INTRODUCTION
Acute anterior poliomyelitis, formerly known variously as polioviral fever, infantile paralysis and Heine–Medin disease,[1] is a viral disease that primarily strikes children and produces serious sequelae and disability. It takes three forms: subclinical, nonparalytic and paralytic. Approximately 95% of infections are subclinical and flaccid paralysis appears in <1% of cases. The causal agent is poliovirus (genus Enterovirus) types 1, 2 and 3, all of which can produce paralysis.[1,2]
Virus is transmitted through direct person-to-person contact or by water and food contaminated with infected fecal matter.[1,2] Circulation of poliovirus is limited to ever fewer countries (currently Afghanistan, Pakistan, Chad, Niger and Nigeria).[3]
This article describes and analyzes the history of acute anterior poliomyelitis epidemics in Cuba, from the first reports of the disease through official certification of its elimination in 1994; presents morbidity and mortality data from the polio epidemics; describes the 1962 vaccination campaign and its protective impact on children; and characterizes adjustments to improve effectiveness of subsequent campaigns. Successful polio control in Cuba is assessed in the context of national health strategies and the social, political and financial support they received.
METHODS
The historiological method was used to analyze documentation.[4] The 1932–2000 polio morbidity and mortality statistics from the Ministry of Public Health’s (MINSAP, the Spanish acronym) National Statistics Division databases were reviewed and data used to calculate crude morbidity and mortality rates, using mid-period population estimates from the State Statistics Committee (now the National Statistics Bureau).
A critical review of reports and scientific literature on the epidemics, polio vaccination campaigns and their results was conducted. Between 2003 and 2012, the directors of the first polio vaccination campaign and Cuban epidemiology historians were interviewed, as were the following experts who were involved in the work of the first and subsequent campaigns: Dr Helenio Ferrer Gracia, MINSAP director of epidemiology (1961–1979) and an organizer of the national polio vaccination campaigns (interviewed 2008); Dr Conrado del Puerto Quintana, deputy director of health for hygiene and epidemiology in Matanzas province 1961 through 1963 (interviewed 2003); and Dr Gabriel Toledo Curbelo, a veteran of the Rural Medical Service; (interviewed 2003, 2005). Dr Miguel A. Galindo, head of Cuba’s National Immunization Program, was also consulted (interviewed 2011, 2012).
The study’s findings follow, with subheadings referring to polio’s chronology in Cuba, including early case detection and epidemics, as well as elimination efforts and their fundamental components.
POLIO DETECTION, REPORTING AND EPIDEMICS
Dr Francisco Cabrera Saavedra first reported patients with polio sequelae in Cuba in 1898 at the end of the Spanish colonial period in the town of Caibarién. That same year, US physicians observed cases on the Isla de Pinos (Isle of Pines, now the Isle of Youth).[5] In 1906, a small outbreak in the village of Santa Fe (Isla de Pinos) was reported by Dr Alberto Recio, who provided no details.[6] It is assumed that the disease was imported from the USA by expatriates living on the Isla de Pinos—a result of extensive trade and travel between the two countries from the second half of the 19th century forward.[5] Also contributing to spread of the disease were troop movements during two US military interventions in Cuba (1899 and 1906).[7]
In 1909, Dr Recio reported three cases of paralytic polio, two in Havana and one in Calabazar on the city’s outskirts.[6] The first epidemic was reported the same year in the former province of Las Villas (central Cuba), mainly in the city of Santa Clara and some other municipalities. Dr Recio’s report to Dr Juan Guiteras, chief medical officer, recorded a total of 200 cases in Santa Clara with 8% mortality[8] and 140 cases in 10 other municipalities (mortality unknown).[9] The main victims were children aged <4 years.
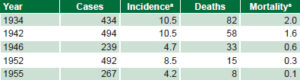
Compulsory polio notification was mandated in 1902, but enforcement was inconsistent in the first half of the century, continuous morbidity and mortality records beginning only in 1932; hence, the dearth of data for epidemics between 1909 and 1934 (Figure 1). In fact, a literature review produced no study on epidemics in any Cuban population during this period other than that of Santa Clara and vicinity in 1909.[5]
Although data from 1932 through 1958 may not have been complete, they revealed five epidemics in this period (Table 1).[5,10] After 1934, epidemics began appearing at regular intervals, usually in the summer (mainly July and August). But the 1946 epidemic struck in May, coinciding with an outbreak in Florida, USA; in Cuba, this epidemic affected mainly children aged <5 years, while in the USA, it affected mainly children aged 5 to 14 years.[5] The percentage of cases in children aged >10 years in Cuban epidemics increased from 3% in 1934 to 14% in 1946.[10]
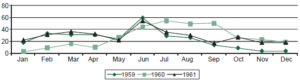
Prior to 1959, Cuba (like many other countries) had no public health policy that provided for polio prophylaxis or control measures.[11] However, transformations beginning that year led to improved compulsory disease notification compliance, and statistical records became more complete and reliable. Reporting confirmed that most cases occurred in June through August, observing an increase in annual case numbers in the early 1960s (Figure 2). From 1957 to 1961, polio reached a higher level of endemicity, with numbers as high as those of epidemic years in the two previous decades. This was interpreted as a result of improvements mentioned in case reporting by medical units across Cuba, an inference supported by the fact that mortality rates did not increase appreciably over the same period (Figure 1).
Figure 1: Polio incidence and mortality in Cuba, 1932–1962

Source: National Statistics Division, MINSAP * Mortality rates per 100,000 population (author’s calculations)
Table 1: Polio epidemics in Cuba 1934–1955
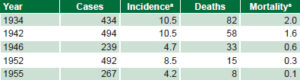
a Rate per 100,000 population / Sources: Health and Welfare Bulletin (1932–1933) Official Health and Social Assistance Bulletin (1934–1953); Statistical Information System for Reportable Diseases; populations 1932–1954, Central Planning Office; populations 1955–1961, State Statistics Committee
The last epidemic outbreak in Cuba occurred in 1961, with 342 cases (Figure 1), 30% of these in children aged >4 years.[9] From 1932 to 1961 a total of 3939 cases of polio had been reported, 3134 of them paralytic; there were 430 deaths, for a case fatality of 10.9%.[10]
1962: DEVELOPING A NATIONAL STRATEGY TO ELIMINATE POLIO
Public health authorities devised a coherent strategy to control the disease, the centerpiece of which was annual vaccination campaigns begun in 1962. Three essential elements characterized the campaigns and followup:
- high vaccination coverage achieved through week-long drives, administering doses before the summer months;
- surveillance of suspected cases; and
- outbreak investigation and control, if necessary.[12]
The strategy also relied on strong support from the central government, training of health personnel and volunteers, and education that developed public support throughout.
Prior to planning the initial 1962 campaign, epidemiological research on polio in Cuba was reviewed and other studies conducted on its evolution and characteristics over the previous 30 years. In the three years prior to the campaign (1959–1961), incidence rates were 4.3, 4.9 and 4.9 per 100,000 population, respectively, suggesting higher levels of endemicity than previously estimated. Over 90% of cases of paralytic polio occurred in children aged <15 years, and the highest age-specific rates were in children aged <4 years.[9]
In 1961, MINSAP’s National Statistics Division received technical assistance from Dr Karel Sacek, Czechoslovakia’s chief of epidemiology and microbiology and a member of the WHO Expert Committee on Virology. Among other aspects, Dr Sacek studied seasonality and vulnerability by age. He found incidence highest between June and August, the disease primarily striking children aged <4 years, although all children aged <15 years were at risk. It was therefore decided to immunize the population aged 1 month to 15 years in the months before summer (Helenio Ferrer, personal communication, 2008). The 1962 campaign thus targeted all Cuban children in this age group using the Sabin trivalent oral polio vaccine, a safe and easy-to-administer vaccine of proven effectiveness.[12]
Figure 2: Polio cases in Cuba by month and year, 1959–1961
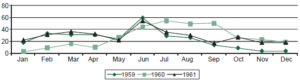
Source: National Statistics Division, MINSAP
Context, conception and organization of the 1962 vaccination campaign To understand the design of Cuba’s first national polio vaccination campaign and those that followed annually, it is useful to highlight a series of facilitating political and administrative changes at the national level from 1959 to 1962, introducing visions and strategies that adopted a disease prevention and community-oriented health approach. The most important of these are summarized in Table 2.
A new public health structure and the existence of mass social organizations were assets in promoting polio vaccination in a campaign format, in keeping with MINSAP’s strategy of mounting major campaigns to control a number of communicable diseases frequent at the time, such as malaria, diphtheria and childhood tuberculosis, the latter two the object of national vaccination campaigns targeting the country’s pediatric population.[11]
Table 2: Events facilitating Cuba’s national polio vaccination campaign, 1959–1962

Source: Del Puerto[10]
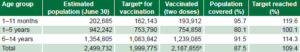
The 1962 polio vaccination campaign set a coverage target of vaccinating 80% of Cuban children aged 1 month through 14 years, 11 months and 29 days—1,999,785 in all.[9] The campaign was divided into five phases: campaign planning, (eight weeks from late December 1961 through February 25, 1962); first dose administration (one week from February 26 through March 4); interval between doses (4 weeks); second dose administration (one week from April 25 through May 1); and evaluation (the four weeks of May).[12]
The campaign was managed and overseen by MINSAP, with national and local collaboration from Cuba’s mass social organizations: the Committees for the Defense of the Revolution (CDR, the Spanish acronym), the Federation of Cuban Women, the Association of Rebel Youth, and the National Association of Small Farmers (ANAP, the Spanish acronym). In tandem with the Cuban Red Cross, their role was to raise public awareness and involve the population in campaign activities, address reluctance by families to vaccinate their children (especially in rural areas), and assist families in getting their children to vaccination posts with the required vaccination cards: in short, employing their volunteers to ensure effectiveness of the campaign nationwide.[12]
The Ministry of Education made schools available for use as vaccination posts, along with teachers, who served on vaccination teams. The Ministry of the Revolutionary Armed Forces provided helicopters for transporting vaccines and personnel to mountainous and hard-to-reach areas. The National Institute for Agrarian Reform provided refrigerated vehicles.
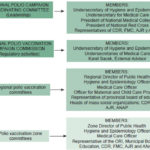
Thus, this effort exemplified intersectoral action in a health intervention.[12] Figure 3 shows the organizational chart of the first polio vaccination campaign.
The National Polio Vaccination Commission assumed administrative, technical, and regulatory functions; [13,14] its members included the Undersecretary of Hygiene and Epidemiology (chair), the Undersecretary of MINSAP and the Executive Director-General of the Ministry, as well as other experts.
Each regional office (seven in all, one for each of the then six provinces and two for the former province of Oriente) had a committee of several officials, whose task was to coordinate and monitor implementation and oversee vaccine storage and distribution (Figure 3).[12]
Regional management, in turn, was divided into zones (essentially corresponding to municipalities in each province) (Figure 3), in which committees of municipal officials were responsible for coordinating and implementing local vaccination activities.[12] In rural areas, the Rural Medical Service, rural militias and ANAP had special responsibility for the campaign.
Figure 3: Organization of Cuba’s National Polio Vaccination Campaign, 1962
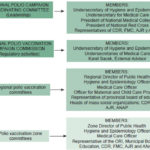
ORI: Integrated Revolutionary Organizations; CDR: Committees for the Defense of the Revolution; FMC: Federation of Cuban Women; AJR: Young Rebels’ Association; ANAP: National Association of Small Farmers.
Zone committees coordinated the human resources for campaign fieldwork, consisting of stationary and mobile teams in each zone, deployed in numbers as conditions warranted.
Stationary teams worked at vaccination posts (located in selected facilities, mainly health centers and schools). Each included a physician in charge; a vaccination officer and two assistants responsible for vaccine transportation and administration; a records manager, in charge of reviewing and filing vaccination cards, compiling lists of people vaccinated, filling out daily information reports to the zone office, and distributing proof of vaccination and vaccination cards; and five to ten people responsible for maintaining order and ensuring that the whole vaccine lozenge was swallowed.
Mobile teams traveled to more distant locations to vaccinate and gather data, using jeeps and minivans or, in very remote areas, horses and mules. Teams consisted of five people: an equipment officer, a vaccination officer, a data manager and two persons responsible for maintaining order and ensuring the whole lozenge was swallowed.[12]
Table 3: Oral polio vaccination outcomes and coverage by age group (Cuba, 1962)
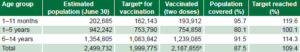
a 80% b 32,052 vaccinated children of unknown age not included
Source: National Statistics Division, MINSAP
Individual vaccination cards were printed for recording the child’s name, address, date of vaccination and doses administered, along with the signature of the vaccination officer.[12]
In both urban and rural areas, CDR health officers and ANAP members used the cards to register all children aged 1 month through 14 years. The cards were issued to the children’s families, who then presented them at vaccination posts, where they were filed alphabetically at the end of the first stage for use at time of the second dose.[12,14] Proof of vaccination was provided for families to show health workers and volunteers during their field visits, while the vaccination cards were kept at vaccination posts, serving as the official cumulative vaccination record.[12]
The pediatric population was vaccinated as programmed (Table 3), with 2.5 mL of suspension administered to children under 2 by teaspoon and a vaccine lozenge to children aged 2 through 14 years.[12]
Vaccination activities were evaluated daily as the campaign unfolded. Daily reports from vaccination posts indicated distribution by age group and quantities of liquid doses and lozenges used; these were summarized at the zone level and transmitted by telephone to regional offices, which forwarded the information to MINSAP’s National Statistics Division, also daily.[12]
Vaccine and logistical considerations The campaign used the Sabin trivalent oral vaccine (serogroups 1, 2 and 3), made with live attenuated virus containing 1 million TCID50 (median tissue culture infective doses), composed of 500,000, 200,000 and 300,000 for serogroups 1, 2 and 3 respectively, in lozenge form and manufactured in the Soviet Union, where 330,000 doses of liquid vaccine were also prepared for children aged <2 years.[13,14] A total of 5 million doses were administered.[13,14] Procurement of enough doses for immunizing the target population was coordinated with the Soviet Union’s Ministry of Public Health, which sent the vaccines in two shipments, one for each programmed stage of the campaign. Vaccines were transported and stored at –20ºC.[12,14]
The vaccine was distributed from a central warehouse in refrigerated vehicles to the seven regional offices, where it was kept at –20ºC. From there, it was transported to the zone offices in refrigerated vehicles at 4–8ºC. The doses were then distributed to the vaccination posts in portable coolers protected from humidity by plastic covers.[14]
The 1962 vaccination campaign: training and public education At national and regional levels, Professor Karel Sacek lectured health professionals and zone directors on polio and the live virus oral vaccine. Health professionals from the national level trained auxiliary personnel, consisting of vaccinators, health brigade members, and health officers from regional and zone social organizations. Three thousand instructors were trained in five-day short courses on vaccination with oral polio vaccine and in turn, taught 50,000 health officers, all volunteers.[12]
Meanwhile, an intensive publicity and public health education campaign was launched, broadcasting 30,000 radio and television messages before vaccination began. Before and during the campaign, publicity activities included a daily 30-minute radio program mainly for the rural population; daily 12-minute television spots featuring talks, dramatizations, and instructions about polio vaccination; and four television roundtables (two for technical personnel and two for the general public).[12]
Mobile units from MINSAP’s Department of Health Education informed the public in the various zones and distributed posters nationwide, with messages targeting the general population, mothers, rural dwellers and children. The print media also carried extensive coverage through newspapers, magazines, newsletters and billboards in cities and towns. Once vaccination began, progress updates were published daily throughout the country.[12]
Evaluation and results Vaccination card data were tabulated mechanically, calculating distribution by age group, number of doses administered, and percentage of target coverage met (Table 3).[12]
Qualitative evaluation of results included determining immune status achieved in the pediatric population. Before and after each stage of the campaign, serum neutralizing antibody titers were examined using the microagglutination test, the standard procedure for determining immunity to poliovirus.[14] Prior to vaccination, 476 serum samples were collected from throughout Cuba, and another 433 collected four weeks after stage one (first dose). This serologic monitoring was repeated six months after stage two (second dose) had concluded. The findings showed low levels of protection against the three vaccine serotypes prior to vaccination and revealed over 80% immunity for type 1 and 2 viruses and 76.7% for type 3 in urban and rural children aged >1 year upon completion of the two-stage vaccination process.[13–15]
Vaccination campaign impact was dramatic. Only 46 cases were reported in the first semester of 1962; and four months into the campaign, no new cases appeared.[9] According to data from the National Statistics Division, after that initial campaign, only ten isolated cases of polio were reported through 1994, and no deaths from the disease were reported after May 1962.[11]
Related results were impressive. The campaign:
- met its objective, vaccinating 87.5% of the population aged 1 month through 14 years (109.4% of target coverage) with 5 million doses administered (Table 3);
- demonstrated the effectiveness of a multidisciplinary, intersectoral effort based on coordinated action by government and mass social organizations, with health authorities taking the lead and actively informing and involving the population through training of volunteers and public education. Thus, broad public participation was garnered to meet a national health goal—a first for Cuba;[11]
- yielded satisfactory results in all age groups. The lowest coverage was obtained in the group aged 1 to 5 years, although the target was still met (Table 3);
- decreased polio incidence to below prior ranges;
- demonstrated the effectiveness of two doses of trivalent vaccine with 1 million TCID50 in protecting Cuban children against polio;
- reported no vaccine-attributable adverse reactions during the campaign; and
- contributed to reduction of polio deaths to zero since 1962.
SUBSEQUENT VACCINATION CAMPAIGNS AND RELATED MEASURES TO ELIMINATE POLIO IN CUBA
The results of the first campaign and its annual repetition thereafter were described in Cuba’s application for certification of polio elimination submitted by the Ministry of Public Health to WHO/PAHO, which on November 7, 1994, officially declared polio eliminated from Cuba.[16,17]
Between the first vaccination campaign in 1962 and 1994 (the period under study), Cuba conducted 34 annual national polio vaccination campaigns, during which 62,544,458 doses of vaccine were administered reaching 90% coverage in the Cuban population aged <49 years.[9,18] Targeting children aged 1 month through 14 years, the campaigns continued to be conducted in February and March during national vaccination weeks, doses administered in different regions over a 72-hour period.[17]
Recommended ages for vaccination have fallen gradually, based on serologic immunity study results.[13–16,18,19] From 1970 to 1992 the schedule consisted of two doses of trivalent vaccine at a six-week interval for children up to three years of age and a booster for children aged nine years.[16] Today, children receive the first two doses at any age from 30 days to 2 years, 11 months and 29 days, and a booster dose up to 9 years, 11 months and 29 days. Since 1992 the vaccine has been administered in drops instead of lozenges.[17]
Different types of oral vaccine have been used over time, the most common being Trivalent 1,2,3 (1962, 1964–1967 and 1969–1994). In 1963, Bivalent 1,2 was used for the first dose and Monovalent 1 for the second. In 1968, Monovalent 1 was used for the first dose and Bivalent 2,3 for the second. These decisions were always supported by epidemiological surveillance of circulating virus, based on virologic studies by Dr Pedro Más Lago.[13,17,20] In the third campaign, in 1964, to guarantee optimal immunity in the ages at highest risk, a vaccine containing 1 million TCID50 for each of the three serotypes of vaccine virus was used.[13] From 1970 to 1991 a vaccine was used that contained 500,000, 200,000 and 300,000 TCID50 for types 1, 2 and 3, respectively.[15,16]
Over the years, the campaigns have received international support from organizations such as PAHO, WHO, UNICEF and Rotary International, which have provided technical assistance through experts who advise and train campaign workers, equipment ranging from vehicles to thermoses for refrigerated vaccine transport, and the vaccines themselves.[16]
Technical aspects of the vaccination campaign have been strengthened, drawing on the experiences of the mass social organizations involved, enlisting active participation by the primary health care system, most recently structured around the family physician and nurse,[16] and altering vaccine composition and formulation as needed. Through continuous education, public awareness about polio prevention has increased, contributing to keeping the country polio free.[16]
On the scientific front, an important development associated with the introduction of polio vaccination was the launch of virologic studies in Cuba at a new research laboratory headed by Dr Pedro Más Lago.[9] The laboratory was established to conduct surveillance and advise the vaccination program, maintaining annual serologic surveillance of immunity in the pediatric population, recommending the type of vaccine to use and age groups to vaccinate. Over 20 serologic studies were conducted to determine immunity to the three types of poliovirus, two of these studies with financial assistance from PAHO.[9,14,16] Initially housed at the National Institute of Hygiene, Epidemiology and Microbiology, in 1989 the laboratory was transferred to the Pedro Kourí Institute of Tropical Medicine, where it remains today.
When the national polio vaccination program was launched in 1962, the National Commission for the Study of Infectious Neurologic Syndromes was also created. Charged with investigating all suspected cases of polio, the commission was made up of neurologists, virologists, pediatricians and epidemiologists. From 1963 to 1989 it investigated 93 suspected cases, confirming 10 cases of polio, all in unvaccinated children. In 15 cases, nonpolio enteroviruses were isolated; the remaining 68 were diagnosed as Guillain-Barré syndrome, transverse myelitis and other polyneuropathies.[9,16]
Acute flaccid paralysis is reported as an adverse event of vaccination with oral polio vaccine (OPV) in Cuba.[18] Galindo noted 20 reports of flaccid paralysis associated with vaccination (the last in 2006)[21] identified through the surveillance system, considering it a rare complication. The risk in the total population aged <15 years vaccinated in Cuba from 1962 to 2006 was 1 case per 3,778,811 doses administered.[18,21]
The main measures used to control outbreaks between 1963 and 1989 were epidemiologic histories, stool samples for virologic studies, serologic studies (matched sera) and virologic studies conducted by the National Commission on Infectious Neurologic Syndromes of material from autopsies of children with suspected poliomyelitis.[16]
The end of wild poliovirus circulation had been suspected since 1967; and was confirmed by at least seven investigations between 1970 and 1994.[14–16] The studies looked for regression of vaccine virus attenuation with viral multiplication in the intestine and transplacental passage of vaccine-stimulated antibodies, and assessed seroconversion at different dosages, as well as duration of immunity.
In 1994, PAHO issued its Certification of Eradication of the disease: “The conclusion of the National Commission for Certification of the Eradication of the Poliomyelitis in Cuba that the wild polivirus is eradicated in the country is confirmed. Washington DC, 7 November 1994. Dr Carlyle Guerra de Macedo, Director.” [translated from the Spanish—Eds.][22]
Commenting on the report submitted by Cuba on June 8, 1994 to obtain this certification,[16] Dr Ciro de Quadros, chief of the PAHO Program on Immunization, called the country’s vaccination campaign strategy a model for the rest of the world.[22] Referring to the first campaign, Dr Mirta Roses, assistant director of PAHO at the time said, “Its concept, its ideology, its instruments, its methodology shook the world. …Cuba transformed the probable into the possible.” [translated from the Spanish—Eds.][23]
Más Lago calculated that,[9] had polio followed its natural course uninterrupted by vaccination, it would have caused 1200 cases of paralysis and 200 deaths between 1962 and 1970.
Polio was eliminated in Cuba thanks to an ongoing combination of several factors: maintenance of high immunization coverage, a highly sensitive epidemiological surveillance system that included exhaustive study by the National Commission on Infectious Neurological Syndromes of every suspected polio case; sustained political commitment; a high degree of social participation; and constant and effective use of the media.[9,12,16,17] The successes achieved from the beginning were confirmed by Dr Sabin, who visited Cuba in 1967. In particular, it was demonstrated that a strategy such as Cuba’s, involving systematic vaccination campaigns and unique in the world at the time, could eliminate polio with an oral vaccine of live attenuated virus.[14]
CONCLUSIONS
The 1962 polio vaccination campaign was one of the first successes in Cuban preventive medicine and epidemiology after the post-1959 reform of the health system. The Cuban experience demonstrates that the disease can be controlled with an effective vaccine and appropriate epidemiological measures, coupled with adequate social, financial and political support. A single coordinated nationwide campaign implemented only twice a year, to prevent constant release of vaccine virus into the environment;[14] and the intersectoral effort that made it possible to implement the campaign at these two times are among the main reasons for its success. Such strategies and results may provide useful examples for other countries in their efforts to eliminate polio.
ACKNOWLEDGMENTS
Thanks to Dr Miguel Galindo, head of MINSAP’s National Immunization Program, for providing a wealth of data for this article; to Dr Helenio Ferrer, the late Drs Gabriel Toledo Curbelo and Conrado del Puerto Quintana; and to MINSAP’s National Statistics Division staff for their help in this investigation.