ABSTRACT
INTRODUCTION Hypertension is one of the most studied risk factors for cardiovascular disease in adults; in children and adolescents, its global prevalence changes with age, from 1%–3% in children to 3.2% in adolescents. In adults, in addition to hypertension, several biochemical markers of cardiovascular risk have been identified. Confirming an association between these and hypertension in childhood and adolescence would allow for more timely diagnosis and monitoring of cardiovascular disease, since the presence of both the markers and hypertension would imply increased risk.
OBJECTIVE Confirm an association between biochemical risk markers of cardiovascular disease and hypertension in children aged 8 to 11 years.
METHODS A cross-sectional study of 373 children aged 8–11 years was conducted in 3 primary schools in the city of Santa Clara in central Cuba. The variables examined were age, sex, height, blood pressure, cholesterol, triglycerides, lipoproteins and apolipoproteins. The children were classified as normotensive, prehypertensive or hypertensive, based on blood pressure readings and percentiles for age, sex and height. Descriptive statistics were calculated for quantitative variables. A bivariate analysis, tests of independence for qualitative variables and a means comparison for quantitative variables (ANOVA and its nonparametric alternative, the Kruskal Wallis test) were performed. Fisher’s F-test and its associated probability value were employed.
RESULTS Some 32.2% of the children were prehypertensive and 5.1% hypertensive. Cholesterol and triglyceride values were significantly higher in hypertensive than in normotensive children (p = 0.028 and p = 0.047, respectively). HDL numbers were higher in normotensive children (p = 0.001), and LDL numbers and the LDL/HDL ratio were higher in the hypertensive children, with differences between groups (p = 0.001 for both variables). There were differences between the three blood pressure categories for lipoprotein(a) and ApoA (p <0.001 and p = 0.001), for ApoB and for the ApoB/ApoA ratio (p <0.001 for both variables), with lower ApoA values and higher ApoB and ApoB/ApoA values in the hypertensive children.
CONCLUSIONS The biochemical risk markers most strongly associated with hypertension in children are ApoB values, LDL, lipoprotein(a), and LDL/HDL and ApoB/ApoA ratios.
KEYWORDS Adolescent, child, hypertension, apolipoproteins, cardiovascular diseases, risk factors, Cuba
INTRODUCTION
Globally, cardiovascular disease (CVD) is a major cause of illness and the leading cause of death, accounting for more than 17.9 million deaths per year in 2015. This number is expected to grow to more than 23.6 million by 2030.[1] CVD is the main cause of death in Cuba and in high-income countries, although it is also on the rise in other middle- and low-income countries.[2]
Atherosclerosis is a process characterized by abnormal deposits of lipids, cholesterol and plaque, leading to coronary artery disease and other cardiovascular problems. Its origin is multifactorial, and many of its main risk factors are known.[3] It is increasingly found in children at younger ages. The importance of determining their health status in relation to its main causal factors facilitates the adoption of preventive and therapeutic interventions to avert or minimize its consequences.
A risk factor for a condition is causal if in its absence, the condition in question would not have occurred at all or would not have occurred until later.[4,5] Cardiovascular risk factors include hypertension, diabetes, dyslipidemia, obesity, smoking, genetic factors and family history.[6]
IMPORTANCE The results provide evidence for greater attention to hypertension in children and adolescents, and for adding study of biochemical markers to conventional risk indicators to ensure timely CVD risk assessment.
The presence of a cardiovascular risk factor is influenced by the presence and extent of coexisting risk factors. Epidemiologic and clinical studies have shown that individuals with multiple risk factors are at higher risk for cardiovascular disease than individuals with just a single risk factor.[7] Concurrence of lipid disorders (as evidence of atherosclerosis) with hypertension increases risk and makes the determination of related biochemical markers particularly important.
Many risk factors are determined by behaviors and attitudes acquired in childhood and continued throughout life. Thus, timely prevention of cardiovascular risk should begin in childhood and adolescence.[8] In recent decades, interest has grown in identifying factors that predispose children and adolescents to developing cardiovascular disease as part of public policies aimed at primary prevention.[9,10]
Hypertension (HT) is one of the world’s most common disorders in adults; its prevalence increases with age, and it is a risk factor for cardiovascular disease. HT is a serious health issue, because its consequences include heart, blood vessel, kidney and retina damage. HT in children is more common than might be expected; globally, its prevalence ranges from 1%–3% in children to 3.2% in adolescents.[11] In Cuba, the prevalence in youngsters aged 5–14 years was 1.8 per 1000 population in 2017.[12]
It is currently recognized that onset and progression of atherosclerosis are related to an inflammatory process in the blood vessels,[13] and recent studies have focused on identifying a number of biochemical markers such as angiogenic growth factors, plate let activation and thrombosis related to lipids and other factors.[14,15] Available data show that these local and systemic inflammatory markers play a key role in development and progression of the atherosclerotic process. Several of them are considered independent risk markers for atherosclerosis and CVD and can therefore be used for screening, diagnostic and monitoring purposes.[5]
Oxidation of low-density lipoproteins (LDL) in the subendothelium is a key factor in vascular damage. LDL molecules are carried through the endothelial cells and accumulate in the vascular intima, where they can undergo oxidation, glycosylation, acetylation and triglyceride enrichment, thus increasing their atherogenicity.[15]
Oxidized LDL particles have atherogenic effects, although other lipoproteins, such as very low-density lipoproteins (VLDL), intermediate-density lipoproteins (IDL) and lipoprotein(a), do as well. Atheroma plaque formation is a complex inflammatory process involving various cells and mediators. Oxidized lipoproteins infiltrated into the subendothelial space stimulate intima’s cells to produce proinflammatory cytokines and chemokines that activate circulating monocytes, which then enter tissues, becoming inflammatory macrophages and later, foam cells, resulting in intracellular accumulation of cholesterol esters and fatty streak formation.[15]
The purpose of this study is to draw attention to the relatively high HT prevalence in Cuban children and adolescents, frequently accompanied by abnormal values of biochemical markers that are predictors of CVD risk. A particularly important motivation is to prevent early-onset CVD and reduce mortality from this cause in Cuba.[1,16]
METHODS
Design and sample Between April 1, 2014 and March 31, 2015, a cross-sectional study was conducted of 373 students aged 8 to 11 years from schools in the city of Santa Clara in central Cuba, chosen for ease of access. All children from the third through fifth grade were included whose parents provided written informed consent.
Variables
Blood pressure For HT classification, criteria of the 4th Report of the American Academy of Pediatrics[11] and the recommendations of the European Society of Hypertension of September 2009[17] were used. Children were classified as normotensive if average systolic and diastolic pressure were both less than the 90th percentile; prehypertensive if average systolic and/or diastolic pressure were greater than or equal to the 90th and less than 95th percentile; and hypertensive if average systolic or diastolic pressure was above or equal to the 95th percentile. All percentiles were age-, sex-, and height-dependent.
Weight was measured with an analog scale and expressed in kilograms.
Height was measured using a height rod attached to the scale and expressed in centimeters.
Lipid panel biochemical markers Cholesterol, triglycerides, high-density lipoprotein (HDL), LDL, lipoprotein(a) [Lp(a)], apolipoprotein A (ApoA), and apolipoprotein B (ApoB) were measured. Cholesterol/HDL, LDL/HDL and ApoB/ApoA ratios were calculated.
Data collection and management Data included a clinical history and measurements as well as laboratory tests. Blood pressure, weight, height and lipid marker results were recorded. Blood pressure was taken five times over the course of three days.
For laboratory tests, children were instructed to fast for 12 hours before venous blood draw. Their parents were also informed to help guarantee compliance. Blood was drawn from the antecubital vein, and serum was obtained following coagulation after centrifuging at 3000 rpm for 15 min. Serum concentrations of total cholesterol (TC) (Cholesterol liquicolor, CHOD-PAP Method, Human, Germany), triglycerides (TG) (Triglycerides GPO liquicolor, GPO-PAP Method, Human, Germany), and HDL cholesterol (HDL-c) (HDL-Cholesterol, Human cholesterol liquicolor test kit, Germany) were then determined. LDL cholesterol (LDL-c) was calculated using the Friedewald-Fredrikson formula: LDL-c = TC – (HDL-c + (TG/5)). Apolipoproteins B-100 and A1 were determined by immunoturbidimetry. The values were expressed in standard international units as mmol/L.
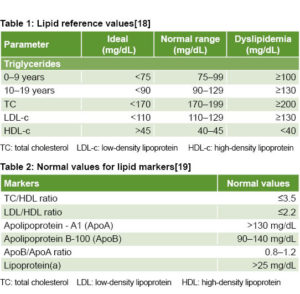
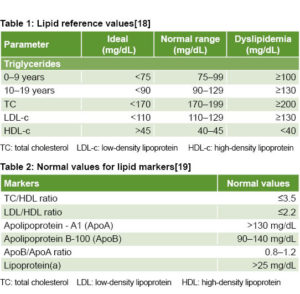
Lipid reference values (mg/dL) are presented in Table 1.[18]
Normal values for the remaining lipid markers are shown in Table 2.[19]
 Analysis Descriptive statistics, means and standard deviations in the lipid panel biochemical markers were used for each group. Tests for independence based on the chi-square statistic and its associated probability were used for qualitative variables, and mean comparison tests (ANOVA and its Kruskal Wallis nonparametric alternative) for quantitative variables. In all cases, the significance threshold was p = 0.05.
Analysis Descriptive statistics, means and standard deviations in the lipid panel biochemical markers were used for each group. Tests for independence based on the chi-square statistic and its associated probability were used for qualitative variables, and mean comparison tests (ANOVA and its Kruskal Wallis nonparametric alternative) for quantitative variables. In all cases, the significance threshold was p = 0.05.
Ethics Once the purpose of the study and the risks and benefits of participation had been explained to the children’s parents, they were asked to provide written consent in the presence of the investigator and a witness, in accordance with Declaration of Helsinki and WHO guidelines.[20,21] Since schoolchildren were involved, Ministry of Education authorization for the study was also obtained as required by Cuban law. All information obtained remained confidential, and in no case was the identity of a child disclosed. Choice of diagnostic media was based on material accessibility, care to maximize benefits for participants, the ethical norm of “do no harm,” and international and domestic guidelines established for good clinical and laboratory practices.
Results of physical examinations and diagnoses based on clinical and biochemical data obtained were provided to parents of participating children. When the examinations revealed health problems, appointments for medical followup were arranged with specialists, at the José Luis Miranda Pediatric Teaching Hospital in Santa Clara.
 RESULTS
RESULTS
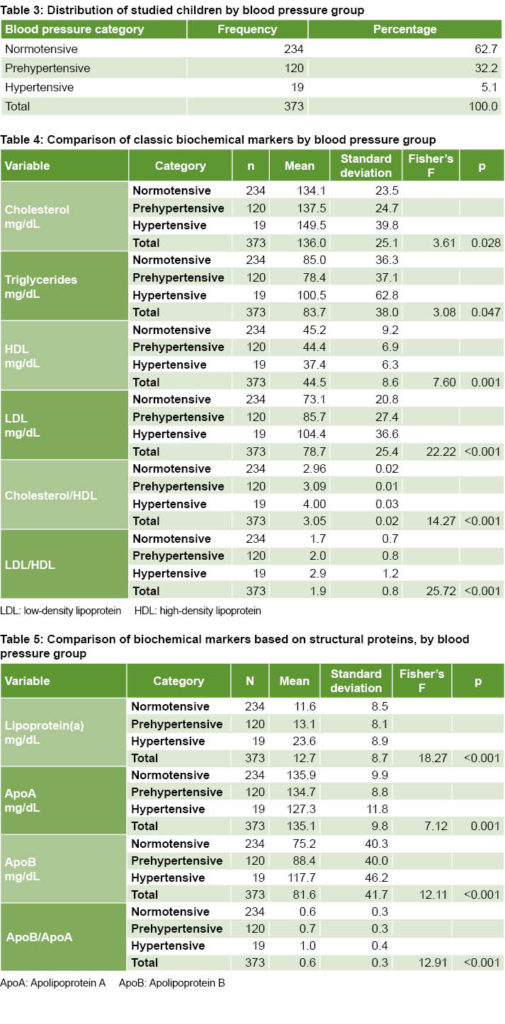
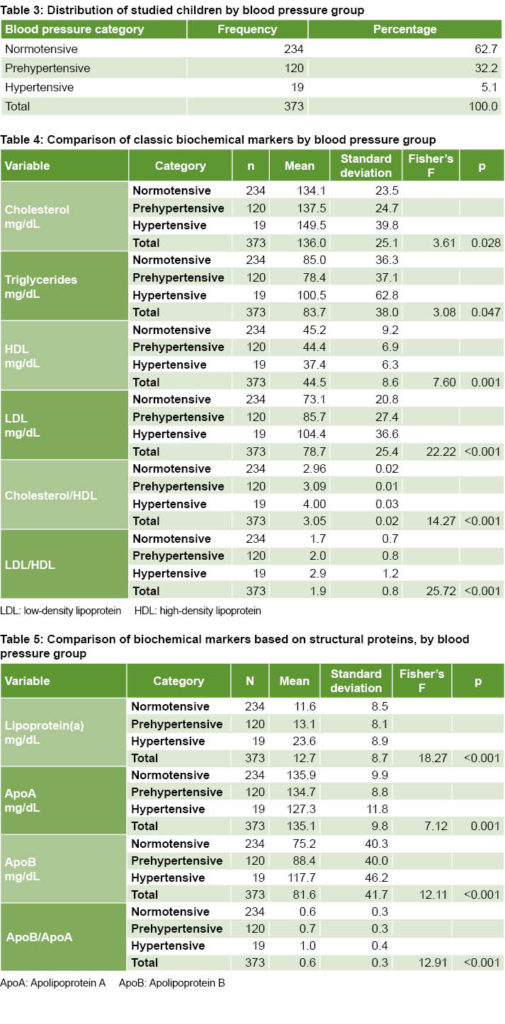
Although most of the children were classified as normotensive, a substantial percentage were hypertensive or prehypertensive (37.3%) (Table 3).
There were significant differences among groups (normotensive, prehypertensive and hypertensive) with respect to classic biochemical markers (Table 4). With the exception of triglycerides—which were higher in normotensive than in prehypertensive children—all indicators showed a monotonically decreasing pattern for HDL and an increasing pattern for the rest of the indicators, as expected.
All biochemical indicators based on the structural proteins of the lipoproteins also exhibited significant differences. With the exception of ApoA, higher values were found in the hypertensive children (Table 5).
DISCUSSION
The proportion of hypertensive and prehypertensive children in the sample exceeds the HT prevalence reported in Cuba for 2017.[11] The high percentage of prehypertensive children is a matter of concern. The global literature reports that progression of prehypertension to HT is approximately 7% per year and that prehypertension poses a high risk for development of HT in children,[22] making it a major challenge for the health system. Lipid alterations found in the prehypertensive children magnify the importance of this condition, underscoring the need to study lipid markers in these children and provide guidance on lifestyle changes to reduce risk of HT and CVD.
The association between serum cholesterol and blood pressure and between both variables and CVD has been confirmed by epidemiologic studies.[23,24] The higher cholesterol values we found in hypertensive and prehypertensive children are consistent with these results and alert to risk of atherosclerosis and CVD in early adulthood.
A close relationship between total serum cholesterol and CVD risk has been reported, along with the finding that changes in cholesterol concentrations through pharmacologic or lifestyle interventions are accompanied by changes in CVD incidence.[25,26] Based on these findings, clinicians and epidemiologists agree that total plasma cholesterol is a useful marker for predicting CVD.[24,27]
Although to a lesser extent than other classic biochemical indicators, triglycerides differed significantly among the groups, with higher concentrations in the hypertensive children. The lower triglyceride numbers in prehypertensive children may have been due to fat distribution, a characteristic not examined in this study. Some studies have shown that hypertriglyceridemia is more strongly associated with body fat distribution and diets rich in saturated fats than with alterations in blood pressure values.[28,29] High triglyceride values have been considered an independent CVD risk factor, although this remains a controversial issue and some authors question the independent nature of the relationship.[23,26]
The hypertensive and prehypertensive children had lower HDL values; according to the literature, therefore, they should be at higher risk of developing atherosclerosis and CVD. High HDL values are considered protective in the presence of hypertension.[28,30] Studies since the 1950s note that persons with high HDL concentrations are less likely to suffer from CVD. Coronary risk is estimated to decrease 2%–3% with a 1 mg/dL increase in HDL concentration.[23,25]
There were wide differences among the groups in terms of both LDL and the LDL/HDL ratio. These results are consistent with those of several studies showing an association between HT and high LDL, and reveal a direct association between high LDL values and CVD.[31,32]
High LDL concentrations in young adults predict appearance of CVD later in life; thus, the relationship between changes in LDL and the development of CVD is considered a continuous process that begins at an early age.[33,34] High values or an increase in values of this lipid marker in the hypertensive and prehypertensive children indicate higher risk of developing CVD in adulthood than in the normotensive children; therefore they need increased medical attention to control blood pressure and dyslipidemia.
Several studies show that high total cholesterol and LDL levels and the total cholesterol/HDL ratio are independently associated with a higher incidence of HT and CVD.[35–38] The prehypertensive and hypertensive children with elevated values for these markers in our study are at greater risk of developing CVD—one more reason to offer them specialized consultations for monitoring and followup.
Lp(a) values were higher in the hypertensive and prehypertensive children. While this is unrelated to HT in children, several studies[39–42] indicate that determining this marker helps identify children and adolescents at future risk of vascular disease, since high values are associated with higher thrombogenic capacity.
These studies also report that high Lp(a) concentrations are an independent CVD risk factor, even in the presence of normal concentrations of cholesterol and triglycerides.[40] Dalmau Serra[42] contends that the risk is higher for Lp(a) concentration in plasma above 30 mg/dL and is 2 to 3 times greater when it exceeds 50 mg/dL. Lp(a) concentrations normally show little variation throughout life, and in adulthood remain at levels similar to those in childhood. High Lp(a) concentrations have been reported in children with familial cardiovascular risk factors.[40] Determining this marker is useful, especially in children with an adverse lipid profile.
ApoA is the main constituent of high-density lipoproteins and higher levels are therefore associated with lower CVD risk.[39] ApoB is found in VLDL, LDL, IDL and lipoprotein remnants, all with atherogenic properties. Thus, high values in hypertensive and prehypertensive children are relevant when estimating the risk of CVD.[39] It has been suggested that low levels of ApoA1 and high levels of ApoB in young people, as found in the hypertensive and prehypertensive children in this study, could predict intimal thickening of the carotid artery in early adulthood and thus be associated with cardiovascular risk.[43] The ApoB/ApoA ratio accurately reflects the balance between atherogenic and antiatherogenic lipoproteins.[44,45] In the hypertensive and prehypertensive children studied, the balance favored atherogenic lipoproteins, denoting greater CVD risk.
An increase in ApoB levels and the ApoB/ApoA1 ratio, as well as a decrease in ApoA1, are better predictors of cardiovascular events than any other known risk factor, including high LDL concentrations.[46–49] Recent prospective studies show an association between ApoA1 and ApoB lipoprotein plasma levels and coronary artery disease, mainly in adults,[48,49] and suggest that the ApoB/ApoA ratio is the strongest predictor of this condition.[48,50] Studies in children are more scarce, but some supporting these results were conducted in Venezuela in 2004 by Fernández and in Spain in 2007 by Garcés and de la Oya.[51,52] This suggests that the hypertensive children in our study are at high risk of developing CVD in early adulthood.
CONCLUSIONS
The proportion of hypertensive and prehypertensive children is higher than previously reported, and their blood pressure values are associated with high values of lipid markers usually considered predictive of CVD. The most important biochemical markers associated with HT in these children were high values for LDL, LDL/HDL and ApoB/ApoA ratios and lipoprotein(a) concentrations. Our results point to the need to ensure monitoring and control of prehypertensive and hypertensive children and adolescents in Cuba.
References

- National Health Statistics and Medical Records Division (CU). Anuario Estadístico de Salud 2017 [Internet]. Havana: Ministry of Public Health (CU); 2018 [cited 2019 Jan 12]. 206 p. Available from: http://bvscuba.sld.cu/anuario-estadistico-de-cuba/. Spanish.
- Benjamin EJ, Virani SS, Callaway CW, Chang AR, Cheng S, Chiuve SE, et al. Heart disease and stroke statistics¾2018 update: a report from the American Heart Association [published online ahead of print January 31, 2018]. Circulation [Internet]. 2019 Mar 5 [cited Apr 10];139(10)e56–528. Available from: http://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000659?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed
- Rodríguez Domínguez L, Díaz Sánchez ME, Ruiz Álvarez V, Hernández Hernández H, Herrera Gómez V, Montero Díaz M. Factores de riesgo cardiovascular y su relación con la hipertensión arterial en adolescentes. Rev Cubana Med [Internet]. 2014 [cited 2019 Jan 12];53(1):25–36. Available from: http://scielo.sld.cu/pdf/med/v53n1/med04114.pdf. Spanish.
- Llapur Milián R, González Sánchez R. Comportamiento de los factores de riesgo cardiovascular en niños y adolescentes con hipertensión arterial esencial. Rev Cubana Pediatr [Internet]. 2006 Jan–Mar [cited 2019 Jan 12];78(1). Available from: http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S0034-75312006000100007. Spanish.
- Rothman KJ, Greenland S. Causation and causal inference in epidemiology. Am J Public Health [Internet]. 2005 [cited 2019 Jan 12];95 Suppl 1:S144–50. Available from: https://ajph.aphapublications.org/doi/pdf/10.2105/AJPH.2004.059204
- Núñez Robles E, Huapaya Pizarro C, Torres Lao R, Esquivel León S, Suárez Moreno EV, Yasuda Espinoza M, et al. Prevalencia de factores de riesgo cardiovascular y riesgo metabólico en escolares, universitarios y mujeres de organizaciones sociales de base en distritos de Lima, Callao, La Libertad y Arequipa, Perú 2011. Rev Perú Med Exp Salud Pública [Internet]. 2014 Oct–Dec [cited 2019 Jan 12];31(4):652–9. Available from: http://www.scielo.org.pe/scielo.php?script=sci_arttext&pid=S1726-46342014000400006. Spanish.
- Abraham CW, Blanco GH, Coloma G, Cristaldi A, Gutiérrez N, Sureda L. ERICA Estudio de los factores de riesgo cardiovascular en adolescentes. Rev Fed Arg Cardiol [Internet]. 2013 Jan–Mar [cited 2019 Jan 12];42(1):29–34. Available from: http://www.imbiomed.com.mx/1/1/articulos.php?method=showDetail&id_articulo=91549&id_seccion=4470&id_ejemplar=8978&id_revista=289. Spanish.
- Sáez Y, Bernui I. Prevalencia de factores de riesgo cardiovascular en adolescentes de instituciones educativas. An Fac Med [Internet]. 2009 Dec [cited 2019 Feb 20];70(4):259–65. Available from: http://www.scielo.org.pe/scielo.php?script=sci_arttext&pid=S1025-55832009000400006. Spanish.
- Briceño G, Céspedes J, Leal M, Vargas S. Prevalencia de factores de riesgo cardiovascular en escolares de un área rural y urbana de Colombia. Biomédica [Internet]. 2018 Dec 1 [cited 2019 Feb 20];38(4):545–54. Available from: https://www.revistabiomedica.org/index.php/biomedica/article/view/4223. Spanish.
- Medrano Donlucas G, Acosta Favela JA, Ruiz Morales ME, Vargas Esquivel JA. Principales factores de riesgo cardiovascular en escolares. Culcyt [Internet]. 2014 Sep–Dec [cited 2019 Feb 20];11(54):72–80. Available from: http://erevistas.uacj.mx/ojs/index.php/culcyt/article/viewFile/869/821. Spanish.
- National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescent. The Fourth Report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics [Internet]. 2004 [cited 2019 Jan 12];114(2 Suppl):555–76. Available from: http://pediatrics.aappublications.org/content/114/Supplement_2/555.long
- National Health Statistics and Medical Records Division (CU). Anuario Estadístico de Salud 2017 [Internet]. Havana: Ministry of Public Health (CU); c2018 [cited 2019 Jan 12]. Table 76, Prevalencia de diabetes mellitus, hipertensión arterial y asma bronquial según grupo de edad y sexo; p. 97. Available from: http://files.sld.cu/dne/files/2018/04/Anuario-Electronico-Espa%C3%B1ol-2017-ed-2018.pdf. Spanish.
- Zócalo Y, Arana M, García V, Mattos V, Curcio S, Farro I, et al. Estudios arteriales no-invasivos para detección temprana o valoración de cambios arteriales en niños y jóvenes expuestos a factores de riesgo cardiovascular y/o patologías sistémicas. Arch Pediatr Urug [Internet]. 2015 Sep [cited 2019 Feb 20];86(3):197–207. Available from: http://www.scielo.edu.uy/scielo.php?pid=S1688-12492015000300006&script=sci_arttext. Spanish.
- García Sánchez N. Sobre los indicadores bioquímicos del daño arterioesclerótico. Rev Cubana Aliment Nutr [Internet]. 2017 Jan–Jun [cited 2019 Jan 12];27(1):189–210. Available from: http://www.medigraphic.com/pdfs/revcubalnut/can-2017/can171m.pdf. Spanish.
- Benozzi S, Coniglio RI. Aterosclerosis: biomarcadores plasmáticos emergentes. Acta Bioquím Clín Latinoam [Internet]. 2010 Jul–Sep [cited 2019 Jan 20];44(3):317–28. Available from: http://www.scielo.org.ar/scielo.php?script=sci_arttext&pid=S0325-29572010000300003. Spanish.
- Ferrer Arrocha M, Fernández-Britto Rodríguez JE, Piñeiro Lamas R, Carballo Martínez R, Sevilla Martínez D. Obesidad e hipertensión arterial: señales ateroscleróticas tempranas en los escolares. Rev Cubana Pediatr [Internet]. 2010 Oct–Dec [cited 2019 Feb 20];82(4):20–30. Available from: http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S0034-75312010000400003. Spanish.
- Lurbe E, Cifkova R, Cruickshank JK, Dillon MJ, Ferreira I, Invitti C, et al. Management of high blood pressure in children and adolescents: recommendations of the European Society of Hypertension. J Hypertens [Internet]. 2009 Sep [cited 2019 Feb 20];27(9):1719–42. Available from: https://journals.lww.com/jhypertension/fulltext/2009/09000/Management_of_high_blood_pressure_in_children_and.1.aspx
- Sociedad Argentina de Pediatría Subcomisiones, Comités y Grupos de Trabajo. Consenso sobre manejo de las dislipidemias en pediatría. Arch Argent Pediatr [Internet]. 2015 [cited 2018 Feb 20];113(2):177–86. Available from: https://www.sap.org.ar/docs/publicaciones/archivosarg/2015/v113n2a23.pdf. Spanish.
- European Society of Hypertension-European Society of Cardiology Guidelines Committee. 2003 European Society of Hypertension-European Society of Cardiology guidelines for the management of arterial hypertension. J Hypertens [Internet]. 2003 Jun [cited 2018 Dec 10];21(6):1011–53. Available from: www.ncbi.nlm.nih.gov/pubmed/12777938
- World Medical Association. Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA [Internet]. 2013 Nov 27 [cited 2018 Dec 10];310(20):2191–4. Available from: https://jamanetwork.com/journals/jama/fullarticle/1760318
- van Delden JJM, van der Graaf R. Revised CIOMS International Ethical Guidelines for health-related research involving humans. JAMA [Internet]. 2016 Dec 6 [cited 2019 Feb 20]. Available from: http://redceih.bvs.hn/wp-content/uploads/2016/12/RevisedCIOMSGuidelines_JAMA_December2016.pdf
- Falkner B, Gidding SS. Prehipertensión en los adolescentes. Hypertension [Internet]. 2008 Dec [cited 2019 Feb 12];25(6):245–8. Available from: https://www.sciencedirect.com/science/article/pii/S0212824108757682. Spanish.
- O’Donnell CJ, Elosua R. Factores de riesgo cardiovascular. Perspectivas derivadas del Framingham Heart Study. Rev Esp Cardiol [Internet]. 2008 Mar [cited 2019 Feb 12];61(3):299–310. Available from: http://www.revespcardiol.org/es/factores-riesgo-cardiovascular-perspectivas-derivadas/articulo/13116658/. Spanish.
- Salazar Vázquez B, Rodríguez Morán M, Guerrero Romero F. Factores bioquímicos asociados a riesgo cardiovascular en niños y adolescentes. Rev Med IMSS [Internet]. 2005 Jul–Aug [cited 2019 Feb 20];43(4):299–303. Available from: http://www.medigraphic.com/pdfs/imss/im-2005/im054e.pdf
- Grupo Hipertensión; Deregibus M, Haag D, Ferrario C. Consenso sobre factores de riesgo de enfermedad cardiovascular en pediatría. Hipertensión arterial en niños y adolescentes. Arch Argent Pediatr [Internet]. 2005 [cited 2019 Feb 17];103(4):348–66. Available from: https://www.sap.org.ar/uploads/consensos/consenso-sobre-factores-de-riesgo-de-enfermedad-cardiovascular-en-pediatr-iacutea-hipertensi-oacuten-arterial-en-el-ni-ntildeo-y-el-adolescente-hipercolesterolemia.pdf. Spanish.
- Sarwar N, Danesh J, Eiriksdottir G, Sigurdsson G, Wareham N, Bingham S, et al. Triglycerides and the risk of coronary heart disease: 10,158 incident cases among 262,525 participants in 29 Western prospective studies. Circulation [Internet]. 2007 Jan 30 [cited 2019 Feb];115(4):450–8. Available from: https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.106.637793
- Gotthelf SJ, Jubany LL. Prevalencia de factores de riesgo cardiovascular en adolescentes de escuelas públicas y privadas de la ciudad de Salta, año 2009. Arch Argent Pediatr [Internet]. 2010 Sep–Oct [cited 2019 Feb 17];108(5):418–26. Available from: http://www.scielo.org.ar/scielo.php?script=sci_arttext&pid=S0325-00752010000500007. Spanish.
- Halperin RO, Sesso HD, Ma J, Buring JE, Stampfer MJ, Gaziano JM. Dyslipidemia and the risk of incident hypertension in men. Hypertension [Internet]. 2006 Jan [cited 2019 Feb 20];47(1):45–50. Available from: https://www.ahajournals.org/doi/full/10.1161/01.HYP.0000196306.42418.0e?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed
- Royo-Bordonada MA, Garcés C, Gorgojo L, Martín-Moreno JM, Lasunción MA, Rodríguez Artalejo F, et al. Saturated fat in the diet of Spanish children: relationship with the anthropometrical, alimentary, nutritional and lipid profiles. Public Health Nutr [Internet]. 2006 Jun [cited 2019 Feb 20];9(4):429–35. Available from: https://www.cambridge.org/core/product/identifier/S1368980006000759/type/journal_article
- Escudero-Lourdes GV, Morales-Romero LV, Valverde-Ocaña C, Velasco-Chávez JF. Riesgo cardiovascular en en población infantil de 6 a 15 años con obesidad exógena. Rev Med Inst Mex Seguro Soc [Internet]. 2014 [cited 2019 Feb 20];52(Suppl 1): S58–63. Available from: http://www.medigraphic.com/pdfs/imss/im-2014/ims141j.pdf. Spanish.
- Sáez Y, Bernui I. Prevalencia de factores de riesgo cardiovascular en adolescentes de instituciones educativas. An Fac Med [Internet]. 2009 [cited 2019 Jan 12];70(4):259–65. Available from: http://www.scielo.org.pe/pdf/afm/v70n4/a06v70n4.pdf. Spanish.
- Romero Velarde E, Campollo Rivas O, Celis de la Rosa A, Vásquez-Garibay EM, Castro-Hernández JF, Cruz-Osorio RM. Factores de riesgo de dislipidemia en niños y adolescentes con obesidad. Salud Pública Mex [Internet]. 2007 Mar–Apr [cited 2019 Jan];49(2):103–8. Available from: https://scielosp.org/pdf/spm/2007.v49n2/103-108/es. Spanish.
- Cuartas S, Pérez Torre M. Evaluación comparativa entre el colesterol no-HDL y el colesterol-LDL en niños y adolescentes. Rev Cubana Pediatr [Internet]. 2017 [cited 2019 Jan 12];89(1):20–9. Available from: http://scielo.sld.cu/pdf/ped/v89n1/ped04117.pdf. Spanish.
- Leguen-Gulgar L, Castellanos M, Sánchez-Bouza MJ, Benet-Rodríguez M. Factores de riesgo cardiovasculares y su relación con las alteraciones del metabolismo de los glúcidos y lípidos. Rev Finlay [Internet]. 2014 Dec [cited 2018 Dec 17];4(4):248–60. Available from: http://www.revfinlay.sld.cu/index.php/finlay/article/view/326. Spanish.
- LLapur Milián R, González SR, Borges Alfonso K, Rubio Olivares DY. Alteraciones lipídicas en la hipertensión arterial esencial. Rev Cubana Pediatr [Internet]. 2013 [cited 2018 Dec];85(3):283–94. Available from: http://bvs.sld.cu/revistas/ped/vol85_3_13/ped02313.htm. Spanish.
- Galarza Carrión GE. Adolescencia e hipertensión arterial. Rev Ciencias Méd [Internet]. 2014 Sep–Oct [cited 2019 Feb];18(5):743–52. Available from: http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S1561-31942014000500004. Spanish.
- Real Delor R, Duarte SE, López Encarnación N. Factores de riesgo cardiovascular en adolescentes de una ciudad del Paraguay. Acta Med Colomb [Internet]. 2017 [cited 2019 Feb 20];42(1):30–4. Available from: http://www.scielo.org.co/pdf/amc/v42n1/0120-2448-amc-42-01-00030.pdf. Spanish.
- Calandrelli M, Saavedra ME, Trevisán M, Zgaib ME, Parola M, Ferrante D. Relevamiento de factores de riesgo cardiovascular en Bariloche. Rev Argent Cardiol [Internet]. 2011 Aug [cited 2019 Jan];79(4):344–50. Available from: http://www.scielo.org.ar/scielo.php?script=sci_arttext&pid=S1850-37482011000400007. Spanish.
- Ruiz Mori E. Riesgo y Prevención Cardiovascular [Internet]. [place unknown]: [publisher unknown]; [cited 2018 Dec 17]. 135 p. Available from en: http://www.sscardio.org/wp-content/uploads/2016/11/RIESGO-CARDIOVASCULAR-V44-copia.pdf. Spanish.
- González-Requejo A, Sánchez-Bayle M, Ruiz-Jarabo C, Asensio Antón J, Peláez MJ, Morales MT, et al. Lipoprotein(a) and cardiovascular risk factors in a cohort of 6 year old children. The Rivas-Vaciamadrid study. Eur J Pediatr [Internet]. 2003 Sep [cited 2019 Jan];162(9):572–5. Available from: http://www.elsevier.es/index.php?p=revista&pRevista=pdf-simple&pii=S0214916804789962&r=8
- Sáez Meabe Y, Lafita Bernar M, Sáez de Lafuente Chivite JP, Narváez Gofinondo I, Vacas Rius M, Magro López AM, et al. Correlación de los perfiles lipoproteicos y variables antropométricas con concentraciones séricas de lipoproteína(a) en la infancia. An Pediatr [Internet]. 2006 Mar [cited 2019 Jan];64(3):221–326. Available from: http://www.analesdepediatria.org/es-correlacion-los-perfiles-lipoproteicos-variables-articulo-resumen-13085509. Spanish.
- Dalmau Serra J. Nuevos factores de riesgo cardiovascular detectables en la edad pediátrica. An Esp Pediatr [Internet]. 2001 May [cited 2019 Jan];54(3):1–72. Available from: http://www.analesdepediatria.org/es-nuevos-factores-riesgo-cardiovascular-detectables-articulo-13012919. Spanish.
- Álvarez Caro F, Díaz Martín JJ, Riaño Galán I, Pérez Solís D, Venta Obaya R, Málaga Guerrero S. Factores de riesgo cardiovascular clásico y emergente en escolares asturianos. An Pediatr [Internet]. 2011 Jun 1 [cited 2019 Feb 15];74(6):388–95. Available from: https://doi.org/10.1016/j.anpedi.2011.01.007. Spanish.
- Torres-Colores J, González-Bárcena D, Muñoz-Solís A. Relación apolipoproteína B/Apolipoproteína AI y componentes del síndrome metabólico en adolescentes con obesidad: Efecto de una dieta hipocalórica baja en carbohidratos. Acta Médica Grupo Ángeles [Internet]. 2006 Apr–Jun [cited 2019 Jan];4(2):81–8. Available from: http://www.medigraphic.com/pdfs/actmed/am-2006/am062a.pdf. Spanish.
- Moreira Lima L, Carvalho MG, Sousa Oliveira M. Índice apo B/apo A-I e predição de risco cardiovascular. Arq Bras Cardiol [Internet]. 2007 [cited 2019 Jan 12];88(6):140–3. Available from: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0066-782X2007000600014&lng=pt&nrm=iso&tlng=pt. Portugues, English.
- Sierra-Johnson J, Fisher RM, Romero Corral A, Somers VK, López Jiménez F, Öhrvik J. Concentration of apolipoprotein B is comparable with the apolipoprotein B/apolipoprotein A-I ratio and better than routine clinical lipid measurements in predicting coronary heart disease mortality: findings from a multi-ethnic US population. Eur Heart J [Internet]. 2009 Mar [cited 2019 Feb 20];30(6):710–7. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2721712/
- Vélez C, Gil LM, Ávila CL, López A. Factores de riesgo cardiovascular y variables asociadas en personas de 20 a 79 años en Manizales, Colombia. Rev Univ Salud [Internet]. 2015 [cited 2019 Feb];17(1):32–46. Available from: http://www.scielo.org.co/pdf/reus/v17n1/v17n1a04.pdf. Spanish.
- Graffigna M, Soutelo J, Catoira N, Azpelicueta AM, Perel C, Aranguren M, et al. Alteraciones lipídicas en adolescentes de peso adecuado. Insuf Card [Internet]. 2017 Dec [cited 2019 Jan 15];12(4):153–9. Available from: http://www.scielo.org.ar/scielo.php?script=sci_arttext&pid=S1852-38622017000400003. Spanish.
- Castillo Arocha I, Armas Rojas NB, Dueñas Herrera A, González Greck OR, Arocha Mariño C, Castillo Guzmán A. Riesgo cardiovascular según tablas de la OMS, el estudio Framingham y la razón apolipoproteína B/apolipoproteína A1. Rev Cubana Invest Bioméd [Internet]. 2010 Oct–Dec [cited 2019 Jan];29(4):479–88. Available from: http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S0864-03002010000400008&lng=es. Spanish.
- Moreira Lima L, Carvalho MG, Sousa Oliveira M. Índice apo B/apo A-I e predição de risco cardiovascular. Arq Bras Cardiol [Internet]. 2007 [cited 2019 Jan];88(6):e187–e90. Available from: http://dx.doi.org/10.1590/S0066-782X2007000600014. Portugues, English.
- Fernández V, Morales LM, Molero-Conejo E, Casanova A, Campos G, Raleigh X, et al. Niveles de Apoproteínas B, A-I y CIII como marcadores de riesgo cardiovascular en adolescentes delgados y obesos. Invest Clin [Internet]. 2004 [cited 2019 Jan];45(1):29–42. Available from: https://www.researchgate.net/publication/262665511_Niveles_de_Apoproteinas_B_A1_y_CIII_como_Marcadores_de_riesgo_Cardiovascular_en_adolescentes_delgados_y_obesos. Spanish.
- Garcés C, de Oya M. Factores de riesgo cardiovascular en la edad infantil. Resultados globales del estudio Cuatro Provincias. Rev Esp Cardiol [Internet]. 2007 May [cited 2019 Feb 20]; 60(5):517–24. Available from: http://www.revespcardiol.org/es/factores-riesgocardiovascular-edad-infantil-/articulo/13106185/. Spanish.
THE AUTHORS
Merlin Garí-Llanes (Corresponding author: merlingll@infomed.sld.cu), physician with dual specialties in cardiology and family medicine, and a master’s degree in comprehensive pediatric care. Associate professor of pediatric cardiology, José Luis Miranda Pediatric Teaching Hospital (HPJLM), Santa Clara, Cuba.
Yosvany García-Nóbrega, cardiologist and assistant professor of pediatric cardiology, HPJLM, Santa Clara, Cuba.
Elibet Chávez-González, cardiologist with a doctorate in medical sciences. Associate professor of electrophysiology and cardiac stimulation, Ernesto Che Guevara Heart Center, Santa Clara, Cuba.
Emilio González-Rodríguez, electrical engineer with a doctorate in technical sciences. Electrical Engineering Department, Electronic Development Center, Marta Abreu of Las Villas Central University, Santa Clara, Cuba.
Julieta García-Sáez, endocrinologist and assistant professor of pediatric endocrinology, HPJLM, Santa Clara, Cuba.
María del Carmen Llanes-Camacho, pediatrician with a master’s degree in comprehensive pediatric care. Consulting professor of pediatric cardiology, HPJLM, Santa Clara, Cuba.
Submitted: October 26, 2018 Approved: April 23, 2019 Disclosures: None