ABSTRACT
The methodology is described in detail for the population-based Isle of Youth Study (ISYS) for epidemiological evaluation of CKD associated with cardio-cerebral vascular disease, arterial hypertension, diabetes mellitus, and other risk factors.
Background Chronic kidney disease emerges as an important and growing global health problem associated with an increase in the incidence and prevalence of the above mentioned diseases.
ISYS Objectives Ascertain CKD morbidity and its relation to chronic vascular diseases and other risk factors in whole population of Cuba’s Isle of Youth special municipality.
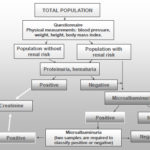
Method 96.6% of the Isle of Youth’s total population (80,117 inhabitants) was studied, all ages and both sexes, November 15, 2004-April 30, 2006. The public was offered general information on the objectives and benefits of the study, and participants provided informed consent. Active screening was performed via personal interview questionnaire and urine sample to determine markers of kidney damage: proteinuria and hematuria (Combur-10-Test) and microalbuminuria (Micral-Test), according to a diagnostic algorithm. For those testing positive for any marker, serum creatinine was studied and glomerular filtration rate (GFR) calculated – in adults by Cockcroft-Gault and Modification of Diet in Renal Disease (MDRD) formulas and in children aged <15 years, by Schwartz – to stratify CKD by stages. Blood pressure, height, weight, and body mass index (BMI) were determined.
Expected Results Prevalence of kidney damage markers in general population and risk groups; relationship in population between CKD and cardio-cerebral vascular disease, diabetes mellitus, hypertension, and other risk factors; comparison of Cockcroft-Gault and Modification of Diet in Renal Disease (MDRD) formulas for measuring the GFR and their application to studies involving mass population screenings; and stratification of CKD in population.
Conclusions ISYS Phase I, active screening of markers for renal damage was concluded using the methodology described above; results are pending publication.
Key Words: Chronic kidney disease; kidney damage markers; screening; prevalence
INTRODUCTION
Chronic kidney disease (CKD) has emerged as an important and growing global health threat associated with increased incidence and prevalence of cardiovascular disease (CVD), cerebrovascular disease, hypertension, diabetes mellitus, obesity, and aging.[1]
This group of diseases shares common characteristics since vascular damage is present in their origin, physiopathology, complications, and progression to chronic conditions. These diseases generally share the same risk factors and some of these may be a consequence of others.
They have epidemic behavior and are responsible for the highest global burden of morbidity, disability, and mortality. For these reasons, they can be grouped in an integrated conceptual framework of chronic vascular disease, thus contributing to an integrated approach to research and intervention. [2,3]
These diseases’ high morbidity and mortality burden is a growing and global phenomenon affecting developed and developing countries alike, although at more accelerated rates in the latter (Table 1).[4-10]
Table 1: Projections for Global Burden of Non-Communicable Diseases with Vascular Damage (millions of patients)

Table 2: Chronic Kidney Disease and Chronic Vascular Diseases in Cuba and the Isle of Youth: Mortality& Morbidity, 2004

*1st, **3rd, ***8th and ****13th cause of death ***** Year 2002
Known mortality and morbidity data for these diseases in Cuba and the Isle of Youth in 2004, before the ISYS study, are shown in Table 2.[11]
There are few population-based epidemiological studies on CKD morbidity from early stages, and those in existence have been carried out based on population samples. The Third US National Health and Nutrition Examination Study (NHANES III, 1988-1994)[12] studied a sample of 15,625 persons aged ≥20 years and found a prevalence of 11% of persistent albuminuria, which increased to 16.8% in the NHANES study 1999- 2004.[13]
The AUSDIAB study[14] conducted in Australia (1999-2000) analyzed a sample of 11,247 persons aged ≥25 years, finding 18% with proteinuria, microalbuminuria, or hematuria.
The PREVEND study[15] conducted in Groningen, Holland (1997-1998) evaluated a sample of 8,592 persons aged 28-75 years, and found 10.6% with persistent albuminuria.
The Cuban ISYS is the only study of its kind in the world in total population. Units analyzed were the individual and the family. Its purpose is to carry out an epidemiological characterization of CKD and its relationship to other diseases with vascular damage, as well as to other risk factors, that may influence the origin and progression of the disease. It also focuses on laying groundwork for scientific implementation and evaluation of population-based interventions, as well as longitudinal surveillance of morbimortality and associated risk factors over the long-term.
The ISYS Study is divided into the following phases:
Phase 1: Active screening for kidney damage markers and associated risk factors for CKD and chronic vascular disease in total population.
Phase 2: Diagnostic confirmation and treatment for specific patients.
Phase 3: Longitudinal follow-up of patients detected and persons testing negative for kidney damage markers.
Phase 4: Population-based intervention.
This paper gives a detailed description of Phase 1 methodology, including active screening of kidney damage markers and associated risk factors in total population on the Isle of Youth.
ISYS: GENERAL OBJECTIVES Ascertain CKD morbidity, its distribution and relationship to CVD, cerebrovascular disease, hypertension, diabetes mellitus, and other associated risk factors, in total population on the Isle of Youth, Cuba.
SPECIFIC OBJECTIVES
- Determine the relative frequency of kidney damage markers: proteinuria, microalbuminuria, and hematuria and their distribution according to sex, age, and kidney function in total population and risk groups.
- Comparatively evaluate the Cockcroft-Gault formula adjusted to body surface and the Modification of Diet in Renal Disease (MDRD) formula for estimating GFR and CKD stage stratification.
- Describe distribution of cohort of cases with kidney damage markers according to CKD stage stratification.
- Describe the relationship between CKD and CVD, cerebrovascular disease, hypertension, diabetes mellitus, and other associated risk factors in total population.
METHOD
Study Period: Phase 1
Phase I was carried out by the Institute of Nephrology and the Municipal Health Department of the Isle of Youth, November 15, 2004-April 30, 2006.
Site Selection for the Study
The Isle of Youth is a special municipality of the Republic of Cuba, located 120 km south of the Cuban mainland, with an area of 2,419 km2, accessible by air or sea. The population includes primarily persons who emigrated to the Isle in their youth, at the end of the 60s and into the 70s, plus their descendents. Later migratory changes have been insignificant, resulting in a population composed of a representation of the various Cuban provinces.
The Isle’s territorial extension and population are similar to other islands of the Caribbean. It has the same health system as the rest of the country; its health indicators are similar to those of the whole country and of developed nations. Access to primary health care, nephrology care, and all health services is universal and free of charge. The Isle has its own media, including local TV, radio and a newspaper. For all these reasons its population was considered appropriate for this type of epidemiological study.
Universe
The 2002 Cuban census recorded 86,559 inhabitants on the Isle, of whom 80,117 were registered in the primary health care system by family doctors.[16,17] This difference may be due to the fact that many people included in the census as residents of the Isle of Youth actually work or study permanently elsewhere, or it may simply be due to migratory shifts. In Phase 1, 77,423 individuals were studied (96.6% of those registered by the health system) grouped in 21,115 families.
Inclusion Criteria
Persons of any age, both male and female, permanent residents of the Isle of Youth, who provided written informed consent.
Exclusion Criteria
Persons not permanent residents of the Isle of Youth; those who did not provide written informed consent.
Preparatory Phase of the Study
Organizational Structure
- The Isle of Youth health system is comprised of the Municipal Health Department, 3 community polyclinics and 114 family doctors’ offices at the primary care level covering the whole population, the latter staffed by family doctors and nurses responsible for providing care to persons in their geographic area. There is 1 municipal hospital with nephrology services (including hemodialysis center) and a medical school. Medical personnel include 455 physicians (227 of these family doctors and 4 specialists in nephrology) and 802 nurses.
- A Municipal Coordination Center for the study was created at the Municipal Health Department and another 3 coordinating centers were established in the polyclinics. Each center was staffed by a coordinator and auxiliary personnel for organizational activities, training, collection and review of questionnaires, supervision of procedures, validation of data, and introduction of information into the study database.
Use of Information Technologies
- A reporting system was created to produce a daily report on completed questionnaires as well as on daily urine and blood analyses; information flowed from family doctors’ offices to the polyclinics and from there to the Municipal Coordination Center.
- A database was created with an automated validation system for quantitative and qualitative variables contained in the questionnaire.
Quality Control: Procedures & Data Validation
Teams were established in each coordinating center for supervision, quality control of procedures, and data validation.
Updating Medical Records from the Family Doctors’ Offices & Polyclinics
Updates were generated for patient clinical histories at all family doctors’ offices and polyclinics.
Training
A total of 114 family doctors and 212 family nurses were trained and certified to carry out interviews and complete questionnaire data, obtain physical measurements, and perform diagnostic urine tests; and 7 laboratory technicians were trained to supervise quality control of urinalyses and blood sampling, and to analyze serum creatinine.
Standardization of Instruments & Equipment
The sphygmomanometers, scales, height rods, and laboratory equipment were standardized and certified by the Biomedical Equipment Department of the municipal health authority.
Pilot Study
A pilot study was performed in 3 family doctors’ offices with 56 persons from the general population, including a proportion of known diabetic and hypertensive patients, in order to identify a larger number of positive cases and evaluate the diagnostic tests. The screening flowchart was tested together with the recording system, the informed consent instrument, questionnaire, and diagnostic tests at the doctor’s office; physical measurements, and other procedures were validated by the trained monitoring group. This small-scale study identified 9 patients with a history of some kidney disease; 7 of whom had kidney damage markers in their urine. Twenty-six new patients with no history of kidney disease were detected with markers, while 21 were negative. Patients with positive markers were evaluated to confirm diagnostic results and apply appropriate treatment. As a result of the pilot study, adjustments were made.
Procedures for Screening Total Population
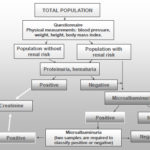
Phase 1 implementation and active screening for renal damage makers and associated risk factors in the population were carried out through public information disseminated within the community, home visits, and at doctors’ offices (Figure 1).
General Information to the Public
- Political and social organizations as well as local government authorities were informed of the study’s objectives and expected benefits, and their collaboration requested.
- Local media (newspaper, radio and television), carried information to the general public on the study’s objectives and expected benefits. The population was asked to cooperate with the study in neighborhood seminars offered by family doctors and nurses and through local organizations.
Home Visits: Participant Recruitment
Family doctors and nurses made home visits to explain to each person and family the study’s objectives and benefits as well as procedures such as urine collection, providing both verbal and written information. During the visit, potential participants were asked to visit their doctor’s office to carry out the screening studies.
Physicians Offices: Informed Consent
Adults were incorporated into the study once each had provided signed written informed consent. Parents or guardians were required to sign informed consent for children aged ≤15 years or for those disabled persons under guardianship unable to provide their own informed consent.
Questionnaire
- A questionnaire was completed by means of an interview carried out by trained interviewers, who were also provided with written instructions.
- The questionnaire includes several sections for data collection and analysis.
- Identification and socio-demographic data was recorded by assigning an individual registration number to each participant comprised of the polyclinic code, doctor’s office code, number assigned each family, and number of the individual in that family. This system was used to facilitate analysis of each person individually and of the family unit. Elements recorded included: sex (male or female); skin color (white, black, mixed, other); date of birth; level of education completed (elementary school, junior high school, high school, university); and occupation. Access to the patient’s identity was limited to family physicians and other physician specialists directly involved in patient follow-up. To all others, identification was limited to the registration number.
- Data taken from the family medical history at the family doctor’s office and certified by a physician included: current pregnancy status; history of low birth weight, diabetes mellitus, hypertension, hypercholesterolemia, obesity, CVD, cerebrovascular disease, kidney disease, dialysis treatment, or kidney transplant.
- Participant-provided data regarding family history and own pathologies included: diabetes mellitus, hypertension, CVD, cerebrovascular disease, kidney disease, and others. Personal lifestyle data recorded include: smoking, workplace exposure to nephrotoxic substances, and use of medications with nephrotoxic effects.
Physical Measurements
- Blood pressure (BP-mmHg) was measured by trained and certified personnel. BP was measured only once using standardized pointer aneroid sphygmomanometers certified by the metrology department of the municipal health authority.
- An appropriate armband size was used, covering at least 80% of the arm. In children, pediatric cuffs were used. Measurements were taken after the person had been seated in a chair, remaining still for at least 5 minutes with their feet on the ground, arm at heart level.
- Weight was measured in kilograms by trained and certified personnel. Calibrated, age-appropriate scales certified by the metrology department of the municipal health authority were used. Needle indicator was reset to zero before each weighin.
- Persons weighed-in barefoot and with as little clothing as possible. Small children were placed in the center of the scale, keeping them as still as possible. If a sheet or cloth was used on the scale, its weight was subtracted from the final value. The needle was observed until it remained still and in equilibrium.
- Height was measured in centimeters by trained and certified personnel. Height rods were standardized and certified by the metrology department of the municipal health authority. Height rods and measuring tapes were also reviewed to check complete number set.
- In small children, a measuring tape was stretched out on a flat surface and the child was placed in a decubitus supine position on a firm, flat surface with knees extended. The child was measured from the top of the head to the heel, while holding the head and knees in position.
- In older children and adults, a vertical height rod (stadiometer) was used, participants standing barefoot and without error-prone hair accessories or hairstyles, back to rod, gaze forward, knees straight, head erect, with right-angle measure flat at top of head.
Laboratory Tests: Urine
- First morning, mid-stream urine specimens were collected, before subjects began physical activity. Specimens were not taken if urinary tract infection was present or in women during or 3 days before or after menstruation. A urine collection bag was used for small children.
- Combur-10-Test (Roche) was performed on urine of all participants, measuring 10 parameters: density, pH, proteins, erythrocytes and hemoglobin, leukocytes, nitrites, glucose, ketones, urobilinogen, and bilirubin.
- Micral-Test (Roche) was carried out to study microalbuminuria in all participants whose urine tested negative for markers of proteinuria, proteinuria plus hematuria, or isolated hematuria, and who were also classified as individuals with renal risk determined by questionnaire data and physical measurements: children aged <5 years, adults aged ≥60 years, diabetics, persons with high blood pressure (HBP), CVD, any type of kidney disease, obesity with hypercholesterolemia, and born with low birth weight.
- For ISYS Phase 2 (studies of individual patients with markers of kidney damage), Micral-Test will be repeated on those who tested positive in Phase 1, until 2 positive or 2 negative results are obtained, to record a sustained positive or negative microalbuminuria.
Laboratory Tests: Blood
- Blood samples were taken to study serum creatinine in all patients testing positive for proteinuria, proteinuria plus hematuria, isolated hematuria or microalbuminuria. The Jaffe technique, with Roche Laboratory reagents and Hitachi 902 processing equipment, was used to perform serum creatinine. Quality control was carried out through Roche Laboratories low value (Precinorm) and high value (Precipath) controllers, according to the Levey-Jennings graphic method for study of repeatability, reproducibility, and precision.
- In adults aged ≥15 years, GFR (mL/min/1.73 m2 of body surface) was calculated using the Cockcroft-Gault[18] formula adjusted to body surface[19] and MDRD.[20, 21]
- Cockcroft-Gault GFR adjusted to body surface = (140 – age)/serum creatinine (mg/dL) x (weight in kg/72) x 0.85 in females x body surface/1.73 m2.
- Body surface (m2) is estimated using the formula = 0.20247 x height (m)0.725 x weight (kg)0.425.
- MDRD GFR = 186.3 x serum creatinine (mg/dL)-1.154 x age -0.210 x 0.742 for females x 1.21 if the person is black.
- For children aged <15 years, GFR was calculated using the Schwartz[22] formula.
- Schwartz GFR= K x height (cm)/serum creatinine (mg/dL). K is a constant that varies with age. Its value is: Premature neonates 0-1 year: 0.33 Term neonates 0-1 year: 0.45 1-12 years: 0.55 13-14 years: 0.70
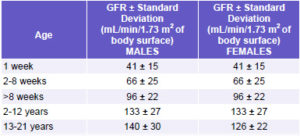
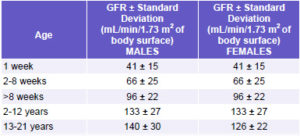
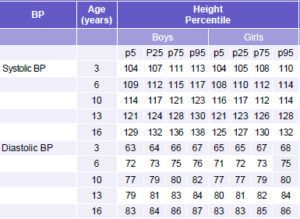
In children, GFR values are evaluated according to age (Table 3),[23] in children aged ≥2 years, values are evaluated the same as adults.
Table 3: Glomerular Filtration Rate (GFR) in Children, by Age
Definitions of Main Variables
- Age: distribution in age groups
- Sex: male or female
- Skin color: white, black, mixed, other
- Proteinuria: Combur-10-Test reading intervals for albumin in urine are: negative (-); 30 mg/dL – 0.3 g/L (1+); 100 mg/ dL – 1 g/L (2+); 500 mg/dL – 5 g/L (3+) with an accuracy of 90% referred to radial immunodiffusion. Tests were considered positive when showing values of ≥0.3 g/L of albumin.
- Hematuria: Combur-10-Test reading intervals for intact erythrocytes in urine are: negative (-); 5-10 (1+); 25 (2+); 50 (3+); 250 (4+) erythrocytes/µL with an accuracy of 90% or more referred to the chamber recount. Tests were considered positive when showing values of ≥5-10 erythrocytes/µL.
- Microalbuminuria: Micral-Test reading intervals for albumin in urine are: negative (-) and at a cut off point ≥20 mg/L albumin in urine has analytical sensitivity of ≥95% (90%-99% range) and a specificity >80% (70%-90% range). Tests were considered positive when showing albumin values of ≥20 mg/L.
- Glucosuria: Combur-10-Test reading intervals for glucose in urine are: normal (-); 50 mg/dL-2.8 mmol/L (1+); 100 mg/dL -.5.5 mmol/L (2+); 300 mg/dL-17 mmol/L (3+); 1000 mg/dL-55 mmol/L (4+) with an accuracy of 90% referred to the hexokinase method. Tests were considered positive when showing glucose values of ≥50 mg/dL.
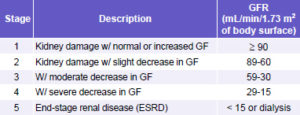
- Chronic kidney disease (CKD): Patients with markers of kidney damage: (proteinuria, hematuria, or microalbuminuria) or GFR <60 mL/min/1.73 m2 without markers for 3 months or more, as defined by Kidney Disease Outcomes Quality Initiative (K/DOQI) criteria, are submitted to CKD stage stratification (Table 4) regardless of the cause of kidney damage. This stratification is applicable to the adult population[24,25] and to children aged ≥2 years.[23]
Table 4: Stratification of CKD According to GFR
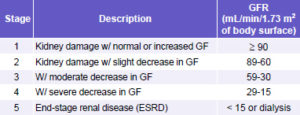
- Chronic kidney failure (renal insufficiency): Patients with GFR <60 mL/min/1.73 m2 of body surface, corresponding to Stage 3 CKD or higher.
- Cardiovascular disease (CVD): Patients whose diagnosis has been documented by a physician.
- Cerebrovascular disease: Patients whose diagnosis has been documented by a physician.
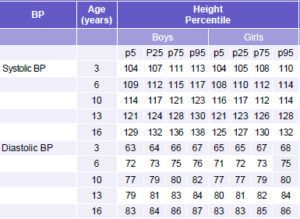
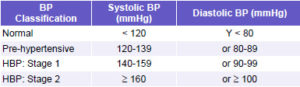
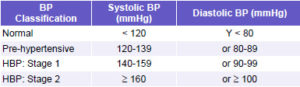
- HBP: Patients whose diagnosis has been documented by a physician, or persons aged ≥18 years with systolic BP of ≥140 mmHg and/or diastolic BP of ≥90 mmHg during interview; HBP classified according to values established by the Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure Seventh Report, 2003 (JNC7)[26] (Table 5). In children aged <17 years, HBP is classified according to values established by the Task Force on High Blood Pressure in Children and Adolescents, 1996 (Table 6).[27]
Table 5: Classification of BP in Adults & Adolescents Aged ≥18 Years
- Patients with Controlled HBP: Patients with known HBP (obviously new HBP patients detected during the interview were not included) with systolic BP <140 mmHg and a diastolic BP <90 mmHg.
- Diabetes mellitus: Patients whose diagnosis has been documented by a physician.
Table 6: BP Classification in Children Aged <16 Years*
*95 percentile BP in children aged 3-16 years, according to height (for 17-year olds, same value was used as for 16-year olds).
Presumed diabetic patients: Persons of any age or sex without a history of diabetes mellitus in which glucosuria was detected during the study.
- Smoking: Patients were classified as smokers and nonsmokers according to their condition at the time of interview.
- Hypercholesterolemia: Patients whose diagnosis has been documented by a physician.
- Body Mass Index (BMI): BMI = kg/m2
The population aged ≥15 years was evaluated according to the following parameters:
Under weight: <18.5 kg/m2
Normal weight: 18.5-24.9 kg/m2
Overweight: 25.0-29.9 kg/m2
Obese: ≥30.0 kg/m2
In children aged <15 years, BMI was calculated with the same formula, but evaluation depended on age, sex and percentiles.
Follow-Up with Patients Detected with Positive Markers in Urine
Patients detected were entered in Phase 2 of the study for diagnostic confirmation and specific treatment. Depending on the type of marker, patients follow a diagnostic-therapeutic algorithm for family doctors, nephrologists, or other medical specialists as required.
Data Processing Techniques
All information was processed automatically. A digital database was set up with Microsoft Access, permitting massive entry of data from questionnaires, with a qualitative and quantitative data validation system, using minimum and maximum value intervals to minimize margin of error. Once required fields are entered, the system automatically calculates age in years; body mass index; GFR for adults aged ≥15 years by Cockcroft-Gault adjusted to body surface and MDRD; and GFR for children aged <15 years, by Schwartz. It also stratifies patients according to CKD Stages, based on GFR in population aged ≥2 years.
Data Analysis Techniques
Frequency distribution was calculated for positive cases of kidney damage markers (proteinuria, proteinuria and hematuria, microalbuminuria, and isolated hematuria) in total population studied.
Frequency distribution was constructed for classification of renal function according to GFR estimated by Schwartz for population aged 2-14 years, and by Cockcroft-Gault adjusted to body surface and MDRD formulas for population aged ≥15 years. Analysis was conducted for cases of children aged ≥2 years who had positive markers of kidney damage in whom serum creatinine had been studied to calculate GFR.
Likewise, double entry tables were devised to cross-reference this classification with the following variables: sex, age group, skin color, HBP status, and diabetes status in patients aged >20 years; as well as sex, age, and kidney damage markers in urine for those aged 2-14 years.
Frequency distribution for the different combinations of the 4 main risk factors was also calculated: diabetes, HBP, obesity or overweight, and personal history of CVD. A cross-referenced classification chart was also plotted for all these combinations with the groups depending on state of kidney function.
Concordance between the 2 classification criteria of kidney function – Cockcroft-Gault and MDRD formulas – was assessed by Kappa statistics and by fitted linear regression equation with a zero intercept and a slope estimated by the “bootstrap” method with 50 replicates.
EXPECTED RESULTS
- Prevalence of kidney damage markers in general population.
- Prevalence of kidney damage markers in renal risk groups.
- Prevalence of CKD and stage stratification.
- Relationship between CKD and CVD, cerebrovascular disease, diabetes mellitus, HBP and other associated risk factors at population level.
- Comparison between Cockcroft-Gault and MDRD formulas for measuring GFR and their applicability in mass screening studies.
CONCLUSIONS
The background, objectives, methodology, and results expected from ISYS Phase 1 are described. These are related to screening for kidney damage markers, stratification of CKD and its relation with CVD, cerebrovascular disease, HBP, diabetes mellitus and associated risk factors. Publication of Phase 1 results is in preparation.
Future Implications of the ISYS Study
According to its design and methodology, ISYS Phase 1 results will serve as:
- A basis of enhanced scientific knowledge regarding CKD, chronic vascular diseases and associated risk factors in total population.
- The baseline groundwork for future lines of research: clinical-epidemiological studies of cases and controls, cohorts, controlled therapeutic trials, and population interventions for decreasing morbidity, mortality, and disability in the general population.
- The bases for an epidemiological surveillance system to measure incidence, prevalence and trends of CKD, chronic vascular diseases, and associated risk factors in the general population.
- Contribution to the improvement of health services and planning of human and material resources in the health sector.
- Contribution to enhance the scientific knowledge base and level of health professionals and technicians.
- Contribution to improving health promotion and education within the general population.
The following erratum has been corrected in all versions of this article.
The correct formula for MDRD appearing on page 27 is: MDRD GFR = 186.3 x serum creatinine (mg/dL)-1.154 x age-0.203 x 0.742 for females x 1.21 if the person is black.
References

- Dirks JH, Dezeeuw D et al. Prevention of chronic kidney and vascular disease: toward global health. The Bellagio 2004 Decla ration. Kidney Int 2005;68:S1-S6.
- Dirks JH, Robinson SW, Alderman M, Couser WG, Grundy SM, Smith SC, et al. Meeting Report on the Bellagio Conference. “Prevention of vascular diseases in the emerging world: an approach to global health equity.” Kidney Int 2006;70:1397-402.
- Almaguer M, Herrera R, Pérez-Oliva J. Epidemia global de enfermedades vasculares crónicas. Un nuevo paradigma y desafío. Rev Hab de Ciencias Médicas. Forthcoming 2007.
- Yusuf S. Global burden of cardiovascular diseases. Part I. General considerations, the epidemiologic transition, risk factors and impact of urbanization. Circulation. 2001;104:2746-53.
- International Diabetes Federation. Diabetes Atlas. 2nd ed. 2004. Brussels (Belgium); 2004.
- King H, Aubert RE, Hermann WH. Global burden of diabetes. 1995- 2025, prevalence, universal estimates and projections. Diabetes Care.1998;21: 1414-31.
- Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet 2005;365:217- 223.
- Lysaght M. Maintenance dialysis population, dynamics, current trends and long term implications J Am Soc Nephrol 2002;13:S37-S40.
- World Kidney Day. An idea whose time has come. Kidney Int 2006;69:781-2.
- Dirks J. A world perspective on renal care. The challenges of prevention and treatment. EDTNA/ERCA J 2005;31:72- 4.
- Anuario Estadístico de Salud. Cuba. 2004. Dirección Nacional de Estadísticas. Ministerio de Salud Pública. Cuba. 2004.
- Coresh J, Astor B, Greene T et al. Prevalence of CKD and decreased kidney function in the adult US population. Third National Health and Nutrition Examination Survey. Am J Kidney Dis 2003;1(19):1-12.
- Saydah S et al. Prevalence of CKD and associated risk factors. United States 1999-2004. MMWR Weekly 2007;56 (08):161-5.
- Chadban S, Briganti E, Keer P et al. Prevalence of kidney damage in Australian adults. The Austr Kidney Study. J Am S Nephrol 2003;14 (Suppl 2):S131- S138.
- Hillege HL, Janssen WMT, Bak AAA, Diercks GFH, Grobee DE, Crijins HJGM et al. Microalbuminuria is common also in a nondiabetic, nonhypertensive population and an independent indicator of cardiovascular risk factors and cardiovascular morbidity. J Int Med 2001;249 (6):519-526.
- Censo de población y viviendas 2002. Cuba. http://www.cubagov.cu/otras_info/ censo/población.htm (accessed 5 July 2007).
- Departamento de Estadísticas. Dirección Municipal de Salud. Isla de la Juventud. Población dispensarizada por los médicos de la familia. Departamento de Estadísticas. Dirección Municipal de Salud. Isla de la Juventud. Cuba. 2004.
- Cockcroft DW, Gault MH. Prediction of creatinine clearance from serum creatinine. Nephron 1976;16:31-41.
- DuBois D, Dubois EF. A formula to estimate the approximate surface area if height and weight be known. Arch Intern Med 1916;17:863-71.
- Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. A more accurate method to estimate glomerular filtration rate from serum creatinine. A new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med 1999;130:461-70.
- Levey AS, Greene T, Kusek JW, Beck GJ, and MDRD Study Group. A simplified equation to predict glomerular filtration rate from serum creatinine. J Am Soc Nephrol 2000;11:155A (abstr A0828).
- Schwartz GI, Brion LP, Spitzer A. The use of plasma creatinine concentration for estimating glomerular filtration rate in infants, children and adolescents. Pediatr Clin N Amer 1987;34:540-71.
- Hogg RJ, Furth S, Lemley KV et al. National Kidney Foundation. Kidney Disease Outcomes Quality Initiative Clinical Practice Guidelines for Chronic Kidney Disease in Children and Adolescents: Evaluation, Classification and Stratification. Ped 2003;111 (6):1416-21.
- National Kidney Foundation: K/DOQI. Clinical Practice Guidelines for Chronic Kidney Disease: Evaluation, Classification and Stratification. Am J Kidney Dis 2002;39:S1-S266.
- Levey AS, Eckardt KU, Tsukamoto Y, Levin A et al. Definición y clasificación de la enfermedad renal crónica: Propuesta de KDIGO (Kidney Disease: improving global outcomes). Kidney Int (edición español) 2005;1:135-46.
- Chobaniam AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jones DW, Materson BJ, Wright JT, Roccella EJ and the National High Blood Pressure Education Program Coordinating Committee. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure. JAMA:289:2560- 72.
- Task Force on High Blood Pressure in Children and Adolescentds. Ped 1996;98:649-58.
THE AUTHORS
Miguel Almaguer López (Corresponding Author) Specialist in Nephrology, Associate Professor, Higher Institute of Medical Sciences, Havana, Senior Researcher, Chief of Preventive Nephrology Services, Nephrology Institute, Havana, Cuba-nefroprev@infomed.sld.cu
Raúl Herrera Valdés, Specialist in Nephrology, Full Professor, Higher Institute of Medical Sciences, Havana, Senior Researcher, Senior Academician, Nephrology Institute, Havana, Cuba
José Chipi Cabrera, Specialist in Nephrology, Instructor, Isle of Youth Faculty of Medicine, Head of Nephrology Service, Héroes del Baire Hospital, Isle of Youth, Cuba
Xidix Toirac Cabrera, Specialist in Rheumatology, Héroes del Baire Hospital, Isle of Youth, Cuba
Osvaldo Castellanos Rabanal, Specialist in Epidemiology, Municipal Health Director, Isle of Youth, Cuba
Jorge Bacallao Gallestey, Professor, Higher Institute of Medical Sciences, Havana, Atherosclerosis Investigations and Reference Center, Havana, Cuba