INTRODUCTION
In recent decades, analysis of the health–illness process has been challenged to find indicators that complement traditional indicators centered on mortality and morbidity, and that incorporate self-assessment of health and well-being. This has led to development of theory and methods to study health-related quality of life (HRQOL), the sense of well-being derived from the subjective assessment of one’s own health status.[1,2] Introduction of this concept and the proliferation of instruments for measuring it have become very important due to its association with indicators of mortality, hospitalization and health service utilization.[3]
A person’s subjective appreciation of their own health depends on their economic, cultural and social context.[2,4,5] One analytical approach to context-related interindividual differences focuses on the influence of social determinants of health, and suggests that people experience distinct exposures and vulnerabilities according to their socioeconomic status (SES), which condition their opportunities as well as their health status.[6,7] Research on the association between SES stratifiers and HRQOL is of particular interest, as are the mechanisms by which SES influences subjective health assessment. Although the social determinant approach has been broadly applied to studying population health status, it lacks quantitative models for explaining constructs such as perceived health, in which attitudes and socialization processes (the moods, emotions, memories and beliefs that health as the object of assessment arouses in the subject) also play a role.[8]
Several studies explain the relationship of health status to conditioning factors such as education,[9,10] employment[9–13] and income,[12,14] but there are few studies of the association between SES indicators and HRQOL. Some show poorer well-being in persons with lower levels of education,[4,15] and a similar association with HRQOL.[16–18] Other studies show an association between employment status and well-being,[15] as well as a worse perception of health in retired or unemployed persons.[16,19] Some studies also examine the relationship between income and well-being[4,9,15] and HRQOL.[5,16–19]
In Chile, several studies have applied one of the generic surveys most frequently utilized to measure HRQOL, the SF-12 Short Form Survey (abbreviated from a 36-item survey).[20] This instrument was used for the first time in Chile in the Second Health and Quality of Life Survey (2006), which found significant differences in perceived health between the highest and lowest socioeconomic groups.[21] The SF-12 was used again in the 2010 Second National Health Survey (ENS), but its results have not been analyzed for the Chilean population nor in relation to the importance of socioeconomic determinants.[22]
This study analyzed ENS data to estimate the association between SES stratifiers and HRQOL in the population aged ≥25 years residing in Chile, under the hypothesis that HRQOL is worse for SES indicator values that imply greater social vulnerability.
METHODS
A cross-sectional analytical study using data from the 2009–2010 ENS was carried out by the Ministry of Health and the Universidad Católica de Chile. The ENS sample design was a complex one with multistage probability sampling. The sample of 5293 people aged ≥15 years (base population 13,355,826) was representative nationally, regionally, by urban and rural area of residence, by sex and age. Given the interest in analyzing SES indicators that require a certain degree of individual autonomy, this study only considered respondents aged ≥25 years, corresponding to a subsample of 4490 persons (2.3% error). Some 17 people who did not respond to the SF-12 survey were excluded, for a final sample of 4473 (base population 10,419,141, 84.5% of the 2010 ENS sample).
The ENS included morbidity and health questionnaires, anthropometric and physiological measurements, and blood and urine samples. Field research was conducted between October 16, 2009 and September 6, 2010. Data were entered directly into personal digital assistants. Data analysis was done at the Universidad Católica de Chile. The ENS protocol was approved by the Research Ethics Committee of the Universidad Católica de Chile Medical School. Information was gathered following signed informed consent, and assurance of confidentiality of sample collection and delivery of results.[23]
HRQOL was measured with the SF-12 v. 2 survey, which consists of 12 questions grouped in eight health domains: general health, physical functioning, bodily pain, vitality, mental health, social functioning, and role functioning (physical and emotional); and two composite scales, physical and mental HRQOL (all scores weighted and summed; value range 0–100).[20,24] Independent variables assessed were SES stratifiers: educational level (years of education, and grouped as primary or less, secondary, and higher), employment status in the last year (employed, unemployed, and not in the workforce such as homemakers, students, pensioners or those unable to work due to disability) and monthly per capita household income (total household income / number of members aged ≥20 years) in groups corresponding to categories of the 2009 National Socioeconomic Characterization Survey:[25] <100,815 Chilean pesos (<US$140), 100,815 to 286,399 Chilean pesos (US$140 to US$398) and >286,399 Chilean pesos (>US$398). The following covariates were controlled: sex, age, area of residence (urban or rural), type of health insurance (public insurance through the National Health Fund, FONASA; private insurance through health insurance institutions, ISAPRE; other), presence of chronic conditions (high blood pressure, diabetes or excess weight), and symptoms of depression.
Complex sampling techniques were applied for all estimations using the complex samples module of SPSS v. 19. Five steps were carried out: 1) calculation of SF-12 scores using procedures described by the instrument’s developers;[24] 2) analysis of SF-12’s metric properties (Cronbach alpha for internal consistency and principal component factor analysis for content validity); 3) descriptive analysis of SF-12 (measures of central tendency and dispersion), and score categorization based on values in two levels: good HRQOL (values above the median) and poor HRQOL (values below the median); 4) bivariate analysis of the distribution of physical and mental HRQOL (categorized variables) according to predictors of interest and covariate adjustment, using logistic regression to compare adjusted ORs with 95% confidence intervals, using p <0.05 as the significance threshold; and 5) multiple logistic regression models generated for each HRQOL composite scale separately by SES stratifier and controlled for covariates that were statistically significant in bivariate analysis. Adjusted ORs were used as estimates of association between SES stratifiers and poor HRQOL.
RESULTS
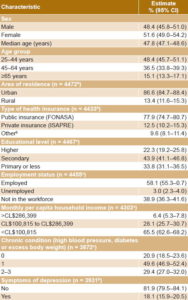
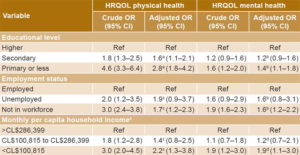
Study population characteristics Women comprised 51.6% of the sample; median age was 47.8 years, and 48.4% were aged 25–44 years. The majority resided in urban areas (86.6%), and 77.9% were covered by FONASA. Average education completed was 10.4 years, and 43.9% had finished secondary school; more than half the population was employed (58.1%); average monthly per capita household income was CL$110,283 (US$153), and 65.5% lived in households with monthly per capita income <CL $100,815 (US$140). With respect to health, 49.6% had one of the chronic conditions included in the survey; 29.4% had two or more conditions; and 18.1% reported symptoms of depression (Table 1).
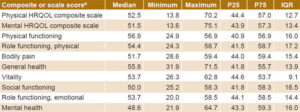
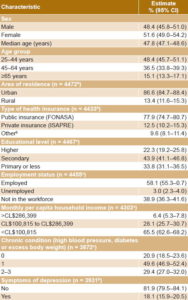
HRQOL and SF-12 psychometric properties Median physical HRQOL was 52.5 (interquartile range 12.7), and median mental HRQOL was 51.5 (interquartile range 13.4) (Table 2). Cronbach alpha was 0.84, and principal component factor analysis confirmed the existence of two components: scales of physical function, physical role, bodily pain and general health associated with physical HRQOL; and scales of vitality, social function, emotional role and mental health linked to mental HRQOL.
Table 1: Sample characteristics, population aged ≥25 years, Chile (ENS 2010, n = 4473a)
a base population 10,419,141 b includes armed forces, no health insurance or other insurance c variation in sample size due to nonresponse to some variables CL: Chilean pesos ENS: National Health Survey FONASA: National Health Fund ISAPRE: health insurance institution
Table 2: SF-12 results, population aged ≥25 years, Chile (ENS 2010, n = 4473a)
a base population 10,419,141 b all scores weighted and summed; value range 0–100; standardized with mean 50, SD 10[24] ENS: National Health Survey HRQOL: health-related quality of life IQR: interquartile range P25: 25th percentile P75: 75th percentile
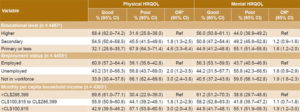
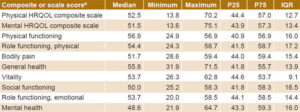
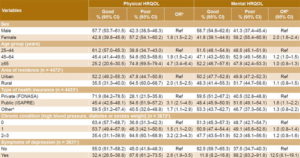
Physical HRQOL The proportion of people with poor physical HRQOL increased as educational level decreased (Table 3). With higher education as the reference category, the ORs for poor physical HRQOL associated with secondary and primary education or less were 1.8 and 4.6, respectively. Poor HRQOL was also more frequent among people who were not in the workforce and in those whose monthly per capita household income was <CL $100,815.
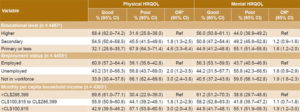
Poor physical HRQOL was more frequent in women, in people aged ≥65 years compared to both younger age groups (25–44 and 45–64 years), in residents of rural areas, in FONASA enrollees (compared to those covered by ISAPREs or other insurance), and in persons with two or more chronic conditions (compared to those with none or one), and in people with symptoms of depression (Table 4).
Table 3: Physical and mental HRQOL by SES, population aged ≥25 years, Chile (ENS 2010, n = 4473a)
a base population 10,419,141 b crude odds ratio c variation in sample size due to nonresponse for some variables ENS: National Health Survey HRQOL: health-related quality of life n: sample size Ref: reference group SES: socioeconomic status
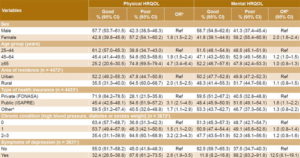
Table 5 displays results of multivariate models generated to analyze SES stratifiers’ effects on physical HRQOL and adjusted ORs for control variables. Risk of poor HRQOL was greater in persons with primary education or less compared to those with higher education, (OR 2.8, 95% CI 1.8–4.2,).
Risk of poor HRQOL was higher for persons not in the workforce than for employed persons (OR 1.7, 95% CI 1.2–2.3). Persons with monthly per capita household income <CL $100,815 also had higher risk of poor HRQOL than those with incomes >CL$286,399 (OR 2.2, 95% CI 1.3–3.8).
Mental HRQOL Differences by SES were also observed in mental HRQOL (Table 3), with a greater probability of poor HRQOL in persons with primary education or less, not in the workforce, and with monthly per capita household income <CL $100,815.
Mental HRQOL exhibited differences by sex (greater probability of poor HRQOL in women), type of health insurance (greater probability of poor HRQOL in FONASA enrollees), and symptoms of depression (greater probability of poor HRQOL in those with symptoms). Differences by age, area of residence and chronic disease were not significant.
When controlled for covariates (Table 5), the effect of the stratifiers on mental HRQOL was more moderate than for physical HRQOL. Persons with primary education or less reported poor HRQOL more frequently than those who completed higher education (OR 1.4, 95% CI 1.1–1.8).
Those not in the workforce had poor HRQOL more frequently than employed persons (OR 1.6, 95% CI 1.2–2.2). Finally, HRQOL was also worse for those in the lowest monthly per capita household income category ( <CL $100,814) than for those in the highest category (OR 1.9, 95% CI 1.1– 3.0).
Table 4: Physical and mental HRQOL by covariates, population aged ≥25 years, Chile (ENS 2010, n = 4473a)
a base population 10,419,141 b crude odds ratio c variation in sample size due to nonresponse for some variables d includes armed forces, no health insurance or other insurance ENS: National Health Survey FONASA: National Health Fund HRQOL: health-related quality of life ISAPRE: health insurance institution n: sample size Ref: reference group
Table 5: Poor physical and mental HRQOL and socioeconomic variables, population aged 25 years, Chile, (ENS 2010)
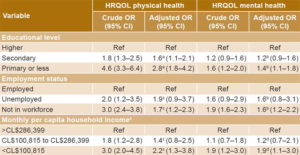
a adjusted for sex, age group, health insurance system, chronic conditions, symptoms of depression b adjusted for sex, age group, chronic conditions, symptoms of depression c adjusted for sex, age group, residence, health insurance system, chronic conditions, symptoms of depression d adjusted for sex, age group, chronic conditions, symptoms of depression ENS: National Health Survey HRQOL: health-related quality of life Ref: reference group
DISCUSSION
Our analysis revealed differences in both physical and mental HRQOL. The most vulnerable groups according to SES stratifiers always perceived the worst HRQOL, unlike groups in intermediate strata. The fact that those with a greater probability of poor HRQOL had primary education or less, were not participating in the workforce, or had a monthly household per capita income <CL $100,815 could be due to a direct effect of their living conditions and access to health services, which are themselves determinants of subjective health. Persons with low SES had more health problems and fewer resources to address them, which, as Delpierre suggests,[17] influences perceived HRQOL.
Several studies in the international literature agree with our assessment of SES’s effects on perceived health.[5,16–19,26] In general, better HRQOL is found in higher-income groups,[5,16–19], just as subjective health assessment is worse among unemployed or retired persons,[16,19] which could be due to a higher proportion of women aged ≥65 years and people with chronic health conditions in that group.
In Chile, studies of perceived health have also identified differences associated with SES and worse perception in the quintiles with the least resources,[27–29] as well as a positive association between perceived health and being employed and socioeconomic status.[21]
Even though international evidence is not absolutely consistent regarding the relationship between HRQOL and sex,[4,5,16] our results are consistent with those of earlier Chilean studies that reported poorer HRQOL in women,[21,27,28,30–32] which may be linked both to their position in the social structure as well as to their living conditions, characterized by the worst indicators for education, income, poverty and employment status.[25,27,28,33]
In terms of physical health, poor HRQOL was more frequent among people aged ≥65 years. There was no significant difference in relation to mental health in this age group. This coincides with previous studies [32,34], so it can be inferred that deteriorating physical conditions and functions associated with increasing chronic disease become more noticeable with advancing age. Perception of mental health may be linked to satisfaction with life, beyond health as such. There is evidence of a U-shaped association with age that describes high subjective well-being in young people, lower in adults, and high again in older adults,[15,33,35] interpreted as owing to a change in older peoples’ expectations that translates as greater satisfaction with their time of life.
Regarding the health insurance system, as with prior analyses,[32] this study showed worse HRQOL in public health enrollees, among whom there is a high proportion of older adults and people with comorbidities compared to private insurance enrollees.[25,27,28,33,36]
The results for chronic conditions coincide with a 2006 study that found illness or disability to be the factor with greatest influence on perceived physical health.[21]
Although differences were observed by SES in both physical and mental HRQOL, they were most marked in the physical dimension. This could be due to a more direct effect of SES on people’s physical health, given worse living and working conditions among the most vulnerable, and to barriers to access to health care and other goods and services that such groups must overcome. The stratifier with greatest influence on physical HRQOL was educational level, which affects health through various mechanisms, as an indicator of the intellectual and material resources of the family of origin,[9,10] and as a determinant of life styles and responsiveness to promotion and prevention messages, as well as of the capacity to interact with health services.[9]
The greater homogeneity in perceived mental HRQOL could be due to other mechanisms that act as intermediaries between stratifiers and HRQOL, such as attitudinal components, social cohesion and social support networks. However, these variables were not included in the 2010 ENS, ruling out analysis of how a person’s feelings, emotions, memories and beliefs might affect perceived HRQOL.[8]
Given the cross-sectional nature of the study, we could not establish temporal precedence between SES stratifiers and HRQOL, so it is possible that associations observed were due to an influence by HRQOL on SES, rather than the converse.
Nevertheless, the study is based on the application of an instrument that is widely used internationally, using secondary data and an appropriate methodology for analyzing complex population samples to estimate the population’s HRQOL and demonstrate its association with SES stratifiers. This information is of interest from a public health perspective, because perceived health can be a marker of health inequities, due to its association with resources, hospitalizations and mortality.[3,17]
For that reason, and given the limited development of HRQOL analysis in Chile, we recommend further study of the subjective perception of health and its association with living conditions. SES indicators should be optimized and attitudinal aspects explored through qualitative methodologies.
CONCLUSIONS
SES is associated with perceived HRQOL, with worst HRQOL reported by the most vulnerable socioeconomically. Women, older adults, residents of rural areas, public health enrollees and people with chronic conditions or symptoms of depression have a greater probability of perceiving poor HRQOL. The effect is more pronounced for physical than for mental HRQOL.