INTRODUCTION
Since the second half of the 20th century, there have been reports of improvements of up to 70% in survival rates following neonatal surgery, mainly due to advances in neonatal intensive care, anesthesia and surgical technique.[1–3]
Neonatal surgery is most commonly performed to correct congenital malformations or birth defects,[2] which are structural anomalies present at birth, whether caused by genetics, pre- or postconception exposure to environmental factors, or some combination of the two.[4] Birth defects requiring neonatal surgery include malformations of several systems: circulatory (especially the cardiac septa, major arteries and veins, and the ventricles and their connections), digestive (such as absence, atresia and stenosis of the esophagus or intestines), nervous, musculoskeletal, respiratory and urinary; as well as diaphragmatic hernia and abdominal wall defects.[4−11]
The complexity of neonatal surgery calls for knowledge and skills that go beyond surgical technique.[12,13] Fluid–electrolyte balance, respiratory and hemodynamic status, and infection risk must be assessed constantly and dynamically to avoid destabilization.
Overall incidence of birth defects varies widely from country to country. The Latin American Collaborative Study on Congenital Malformations (ECLAMC) found an overall prevalence of birth defects in nine participating countries (Argentina, Bolivia, Brazil, Colombia, Chile, Ecuador, Paraguay, Uruguay and Venezuela) of 2.7%, ranging from a low of 1.4% in Ecuador to a high of 4.2% in Brazil.[14,15] Large population studies have estimated prevalence of major congenital malformations at 2%–3% of all live births in developed countries, and up to 7% in developing countries.[5,14] Globally, approximately 1.6% of neonates have congenital malformations that can be lethal or disabling if not diagnosed promptly and treated appropriately.[11,16–18]
In Cuba, the most common birth defects contributing to infant mortality are congenital cardiopathies, followed by digestive system anomalies, diaphragmatic hernias, chromosomal disorders, and malformations of the central nervous system.[19] About half of the malformations are in the cardiovascular apparatus and of these, about 25% are severe.[7,8,19] Cuba’s success in reducing infant mortality (4.3 per 1000 live births in 2015),[19] is due, among other things, to strategies to reduce morbidity and mortality caused by birth defects.[6] However, birth defects and chromosomal anomalies were still the second leading cause of infant death in Cuba in 2014, with a rate of 0.9 per 1000 live births.[19]
In order to improve population quality of life and reduce infant mortality, in the early 1980s, Cuba’s National Health System (SNS) implemented the National Program for Diagnosis, Management and Prevention of Genetic Diseases and Birth Defects, which provides serum alpha-fetoprotein testing, amniocentesis and high resolution ultrasound.[6] When a birth defect is detected prenatally, parents receive genetic counselling on its consequences and prospects, and informed of their options, including pregnancy termination and its risks in the case of potentially lethal or highly disabling anomalies.[6] Early diagnosis, followed by appropriate surgical correction, increases these newborns’ survival and life expectancy.[20]
Dr Guillermo Hernández Amador, pioneer of neonatal surgery in Cuba, began to perform it in 1966 in Havana’s William Soler University Children’s Hospital (HPUWS).[21] In 1970, Dr Olimpo Moreno established the HPUWS neonatal intensive care unit (NICU), since then the neonatal surgery reference center for western Cuba (the provinces of Mayabeque, Artemisa, Havana and Pinar del Río, and the Isle of Youth Special Municipality). It provides comprehensive neonatal clinical and surgical services, with the exception of neurosurgery and cardiovascular surgery (such cases are referred to the Juan Manuel Márquez Pediatric Hospital neonatal neurosurgical unit and the William Soler Heart Center, respectively).
There are few published reports on surgical activity in Cuba’s neonatal surgical centers, particularly on factors affecting case fatality and survival. This study’s main objectives were to describe neonatal surgical case fatality and survival in HPUWS in 2005–2015, estimate risk of death, and identify neonatal characteristics predictive of mortality.
METHODS
Design and population We used hospital administrative data and clinical records to conduct a retrospective cohort study of case fatality in a series of 739 patients in HPUWS’ NICU from January 2005 to December 2015, inclusive.
Analysis The dependent variable was discharge status (alive, deceased). Independent variables were sex (female, male) age (in days) at time of surgery, gestational age (premature <37 weeks, full term 37–41 weeks, post-term ≥42 weeks), birth weight (low <2500 g, normal 2500–4000 g, high >4000 g), surgical indication, surgical order (first, repeat) and other neonatal characteristics presumably associated with risk of death (sepsis, other complications).
Contingency tables were constructed and analyzed to assess associations between neonatal characteristics and discharge status. A classification tree was used to obtain simple estimates of surgical risk and identify predictive variables.
Ethics Signed informed consent is not required for studies based on administrative data. Data collection and processing incorporated procedures to ensure patient anonymity and confidentiality. The study was approved by the HPUWS Scientific Council and Ethics Committee.
RESULTS
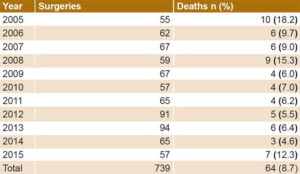
During the study period, 5836 neonates were admitted to the NICU, of whom 739 underwent surgery (12.7%). Surgery incidence peaked in 2013 at 18.4 per 100 admissions (94/512). The highest case fatality occurred in 2005 at 18.2%, although rates were generally stable, and lower, over the study period (Table 1). Approximately 57% of surgeries were performed on boys.
On average, surgery was performed in the first 9.3 days of life (median 3), with 6 patients operated on the day they were born and 64.5% (477/739) in the first 10 days of life. One outlier had surgery on day 80.
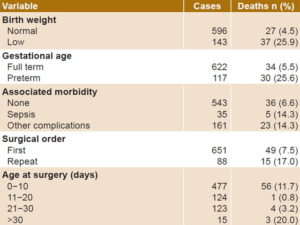
Most neonates were of normal weight (80.6%, 596/739); the majority were born at full term (84.2%, 622/739) (Table 2).
Table 1: Neonatal surgical case fatality, HPUWS, 2005−2015
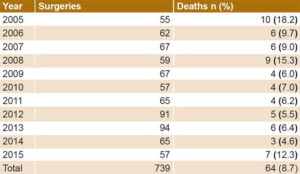
HPUWS: William Soler University Pediatric Hospital
Table 2: Neonatal surgical case fatality* by patient characteristics, HPUWS, 2005−2015
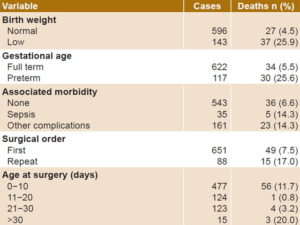
*8.7% overall, 64/739 HPUWS: William Soler University Pediatric Hospital
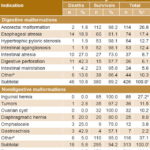
Overall survival was 91.3% (675/739). Operations to correct digestive malformations were the most common (57.6%, 426/739). Anorectal malformations and esophageal atresias were the most common digestive malformations (Table 3). Approximately 46% (34/74) of neonates with esophageal atresias had other major associated malformations, including complex cardiopathies (5/34), anorectal malformations (5/34), and skeletal and renal malformations (2/34). VATER syndrome (vertebrae, anus, trachea, esophagus, and renal abnormalities) was present in 44.1% (15/34) of patients with esophageal atresia. One patient had annular pancreas and gastric perforation, two had diaphragmatic hernias and another two had multiple malformations.
The highest case fatality rates were among neonates with digestive malformations (71.9%, 46/64): digestive perforation (42.3%), intestinal atresia (27%), and esophageal atresia (18.9%). Case fatality for neonates with abdominal wall defects was 42.9% (3/7) for gastroschisis and 25% (3/12) for omphalocele (Table 3).
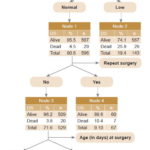
Case fatality distribution for age at time of surgery was J-shaped, with rates of 11.6% in the first 10 days and 20% after 30 days, but <5% at 11–30 days. Figure 1 illustrates risk of death according to neonatal characteristics, notably:
0.087 overall;
0.045 for newborns with normal birth weight;
0.259 (almost triple overall risk) for newborns with low birth weight;
0.038 for newborns with normal birth weight and first surgery, but 0.104 for repeat surgery;
0.005 for newborns with normal birth weight and first surgery at age >10 days; and
0.059 for newborns with normal birth weight and first surgery at age 0–10 days.
Prematurity, low birth weight, more than one surgery, and surgical complications all markedly increased risk of death.
Sepsis was the most common surgical complication (4.7%, 35/739), most often caused by coagulase-negative staphylococci (40%, 14/35) and Staphylococcus aureus (25.7%, 9/35). Among noninfectious complications, the most common were wound dehiscence (4.7%, 35/739), obstructed airways (4.2%, 31/739) and clotting disorders (2.8%, 21/739).
A simple algorithm based on classification trees determined that low birth weight and repeat surgery were the two conditions that best predicted death. Other variables such as prematurity or complications that were important in univariate analysis but did not add appreciably to predictive capacity did not emerge as predictors in the algorithm.
Table 3: Neonatal surgical case fatality and survival by surgical indication, HPUWS, 2005−2015
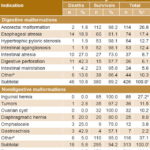
a of total digestive malformations (n = 426) b intestinal stenosis (13), bile duct malformations (12), annular pancreas (6), gastrostomy (5), meconium ileus (4), enteric cyst (1), necrotizing enterocolitis (1),gastroesophageal refl ux (1), intestinal volvulus (1) c 57.6% of total (426/739) d of total nondigestive malformations (n = 313) e biopsies (20), urological malformations (15), testicular torsion (14), ophthalmologic malformations (13), septic arthritis (7), deep abscesses (6), amputation of limbs (5), tracheotomy (5), maxillofacial surgery (4), umbilical defects (4), blockage of choanae (4), diaphragmatic defects (4), hematomas (4),lobar emphysema (2), hydronephrosis (2), nesidioblastosis (2), hydrocele (1),laryngeal stridor (1), tracheobronchial malformation (1), empyema (1), dislocated shoulder (1) f 42.4% of total (313/739) HPUWS: William Soler University Pediatric Hospital
Figure 1: Classification tree predicting discharge status based on low birth weight, surgical order and age at surgery*
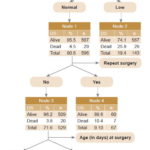
*Prematurity and complications were entered in the initial model but did not emerge in the prediction algorithm. DS: discharge status
DISCUSSION
Neonates undergoing surgery are still adapting to extrauterine life; their fragile homeostasis is placed in double jeopardy by their complex medical conditions and the stresses of surgery and anesthesia.[22] Such surgery constitutes a global challenge, although associated mortality is low in developed countries, which generally enjoy better organization of NICUs, greater resources and better infrastructure, highly qualified personnel, and more advanced maternal and fetal medicine and reproductive genetics.[23]
Transportation is a fundamental component in care of neonates with birth defects requiring specialized treatment, since prompt surgery can minimize complications.[24−27] In Cuba, transferring neonates between settings is considered a risk factor. When unavoidable, it is done as safely and efficiently as possible, in a specially equipped ambulance staffed with a neonatologist and specialized nurse.[26]
Most of the neonates we studied were operated on in the first 10 days of life, which reflects Cuba’s health service coverage and accessibility and also helps explain the high survival rate. Optimal surgical timing is possible when there is appropriate clinical assessment and good patient status. Fewer and fewer neonatal surgical indications require immediate treatment.[28,29] Our study found the lowest case fatality among those operated on days 11–30. Higher case fatality at earlier ages could partly reflect more serious conditions becoming apparent earlier. The almost tenfold increase in risk for normal weight infants operated on for the first time at <10 days compared to their older peers supports this possibility.
The preponderance of male sex among neonatal surgical patients is consistent with reported higher rates in male infants of birth defects such as intestinal atresias and hypertrophic pyloric stenosis, the latter with neonatal sex ratio of 4:1.[22,28–34]
Other authors have observed neonatal mortality inversely proportional to gestational age,[12,35–37] which is consistent with our finding of fivefold higher risk of death in preterm neonates.[38,39]
The most important established predictor of neonatal mortality and morbidity is birth weight: Low birth weight substantially increases the likelihood of illnesses and complications in children aged less than one year.[32,33,40] This was confirmed in our study, which found low birth weight a powerful risk factor for surgical mortality (the a priori risk of 0.087 almost tripled for newborns with low birth weight and fell to less than half for newborns with normal birth weight undergoing first surgery).
Chances of surviving the first month of life are influenced by various environmental, social and genetic factors.[11] With few exceptions, surgery is an emergency. Optimal surgical timing is determined by the neonatologist and the surgeon, based on the newborn’s condition. However, in our experience, if a defect can be corrected in an early neonatal stage, this can be result in faster recovery and better survival rates, especially in the case of digestive malformations. Holguin’s regional neonatal surgery center (in eastern Cuba) reports 91.9% survival after neonatal surgery,[41] findings similar to ours.
The greater frequency of digestive system congenital malformations (especially anorectal malformations and esophageal atresia) in our study is consistent with findings by other authors in Cuba and elsewhere.[28,33,42,43]
Esophageal atresia is a common birth defect globally, occurring in 1 of every 3000 births; 50% of patients have other associated malformations.[34,44] It is considered a surgical emergency, since it is lethal if not corrected. Contemporary surgical treatment of esophageal atresia permits >95% survival.[45] The lower survival rates we observed in our study could be due to accompanying other major malformations, especially complex anorectal, skeletal and renal anomalies, all of which affect clinical outcomes.[46]
Congenital diaphragmatic hernia is one of the biggest remaining challenges in neonatal surgery. Mortality results directly from hypertension at birth combined with pulmonary hypoplasia induced by intestinal herniation during critical stages of pulmonary development.[1] Despite substantial progress in diagnosis and treatment, mortality from this condition is still 30%–60%,[1,41] higher than observed in our study.
Intestinal atresias are the main cause of intestinal occlusion in the neonate; postoperative mortality depends on various factors: anatomical site, associated anomalies, short bowel syndrome, and obstruction from bands or volvulus.[45] Survival rates in our study were comparable to Cuban rates reported elsewhere.[19,46]
Survival of neonates with abdominal wall defects, particularly gastroschisis, would be impossible without major advances in NICUs.[10,11,41] Our >50% survival can be considered good, although the small number of cases means results should be interpreted with caution.
During the postoperative period, neonates are vulnerable to various complications, most commonly, infection.[47,48] Infection at the surgical site constitutes the primary cause of infection associated with surgical care (40% of postsurgical infections),[19] and is the third leading cause of infection associated with medical treatment in children (14%–16%).[47–52] Wound sepsis is preventable but, despite advances in surgical technique, continues to be one of the main challenges in treatment of congenital intestinal malformations. In our study, infectious complications were uncommon, even among patients who did not survive.
Complications during surgical recovery prolong neonatal hospital stay and increase surgical costs and risk of death.[9–11] In our series, patients who died had at least one predictor of neonatal death, most commonly low birth weight. Low prematurity rates in the population studied may be considered a successful outcome of Cuba’s National Maternal–Child Health Program.[53]
The study’s main constraint is that it does not include neonates operated on for congenital cardiopathies or neurological malformations, since these surgeries are not performed at HPUWS. Since these are the most common birth defects requiring neonatal surgery, this hinders comparisons with other studies. Future multicenter studies could provide more information on neonatal mortality from the full range of birth defects.
CONCLUSIONS
Recent important developments in neonatal surgery in Cuba may explain high neonatal survival rates observed in this study. Our study identified some important predictors and applied a simple practical algorithm to estimate surgical risk based thereon. Our results support the importance of factors such as preterm birth and low birth weight in reducing chances of survival, and these must be addressed to improve prognosis for neonatal surgical patients.