INTRODUCTION
Use of addictive substances has evolved through two modalities: as part of religious ceremonies and in secular communal use associated with eating and interpersonal relationships.[1] Tobacco and alcohol use are especially relevant to global public health because of the wide range of consequent illnesses and injuries and the many social and legal problems they provoke. Both substances are presently included among the principal causes of preventable morbidity, mortality and disability at national and international levels.[2] Besides their association with the main types of cancer, they can lead to hepatic cirrhosis, fetal damage, hypertension, gastritis, diabetes, stroke, depression, traffic accidents, falls and work problems.[3] Their increasing use among adolescents and youth in many countries[4] is worrisome because of the seriousness of the health problems they cause and their significant social impact.
Researchers at the Scientific and Technological Development Unit (CEDRO, the Spanish acronym) of the Medical University of Havana (UCMH, the Spanish acronym) and the scientific research department of the School of Nursing and Public Health at the Michoacan University of Saint Nicholas of Hidalgo (UMSNH, the Spanish acronym) in Morelia, Mexico, have been collaborating in applied research on addictions since 2011. Following an initial meeting at the 4th International Congress on Health and Quality of Life in Holguín, Cuba in April 2011, we have continued to publish jointly and co-present at events and workshops in Mexico and Cuba.[5]
This study is the result of our mutual interest in identifying levels of addiction risk in the professionals we are educating and also expresses our shared commitment to ensuring that the scourge of drugs does not affect those who have professional and human responsibility for the public’s mental health—through health promotion, disease prevention, and patient rehabilitation and social reinsertion.
Tobacco Smoking at the global level has increased substantially since World War II, especially among women and youth.[6] Tobacco smoke is a gas with >500 components as well as >3500 water-soluble compounds, including nicotine, which is both addictive and toxic. Nicotine reaches the brain as fast as five seconds after smoke is inhaled.[7] According to WHO, smoking has become a genuine epidemic affecting billions of people globally. Its high prevalence in countries such as Mexico and Cuba is alarming. Tobacco use is considered one of the preventable risk factors most responsible for the two main causes of death in the world: cardiovascular diseases and cancer.[8]
In Latin America, 15% of deaths are smoking related.[4] Smoking, unhealthy eating and physical inactivity form a toxic triad that plays a key role in the occurrence of chronic non-communicable diseases.[9] Because bystanders are also exposed, the smoking epidemic affects the health of the entire population, not just smokers themselves.
Mexico has an addictions surveillance system (SISVEA, the Spanish acronym) that guides public health policies and assesses effectiveness of control strategies for tobacco and other drugs.[10] In recent years, nearly 13 million Mexicans were reported to have smoked more than 100 cigarettes in their lives, constituting a national epidemic. Annually, more than 53,000 Mexicans die from smoking-related diseases.[11] On average, Mexico’s adolescent smokers begin smoking at 13.7 years, and the two most common reasons given for doing so are curiosity and cohabitation with smokers.[12]
National risk factor surveys in Cuba also show a high prevalence of tobacco use that has alarmed health authorities. Prevalence in Cuban women, who have not traditionally smoked in large numbers, is now approximately 22.3%.[13] Five of the first seven causes of death in Cuba are related to lifestyle and substance use, smoking one of the most important risk factors.[14] In recent years there have been reports of increased use of psychoactive substances by Cuban medical students. This trend is especially evident in early initiation and increased smoking by both sexes.[15,16] Age of smoking initiation is falling and is now estimated at approximately 12 years.[17] A similar picture is seen in university students in nonmedical programs. A study conducted on a municipal campus of the University of Havana concluded that approximately one third of students assessed were at risk of addiction; more than half also reported being subject to stress and having an external locus of control.[18]
Smoking in Cuban hospitals and medical schools is a common sight, despite regulations prohibiting it. The majority of health personnel who smoke are service workers, but professionals and students often smoke as well.[19] In these cases, smoking cessation is an ideal way to reduce individual harm and improve health educators’ effectiveness.
Alcohol WHO defines alcoholism as a chronic behavior disorder characterized by dependence on alcohol and manifest in inability to abstain from drinking and/or to stop drinking once started.[20] A steady increase has been observed in the number of persons addicted to alcohol in the Americas. However, while the social costs related to alcohol dependence are great, the social costs of harmful alcohol use by nondependent drinkers are even greater.[21]
The typical pattern of alcohol use in Mexico involves occasional drinking but of large quantities.[12] Adolescents in Mexico appear to be copying the adults’ model and a substantial number are problem drinkers. There has been a notable increase in drinking among adolescent women. According to Mexico’s National Addictions Survey, an important proportion of the population requires treatment and an even larger proportion needs to learn to moderate their alcohol intake and avoid binge drinking.[12]
In Cuba, 45.2% of the population aged >15 years consumes alcoholic beverages, predominantly in the group aged 15–44 years. Alcohol use has increased notably in the last 15 years; the majority of problem drinkers are aged 25–42 years.[22] This tendency is also seen in groups traditionally less vulnerable to alcohol abuse; for example, prevalence of alcohol use in women is approximately 10.4%.[13] There is a trend to take up drinking at ever younger ages, with the estimated age of initiation at approximately 15 years.[17]
Harmful use of alcohol has become a social problem in Cuba with major repercussions in family and work spheres, leading to violence, divorce, and reduced productivity because of tardiness and absenteeism. The individual may suffer from psychopathological symptoms—such as anxiety, depression, sleep disorders—and a lack of knowledge of the disease.[23] In certain sectors, alcohol consumption during the work week is increasingly frequent, and there has been a perceptible increase in tolerance of drinking in parks and plazas on holidays and weekends, despite its illegality in those venues.[24]
The aforementioned increase in use of psychoactive substances by Cuban medical students is also evident in worrisome drinking patterns in terms of amount ingested, frequency of light inebriation and money spent on alcoholic beverages.[15,16]
The objective of this study was to identify the prevalence of tobacco and alcohol use by health sciences students in Mexico and Cuba, in order to support educational interventions to promote healthy lifestyles and develop professional competencies to reduce the harmful impact of these legal drugs on public health in these countries.
METHODS
A descriptive cross-sectional study was conducted using quantitative and qualitative techniques (the latter for more in-depth analysis of the most relevant quantitative results) of students enrolled in UMSNH School of Nursing and Public Health and the Manuel Fajardo Medical Faculty at UCMH in the 2011–2012 academic year. The sites were chosen for feasibility. A pilot study was first conducted with 27 of the 31 first-year medical students in the same academic year at the Artemisa Medical School satellite campus in San Antonio de los Baños, Cuba. Results of the protocol were satisfactory, and thus no modifications were introduced.
The study universe consisted of 1516 undergraduate nursing and public health students in UMSNH’s School of Nursing and Public Health and 1481 medical students in the Manuel Fajardo Medical Faculty at UCMH. A convenience sample was collected of all students who attended classes at the time and date indicated, and who satisfied inclusion criteria (stable attendance at academic activities and willingness to participate in the study). Participants included 117 students in Mexico and 108 students in Cuba.
Variables Demographic variables were age and sex.
Tobacco use: dichotomous variable determined by Yes/No response to question whether the subject was a smoker.
Nicotine dependence level: definition based on the three Fagerström levels of dependence:
Minimally dependent: 0–4 points
Moderately dependent: 5–6 points
Highly dependent: ≥7 points[25]
Exposure to environmental tobacco smoke (ETS): Dichotomous variable determined by Yes/No response to whether subject was habitually exposed to a smoker’s tobacco smoke.
Alcohol use: dichotomous variable determined by Yes/No response to whether the subject ingested alcoholic beverages.
Hazardous use of alcohol: consumption of >2 drinks containing alcohol on a typical day (1 drink = 10 g pure alcohol).
Frequency of alcohol use: categorical variable with categories never, ≤1 time per month, 2–4 times per month, 2–3 times per week, ≥4 times per week.
Risk level of alcohol use: Definition based on risk levels defined in the Alcohol Use Disorders Identification Test (AUDIT):[26]
Low risk: 0–7 points (Zone I)
Hazardous use: 8–15 points (Zone II)
Harmful use: 16–19 points (Zone III)
Alcohol dependent: ≥20 points (Zone IV)
Data collection Health sciences students in Mexico and Cuba completed an anonymous voluntary self-administered questionnaire containing 22 questions, including 6 questions from the Fagerström Test for Nicotine Dependence (FTND),[25] and 10 from AUDIT.[26] Questions included the subject’s age when he/she started smoking and his/her level of consumption (Have you ever smoked? Have you smoked more than 100 cigarettes in your life?); possible exposure to ETS (Do you live with someone who smokes?); and knowledge about pertinent legislation in effect (Is the sale to minors of products such as cigarettes prohibited by any law in your country, state, or municipality?). Finally there were two questions to evaluate cooperation level while responding to the questionnaire (How do you feel after completing this questionnaire? Would you be willing to answer this questionnaire again or another if requested?).
FTND is a self-administered six-item questionnaire on consumption of cigarettes, designed to evaluate nicotine dependence, a revised version of the eight-item Fagerström Tolerance Questionnaire published in 1978.[27] Nicotine dependence is an ordinal qualitative variable. It is defined as the state of adaptation manifested in intense physical and psychological disorders when administration of nicotine is withdrawn.[28] It is expressed based on the fact that consumption produces a sensation of satisfaction and a psychic impulse that requires periodic or continuous administration in order to obtain pleasure or prevent discomfort.
The AUDIT test is a ten-item self-administered questionnaire based on a WHO project in six countries (Australia, Bulgaria, Kenya, Mexico, Norway and the USA).[26] It is a sensitive instrument used as a screening technique and capable of detecting less serious problems related to alcohol use. Questions 1–3 concern amount consumed; questions 4–6 are about drinking behavior and attitudes; 7 and 8 refer to adverse reactions; and the last 2 questions cover problems related to alcohol use. All questions are limited to events during the last year.
Finally each subject was interviewed, keeping in mind the questionnaire findings but avoiding leading questions so that opinions and attitudes could emerge spontaneously. Interview objectives were to elicit more contextual detail than could be obtained from questionnaire responses and to further explore opinions and attitudes toward alcohol and tobacco use.
Questionnaire responses were entered in a database using SPSS Version 17. Means and percentages were calculated for quantitative and qualitative variables, respectively. Interview data were analyzed manually in an iterative process of synthesis, distillation and categorization; the categories were then validated by respondents, refined, coded and cross-linked.
Ethics The study was approved by the research ethics committees of the two institutions involved. All participants provided written informed consent.
RESULTS
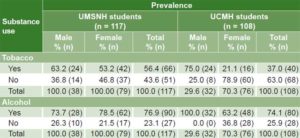
Tobacco The average age of the 117 Mexican students surveyed was 24 years and of the 108 Cuban students 18.7 years; in both cases the majority of students were women. Prevalence of smoking was 56.4% in Mexican students and 37% in Cubans. Prevalence of alcohol use in Mexican students was 76.9%; in Cubans, 74.1% (Table 1).
Table 1: Prevalence of tobacco and alcohol use in health sciences students, UMSNH (Mexico) and UCMH (Cuba)
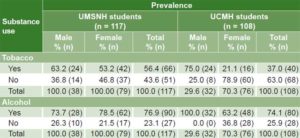
UCMH: Medical University of Havana UMSNH: Michoacan University of Saint Nicholas of Hidalgo
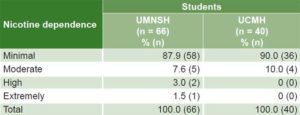
Minimal nicotine dependence per FTND was present in 87.9% (58/66) of Mexican students who smoked (49.6% of all Mexican students) while 12.1% were at least moderately dependent. Among Cuban student smokers, 90% (36/40, or 33.3% of total) reported minimal nicotine dependence and 10% (4/40, or 3.7% of total) were moderately dependent (Table 2).
Table 2: Nicotine dependence* among student smokers, UMSNH (Mexico) and UCMH (Cuba) (n = 106)
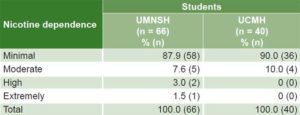
UCMH: Medical University of Havana UMSNH: Michoacan University of Saint Nicholas of Hidalgo , *per Fagerström Test for Nicotine Dependence[26]
Interview analysis found that tobacco use and exposure to ETS in public and private places were similar in both contexts. About 60% of subjects in both samples reported that they lived with a smoker and were involuntarily exposed to tobacco smoke, citing criteria such as “I hang out with friends who smoke,” “Wherever I go people are smoking,” “Smoking is accepted as normal,” “My parents and other close relatives smoke at home,” etc.
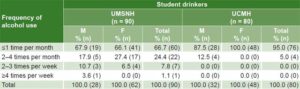
Alcohol Approximately 76.9% (90/117) of Mexican students consumed alcohol, with little difference between men and women (73.7% and 78.5%, respectively). All the Cuban men (32/32) consumed alcohol, as did 63.2% of the women (48/76) (Table 1). Among those who consumed alcohol, two thirds of the Mexican students, both men and women, consumed alcohol ≤1 time per month (67.9% and 66.1%, respectively). Among the Cubans, drinking frequency tended to be lower, with 87.5% of men and all women drinking ≤1 time per month; none more than 2–4 times per month (Table 3). Among Cuban students, 70.3% reported they occasionally consumed alcoholic beverages on weekends. They also specified that on average they drank once a month during recreational activities.
Table 3: Frequency of alcohol use among student drinkers, UMSNH (Mexico) and UCMH (Cuba) (n = 170)
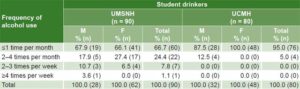
UCMH: Medical University of Havana UMSNH: Michoacan University of Saint Nicholas of Hidalgo
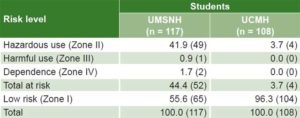
Table 4: Distribution of risk* from alcohol use among health sciences students, UMSNH (Mexico) and UCMH (Cuba) (n = 225)
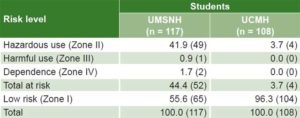
UCMH: Medical University of Havana UMSNH: Michoacan University of Saint Nicholas of Hidalgo *per Alcohol Use Disorders Identification Test[27]
In both groups the majority reported minimal consumption levels, but 44.4% of Mexican students’ were classified as at-risk drinkers (Zone II or higher per AUDIT) (Table 4).
DISCUSSION
Tobacco The high prevalence of smoking in Mexican health sciences students is cause for concern. It corresponds with early onset of tobacco use nationally, which has being a major health problem in Mexico. A high percentage of the adult population that smokes or has smoked began the habit between 10 and 19 years of age.[12] The student population has begun smoking at ever younger ages.
This situation will most likely not improve while there continue to be violations of stipulations established in Article 277 of Chapter XI of the General Health Law, prohibiting the sale of tobacco products to minors and availability of such products in pharmacies, hospitals and schools. It also establishes smoke-free areas in health facilities, classrooms, workplaces and mass transit.[29] In order to prevent exposure to ETS, which affects the health not only of active but also passive smokers, that law needs to be better enforced.
As for Cuban students, more than one third had also begun smoking at early ages. Thus, results of our study mirror global patterns in which adolescents generally begin to consume tobacco at a very young age, which increases the risk of developing related problems.[12] Once hooked in youth, the addiction is very hard to overcome. Youth is the life stage of most intense educational and professional development, and both can be affected by tobacco use. Evidence suggests early diagnosis and prompt intervention are vital.[29]
Smoking has become a priority problem for health authorities in Cuba. There are frequent violations of the regulations established by the Ministry of Public Health (MINSAP, the Spanish acronym) prohibiting smoking in health institutions, including medical universities. Ministerial Regulation 360 of 2005[30] prohibits smoking or keeping any tobacco product lit in all institutions of the national health system, except in open spaces outside the institution during a coffee or lunch break as established by labor regulations. Systematic violations of established regulations impede tobacco control in a nation that has admirable health indicators in other areas. Social indiscipline and indifference to regulations are obstacles that prevent both the public and health workers and students from recognizing the significant risks of tobacco exposure.
Besides MINSAP, other state bodies have also enacted related regulations. For example, Ministerial Resolution 335 of 2004[30] of Cuba’s Ministry of Domestic Trade expressly prohibits sale to minors (aged <16 years) of cigarettes—in packages or singly—or cigars. It is noteworthy that Cuban students frequently admitted being unaware of these laws, which does not help them comply.
Health institutions—especially health sciences education centers training tomorrow’s health professionals—should use evidence from this study to expand strategies to control tobacco use and exposure to ETS, and to enforce regulations prohibiting smoking in public places and other enclosed spaces. The sale of tobacco products to minors should be more strictly controlled, and direct and indirect publicity of tobacco products prohibited in practice. These measures should reduce tobacco use and encourage creation of smoke-free environments.
The smoking patterns we observed in Cuban and Mexican health sciences students are not unique, as reflected in a study in Spain that found such students to smoke at similar rates to the overall population.[31] The public will look to them as role models, and their tobacco use may mislead others to view active consumption of tobacco and exposure to ETS as unimportant issues for public health. This deprives them of an opportunity to influence the population by example.
Alcohol Our findings that the majority of Mexican students drank but with relatively low frequency coincide with those of the the National Addictions Survey in Mexico, which reported moderate frequency, but of large amounts, and that consumption progressively increases with age. Our study showed that occasional binge drinking persists in this Mexican student population.
The one third of students who reported drinking more than once a month are candidates for education to maintain moderate intake and prevent binge drinking, with its attendant social, family, and personal problems. Only three students were identified as needing treatment for dependent or harmful use.
While the proportion of Cuban students who had initiated alcohol use was similar to the Mexican students, more Cubans drank less than once a month. Overall prevalence of alcoholism in Cuba is estimated at 5% in individuals aged >15 years.[32] While this is lower than in many countries in the region, undesirable consumption patterns do exist.[18] Systematic casefinding of alcoholism in a Havana polyclinic catchment area in 2011 found a higher percentage of alcoholics than suggested by surveillance reports.[33] Our results reflect this reality. While the Cuban students reported relatively low alcohol consumption, most began drinking before age 16 and they often responded that they did it for fun or to relieve the stress of their studies.
As was the case for tobacco, the young age at drinking onset in Cuba also indicates systematic violations of alcohol regulations;[17] specifically, Ministerial Resolution 334 of 2004 of Cuba’s Ministry of Domestic Trade prohibits sale of alcoholic beverages to minors (aged <16 years) in any type of establishment, public or private, regardless whether in pesos or freely convertible currency.[30]
The situation described is not unique to these countries. For example, a Colombian study found that 85% of young people (aged 20–25 years) had consumed alcohol at some point in their lives and a similar proportion (80.4 %) had done so in the previous year, and approximately half the youth studied had consumed alcohol in the previous month. Percentages were higher among university students, 94.6% of whom had tried alcohol and 94.6% of whom were consumers at the time of the study.[34]
This study was of two specific populations and is not meant to be generalized to all young people or even all health sciences students in Mexico and Cuba. Our intention was simply to describe the extent of tobacco and alcohol use in these two groups of health sciences students. In addition, comparisons between the two student populations should be made with caution because Cuban students were on average over five years younger than the Mexican students. Based on our findings, we are working to fulfill the main recommendation resulting from the study, which is to support educational interventions to promote healthy lifestyles and develop professional competencies for drug abuse prevention. The authorities of the two universities have undertaken actions to address the problem of student alcohol and tobacco use. For example, UCMH created CEDRO to be a center for addiction prevention through education, research, and university extension.[35]
CONCLUSIONS
This study constitutes the first step in a joint approach to a priority problem in both universities. Addictive behaviors not only can cause students to drop out of school, but can also limit development of general and specific professional competencies to prevent abuse of these drugs and other addictions in the broader population. Strategies to modify and reduce alcohol use are needed, and these should involve families, professors and students themselves, since they are the future health professionals charged with reducing the impact of abuse of these drugs in their countries.