. The percentage of deceased patients whose pregnancies were terminated by induced abortion was also high, although the number of cases in this category was small.
Table 5: Pregnancy Outcome and Patient ICU Discharge Status, 1998-2004

Source: Data collection form, Enrique Cabrera General Teaching Hospital.
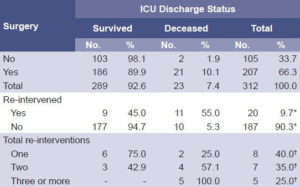
Nearly two-thirds of the patients underwent major surgery (Table 6), with a marked difference in patient discharge status compared to those who underwent no surgery: 10.1% of the surgical patients died, compared to 1.9% of non-surgical patients. Noteworthy is the fact that the prognosis for patients who underwent multiple interventions was worse: the 25.0% mortality rate for those patients re-intervened twice, and 100.0% for those re-intervened three times or more.
Table 6: Surgical Interventions and Patient ICU Discharge Status, 1998-2004
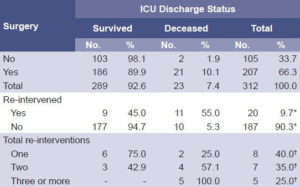
* Figures based on 207 surgical cases. † 20 re-interventions were considered. Source: Data collection form, Enrique Cabrera General Teaching Hospital.
In this study, diagnoses of illnesses that prompted ICU admission were classified in two groups: obstetric and non-obstetric causes. As noted in Table 7, the most commonly diagnosed illnesses were early obstetric hemorrhage, pre-eclampsia/ eclampsia, and postpartum sepsis. Antepartum and late post-partum hemorrhage were the next most commonly diagnosed conditions, indicating the importance of hemorrhagic disorders in this sample.
Table 7: Obstetric Disorders and ICU Patient Discharge Status

* Figures based on total number of patients. PI: Post-intervention. Source: Data collection form, Enrique Cabrera General Teaching Hospital.
Early postpartum hemorrhage was reported in 11.1% of deceased patients, 7.7% among those with postpartum sepsis, and 4.8% in those with pre-eclampsia/eclampsia. Amniotic fluid embolism was observed in two patients, one of whom died.
Non-obstetric illnesses observed in patients (Table 8) included 10.3% diagnosed with severe asthma (6.3% deceased), 9.6% with community-acquired pneumonia (CAP), and 6.7% with acute peritonitis (23.8% deceased).
Table 8: Non-Obstetric Disorders and Patient ICU Discharge Status

* Includes one patient with postpartum sepsis and one with hemorrhage, also considered in Table 7. † Figures based on total number of patients. ‡ Includes 15 patients with sickle cell disease complications. Source: Data collection form, Enrique Cabrera General Teaching Hospital.
High case fatality was observed from acute promyelocytic leukemia and pulmonary embolism. In both cases, two of five patients died (40.0%). As shown in Tables 7 and 8, two main diagnoses were ascertained in 13 surviving patients and in 4 deceased patients.
None of the patients with community-acquired pneumonia died, although this was the second major non-obstetric illness observed in these patients (30 cases).
It is noteworthy first, that sickle cell disease was observed in 4.8% of patients included in the study (13.3% deceased). Second , that although vasoocclusive and hepatic crises were diagnosed in 46.7% and in 33 .3 % of sickle-cell patients, none of these patients died . Finally, althoug hacute chest syndrome (ACS) was detected in only three patients (20.0% of sickle-cell patients), its prognosis was poor, as two thirds o f ACS patients died.
DISCUSSION
Results of published studies on maternal mortality in intensive care units vary greatly, depending on location, socio-economic development, type of patients included and specific characteristics of the unit.
Several articles refer to the age of ICU obstetric patients, which varies according to location, socio-economic development, and characteristics of the study. However, few reports have linked age with patient prognosis. Bhagwanjee et al.[3] observed no differences between surviving and deceased patients, while Urbay Ruiz et al.[30] reported a worse prognosis for patients aged <20 years (11.4% deceased). In their seminal study, Waterstone et al.[7] found that age >34 years was an independent predictor for maternal mortality in obstetric ICU patients. It is noteworthy that in general, a worse prognosis has been described for adolescents and patients aged >35 years,[7,28,29,31,39] a finding corroborated in our study.
Our study showed no significant association between skin color and ICU patient discharge status. The small difference observed corresponds with the ICU’s particular characteristics, which during this period admitted a relatively large number of patients with sickle cell disease, with a case fatality rate superior to the series’ mean, a finding addressed below. Only Waterstone et al.[7] observed a worse prognosis for women of color, which they attributed to the lower socio-economic conditions of this group in the United Kingdom.
Pre-existing illness was a significant variable in the univariate analysis. Association of mortality with disorders such as myeloid leukemia, hypertension, diabetes mellitus and sickle cell disease was considerable, as has been previously recognized. [3,7,17,18,28] Also of interest was the association between obstetric status (pregnant or postpartum) and ICU discharge status. Evaluated both at onset of illness and at admission, postpartum patients had higher mortality than those who were pregnant. However, analysis showed no significant association between patient obstetric status and ICU discharge status.
We believe a number of factors may explain the worse prognosis for surgical patients. These include hemorrhage, hemodynamic alterations (low blood pressure and shock), embolic phenomena, anesthetic risk, bronchoaspiration, respiratory depression, drug toxicity, and common post-operative complications. It has been suggested that these patients may suffer surgical complications due to arterial hypoxemia during manipulation of the airways, and that contributing to maternal mortality may also be pregnancy-related changes (decrease in residual functional capacity, increase in oxygen consumption, oral/pharyngeal edema), which expose obstetric patients to the risk of reduced arterial oxygen saturation during episodes of apnea or hyperventilation. [47] Severity of the illness that prompted a cesarean section or other surgical intervention may be another contributing factor. Moreover, a greater number of surgical re-interventions introduces greater risk of complications. At the same time, the severity of illness requiring re-intervention may itself be associated with a worse prognosis.[47]
Postpartum hemorrhage and pre-eclampsia/eclampsia syndrome are recognized as the most common illnesses leading to ICU admission for obstetric patients, which coincides with our own findings, in which postpartum sepsis was the third most common obstetric diagnosis. In Hazelgrove’s series,[6] pregnancy-related or -induced hypertension was observed in 39.5% of the patients, followed, in order, by postpartum hemorrhage in 33.3%. Quah’s report[8] indicates that pre-eclampsia/eclampsia was present in 50.0% of cases, followed by hemorrhage (24.0%) and respiratory insufficiency (10.0%). Estrada Altamirano et al.[12] observed that the most frequent illnesses were pregnancy-induced hypertension (53.8%), hypovolemic shock (10.2%) and critical heart disease.
It is important to note that Afessa et al.[9] reported respiratory insufficiency, followed by pre-eclampsia and HELLP syndrome (hemolysis, elevated liver enzymes and low platelet count) as the most commonly diagnosed disorders in their study, while Olarra et al.[10] reported pregnancy-related hypertension in half their cases. Postpartum hemorrhage followed in order by pre-eclampsia/eclampsia were reported as the most commonly diagnosed disorders in the ICU in a number of articles,[7, 11, 13, 21] while in others, the reverse was observed: preeclampsia/ eclampsia was most frequent, followed by postpartum hemorrhage. [5,6,8,10,14,16,18,30]
In Cuban national studies, Rodriguez Iglesias et al.[29] reported postpartum post-cesarean sepsis and hemorrhage as the most common disorders, each observed in 33.3% of cases. Postpartum sepsis and eclampsia were reported in 16.6% and 8.3%, respectively. While Urbay et al.[30] observed pre-eclampsia in 22.9% of patients admitted, postpartum sepsis was the second most commonly diagnosed illness at 22.5%, which is striking.
Reviewing mortality from these conditions in our study, the largest number of case fatalities was observed in patients with postpartum hemorrhage, followed by those with pre-eclampsia/eclampsia and postpartum sepsis. Patients with amniotic fluid embolism presented a poor prognosis since death resulted in half the patients, although the number of women with this diagnosis (2) was quite low. Nevertheless, it is considered a catastrophic condition that occurs during delivery,[48,49] with an incidence of between 1 in 8000 and 1 in 80,000 cases and a very high case fatality rate, reaching over 50%.
In Okafor and Aniebue,[16] the case fatality rates were significantly high for postpartum hemorrhage patients (50.0%) and preeclampsia/eclampsia patients (44.0%). The authors attribute this result to the bad social and economic situation of a poor African country such as Nigeria, with insufficient prenatal care and nutrition levels. Conversely, Harrison’s study[21] in the United Kingdom reported mortality rates of 3.5% among eclampsia patients, 2.6% among pre-eclampsia patients, only 0.6% in patients with postpartum hemorrhage. In another Cuban study, Urbay et al.[30] observed a 6.5% case fatality rate among postpartum sepsis patients and a 3.2% mortality rate in pre-eclampsia patients.
In Mexico, Briones Garduño et al.[18] reported that the pre-eclampsia/eclampsia syndrome was the main cause of death (37.6% of all deceased patients), followed by postpartum hemorrhage (16.6%) and sepsis (9.7%).
Obstetric patients are also admitted to ICUs for non-obstetric conditions, which in many cases are extremely serious and related to patient ICU discharge status. In this study, the main reasons for these admissions were, in order, severe asthma, community-acquired pneumonia (CAP) and acute peritonitis. However, poor prognosis was most associated with acute chest syndrome, sickle cell anemia, acute promyelocytic leukemia, pulmonary embolism and acute peritonitis due to different causes.
It should be noted that the large number of sickle cell cases observed in this study is related to the characteristics of the unit, with patients referred from the National Institute of Hematology located in the same hospital. Although vaso-occlusive and hepatic crises were observed in 46.7% and 33.3%, respectively, of sickle cell cases, all such patients survived. Patients with ACS had a poor prognosis since two thirds of these cases resulted in death, findings coinciding with the published literature, which notes the presence of pulmonary complications, mainly ACS, as a fundamental determining factor in the survival of obstetric sickle cell patients. These patients are more prone to develop complications with a poor prognosis, as we have also observed in our study.[50]
In the literature consulted, however, reporting on such non-obstetric conditions was rare. According to Munnur et al.,[25] findings related to these conditions differ according to socio-economic level and development of health care for pregnant and postpartum women. Consequently, malaria, viral hepatitis, venous thrombosis and poisoning, in that order, were the most diagnosed illnesses in India; whereas in the United States, the most frequently diagnosed illnesses, after placental anomalies, were myocarditis, sepsis, and drug abuse.[25]
The main cause of death observed in the Estrada Altamirano series in Mexico[12] was secondary complications of critical cardiopathies (40.9%), followed by irreversible hypovolemic shock (22.7%). Furthermore, despite the fact that pregnancy-induced hypertension was the most frequently observed disorder, it was only the third cause of death (18.1%). These results vary significantly from the findings of our study.
CONCLUSIONS
The most commonly diagnosed obstetric disorders in the ICU were early postpartum hemorrhage, pre-eclampsia/eclampsia syndrome, and postpartum sepsis, findings which concur with those of most published studies on this question. A severe asthmatic state, pneumonia and peritonitis were the most commonly diagnosed non-obstetric disorders.
Highest case fatality was observed among patients with obstetric disorders associated with amniotic fluid embolism, postpartum sepsis, early postpartum hemorrhage, and pre-eclampsia/eclampsia syndrome. Among patients with non-obstetric illnesses, ACS, promyelocytic leukemia and pulmonary embolism provoked the highest case fatality. Our ICU is the national reference center for pregnant and postpartum patients with hematological disorders, and is located in the same hospital as the Institute of Hematology and Immunology, facilitating comprehensive and multidisciplinary care for patients referred from all over the country. We believe that this is the chief aspect in which our study differs from others conducted on the incidence and case fatality rates for ACS and leukemia.
We found significant association between pre-existing illnesses and patient ICU discharge status; and patients undergoing several surgical interventions had a worse prognosis, which in our view may result from greater risk of complications and the severity of the underlying illness.
The main limitation of this study is that it was conducted in only one ICU of the country’s capital, and where a significant number of cases with hematological illness are admitted. Consequently, the authors believe that, taking in account the strengths of our national health system, a national multi-center study of severe maternal morbidity is warranted involving ICUs in various institutions throughout the country.
We recommend that the study’s results be made available to health authorities to inform development of relevant health policies, as well as decision-making that contributes to a substantial decrease in the incidence of such cases.
References

- Lewinsohn G, Herman A, Leonov Y, Klinowski E. Critically ill obstetrical patients: outcome and predictability. Crit Care Med. 1994;22(9):1412-4.
- el-Solh AA, Grant BJ. A comparison of severity scoring systems for critically ill obstetric patients. Chest. 1996;110(5):1299-304.
- Bhagwanjee S, Paruk F, Moodley J, Muckart DJ. Intensive care unit morbidity and mortality from eclampsia: an evaluation of the Acute Physiology and Chronic Health Evaluation II Score and the Glasgow Coma Scale Score. Crit Care Med. 2000;28(1):120-4.
- Taylor R, Richards GA. Critically ill obstetric and gynaec ological patients in the intensive care unit. S Afr Med J. 2000;90(11):1140-4.
- Cohen J, Singer P, Kogan A, Hod M, Bar J. Course and outcome of obstetric patients in a general intensive care unit. Acta Obstet Gyne- col Scand. 2000;79(10):846-50.
- Hazelgrove JF, Price C, Pappachan VJ, Smith GB. Multicenter study of obstetric admissions to 14 intensive care units in Southern England. Crit Care Med. 2001;29(4):770-5.
- Waterstone M, Bewley S, Wolfe C. Incidence and predictors of severe obstetric morbidity: case-control study. BMJ. 2001;322:1089-94.
- Quah TC, Chiu JW, Tan KH, Yeo SW, Tan HM. Obstetric admissions to the intensive therapy unit of a tertiary care institution. Ann Acad Med Singapore. 2001;30(3):250-3.
- Afessa B, Green B, Delke I, Koch K. Systemic Inflammatory response syndrome, organ failure and outcome in critically ill obstetric patients treated in an ICU. Chest. 2001;120(40):1271-7.
- Olarra J, Longarela AM, Suárez L, Palacio FJ. Critically ill obstetric patients treated in an ICU. Chest. 2002;121:2077.
- Heinonen S, Tyrväinen E, Saarikoski S, Ruokonen E. Need for maternal critical care in obstetrics: a population-based analysis. Int J Obstet Anesth. 2002;11(4):260-4.
- Estrada Altamirano A, Hernández Pacheco JA, Cisneros Castelo M, Quesnel García C. Experiencia de la unidad de cuidados intensivos obstétricos del Instituto Nacional de Perinatología, 1993- 1998. Perinatol Reprod Hum. 2002;16(2):88-95.
- Cheng C, Raman S. Intensive care use by critically ill obstetric patients: a five year review. Int J Obstet Anesth. 2003;12 (2):89-92.
- Demirkiran O, Dikmen Y, Utku T, Urkmez S. Critically ill obstetric patients in the intensive care unit. Int J Obstet Anesth. 2003;12:266-70.
- Gilbert TT, Smulian JC, Martin AA, Ananth CV, Scorza W, Scardella AT. Obstetric admissions to the intensive care unit: outcomes and severity of illness. Obstetric Gynecol. 2003;102:897-903.
- Okafor UV, Aniebue U. Admission pattern and outcome in critical care obstetric patients. Int J Obstet Anesth. 2004;13(3):164-6.
- Karnad DR, Lapsiam V, Krishnan A, Salvi VS. Prognostic factors in obstetric patients admitted to an Indian intensive care unit. Crit Care Med. 2004;32:1418-9.
- Briones Garduño JC, Díaz de León Ponce M, Gómez Bravo Topete E, Ávila Esquivel F, Rodríguez Roldón M, Briones Vegas CG. Mortalidad materna y medicina crítica. Tres décadas (1973-2003). Rev Asoc Mex Med Crit y Ter Int. 2004;18:118-22.
- Anwari JS, Butt AA, Al-Dar MA. Obstetric admissions to the intensive care unit. Saudi Med J. 2004;25(10):1394-9.
- Braga Viggiano M, Guillermo Campos VM, de Souza E, Camano L. Necessidade de cuidados intensivos en maternidade pública terciaria. Rev Bras Ginecol Obstet. 2004;26(4):317-23.
- Harrison DA, Penny JA, Yentis SM, Fayek S, Brady AR. Case mix, outcome and activity for obstetric admissions to adult, general critical care units: a secondary analysis of the ICNARC Case Mix Programme Database. Crit Care. 2005;9(Suppl 3):S25-S37.
- Martins Bezerra EH, Alencar Junio CA, Goncalves Feitosa RF, Alves de Carvalho AA. Mortalidade materna-escola. Rev Bras Ginecol Obstet. 2005;27(9):548-53.
- Dias de Souza JD, Guiherme Cecatti J, Angela Parpinelli A. Factores asociados a gravidade da morbidade materna na caracterizacao de near miss. Rev Bras Ginecol Obstet. 2005;27(4):197- 203.
- Peracali JC, Parpinelli MA. S�ndrome hipertensivas da gestacao: identificacao da casos graves. Rev Bras Ginecol Obstet. 2005;27(10):627-34.
- Munnur U, Karnad DR, Bandi VDP, Lapsia V, Suresh MS, Ramshesh P, et al. Critically ill obstetric patients in an American and an Indian public hospital: comparison of case-mix, organ dysfunction, intensive care, and outcomes. Intensive Care Med. 2005;31:1087-94.
- Oladapo OT, Lamina MA, Fakoya TA. Maternal deaths in Sagamu in the new millennium: a facility-based retrospective analysis. BMC Pregnancy Childbirth. [online series]. 2006 [Cited 10 May 2007]. 6:6. Available from: http://www. biomed_central.com/1471-2393/6/6. Consulted: 3 May, 2008.
- Al-Suleiman SA, Qutub HO, Rahman J, Rahman MS. Obstetric admissions to the intensive care unit: a 12-year review. Arch Gynecol Obstet. 2006;274:4-8.
- Fuentes García AR, Pagés Mesa D, Hernández Cabrera J, Domínguez Blanco A, Crespo Hernández T, Suárez Ojeda R. Mortalidad materna: algunos factores a considerar 1986-1995. Rev Cubana Obstet Ginecol. 1998;24:80-5.
- Rodríguez Iglesias G, Delgado Calzado J, Pérez Riveiro L. Experiencia de 12 años de trabajo en la atención de adolescentes obstétricas críticamente enfermas en la unidad de cuidados intensivos. Rev Cub Obstet Ginecol. 1999;25(30):141-5.
- Urbay Ruiz AA, Cruz Martínez H, Fong Seuc L, Santos Pérez LA, Valledor Tristá R, Molerio Sáez LE. Comportamiento de la enfermedad obstétrica grave. Nueve Años en una Unidad de Cuidados Intensivos. Medicentro. 2002;6:1-8.
- AbouZahr C. Global burden of maternal death and disability. British Med Bull. 2003;67:1-11.
- AbouZahr C. Safe motherhood: a brief history of the global movement 1947-2002. British Med Bull. 2003;67:13-25.
- Lewis G. Beyond the numbers: reviewing maternal deaths and complications to make pregnancy safer. British Med Bull. 2003;67:27-37.
- Murphy DJ, Charlett P. Cohort study of near-miss maternal morbidity and subsequent reproductive outcome. Eur J Obstet Gynecol Reprod Biol. 2002;102:177-8.
- Say L, Pattinson RC, Gulmezoglu AM. WHO systematic review of maternal morbidity and mortality: the prevalence of severe acute maternal morbidity (near miss). Reprod Health. 2004;17(12):3.
- Minkauskiene M, Nadisauskiene R, Padaiga Z. Severe acute maternal morbidity: Lithuanian experience and review. Int J Fertil Women Med. 2006;51(1):39-46.
- Pollock WE. Caring for pregnant and postnatal women in intensive care: what do we know. Anest Crit Care. 2006;19:57-65.
- Velazco A, Rigol O. Puerperio normal. In: Rigol Ricardo O, editor. Obstetricia y Ginecología. Ciudad de La Habana: Editorial de Ciencias Médicas; 2004. p. 107-11.
- Cabezas E, Castell J, Farnot U. Mortalidad materna y perinatal. In: Rigol Ricardo O, editor. Obstetricia y Ginecología. Ciudad de La Habana: Editorial de Ciencias Médicas; 2004. pp. 243-50.
- Oliva Rodríguez JA. Hemorragia postparto. In: Oliva Rodríguez J, editor. Temas de obstetricia y ginecología. Ciudad de La Habana: Editorial de Ciencias Médicas; 2005. p. 1-16.
- Álvarez PL, Águila S, Acosta RB. Sangramiento en obstetricia. In: Rigol Ricardo O, editor. Obstetricia y Ginecología. Ciudad de La Habana: Editorial de Ciencias Médicas; 2004. p. 137-63.
- Fernando D, Jayatilleka A, Karunaratra V. Pregnancy-reducing maternal deaths and disability in Sri Lanka: national strategies. British Med Bull. 2003;67:85-98.
- Oladapo OT, Ariba Aj, Odusoga OL. Changing patterns of emergency obstetric care at a Nigerian University Hospital. Int J Gynaecol Obstet 2007;98:278-84.
- Kaddour C, Soussi R, Haddad Z, Zaghdoudi Z, Magour M, Soussi M. Causes and risk factors of maternal mortality in the ICU. Crit Care 2008;12 (Suppl 2):193-4.
- Ministerio de Salud Pública. Anuario Estadístico de Salud 2005. Ciudad de La Habana: Dirección Nacional de Estadísticas;2005.
- Organización Mundial de la Salud. Manual de la Clasificación Estadística Internacional de Enfermedades, Traumatismos y Causas de Defunción: basada en las recomendaciones de la Conferencia para la Novena Revisión. Organización Panamericana de la Salud; 1978. [Accessed on February 11, 2008]. Available from: http://bases. bireme.br/cgi-bin/wxislind.exe/iah/online/.
- Santos AC, O’Gorman DA, Finster M. Obstetric anesthesia. In: Barash PG, Cullen BF, Stoelting RK, eds. Clinical Anesthesia. Philadelphia: Lippincott Williams & Wilkins; 2001. p. 1141-70.
- Báez A, Giradles EM, Pop A. Crónica de una muerte “no” anunciada: un caso de embolismo por líquido amniótico. Rev Cub Med Int Emerg. 2004;3(1):40-5.
- Drife J. Thromboembolism. British Med Bull. 2003;67:177-90.
- Renz CL, Schmidt GA. Enfermedad drepanocítica. En: Hall JB, Schmidt GA, Wood LD, eds. Cuidados Intensivos. 2nd ed. Ciudad México: McGraw Hill; 2001. p.1781-99.
THE AUTHORS
Albadio Pérez Assef (Corresponding Author: albadio.perez@infomed.sld.cu), specialist in internal medicine and in critical care and emergency medicine; assistant professor, Higher Institute of Medical Sciences of Havana, Cuba.
Jorge Bacallao Gallestey, full professor, Higher Institute of Medical Sciences of Havana, Cuba.
Serafín Alcina Pereira, specialist in family medicine and in intensive care and emergency medicine; instructor, Higher Institute of Medical Sciences of Havana, Cuba.
Yamilka Gómez Vazco, specialist in family medicine and in intensive care and emergency medicine, Havana, Cuba.
Submitted: January 8, 2008 Approved: May 5, 2008