INTRODUCTION
Tuberculosis (TB) is a bacterial infectious disease caused by Mycobacterium tuberculosis. It is a global health problem, despite being preventable and curable. According to the WHO, an estimated 9 million people had TB in 2013 and 1.5 million died from it, with 95% of cases and 98% of deaths occurring in low-income countries.[1,2]
TB mortality rates fell by 45% worldwide between 1990 and 2013 (with the exception of many African countries).[2] Countries that reduced mortality are on their way to achieving the global Stop TB Partnership’s target to halve rates of prevalence and mortality by 2015, compared to 1990 levels.[3]
TB was a major health problem in Cuba in the nineteenth century and first six decades of the twentieth, with a reported incidence of 35.9/100,000 in 1954 and 40.1/100,000 in 1962.[4] However, By 2012, TB incidence had been reduced to 6.1/100,000,[5] one of the lowest in the Americas.
According to PAHO, countries with rates below 25/100,000 are well situated to control TB.[6] The current goal for the Americas, adopted at the 2006 Costa Rica Meeting, is one case per million. Chile, Costa Rica, Puerto Rico and Uruguay have adopted similar paths within the framework of the objectives, strategies and actions promoted by PAHO since 1999 for Latin American countries with low TB prevalence.[6,7]
To reach the goal of eliminating TB as a public health problem in Cuba when the all-form TB rate falls below 5/100,000 population—[8] the epidemiological evolution of the disease and strategies designed to prevent and manage it to date must be well understood. This should inform decisionmakers’ next steps.
This paper aims to present a historical survey of the components and actions introduced as changes in the 1970 version of the National Tuberculosis Control Program (PNCT) and their impact on TB rates and mortality in Cuba. As background to assess the impact of these changes, Cuba’s TB control history was reviewed from the late 19th century to the organization of the National Tuberculosis Commission and the creation of the first national TB control program in 1963.
METHODS
This research was carried out using the historiological method of document analysis,[9] relying on heuristics to make a deductive-inductive assessment of all available sources on the history of Cuban public health and specifically of TB, and hermeneutics to arrive at general considerations through synthesis. Contemporary reports and scientific literature related to the PNCT in the 1960s and 1970s were reviewed.
Interviews were carried out with key informants who participated in the first stages of TB control. These included Dalia Fernández Vila (senior PNCT nurse); Dr. Helenio Ferrer Gracia, who led the National Department of Epidemiology of the Ministry of Public Health (MINSAP) during the 1960s; and Professor Edilberto González Ochoa, epidemiologist in the PNCT 1967–1974. Morbidity and mortality rates in the TB epidemiology section of the Pedro Kourí Tropical Medicine Institute and MINSAP annual health statistics were reviewed. Relative change (percent) was calculated between 1969 and 2012 for incidence rates.
RESULTS
Tuberculosis in Cuba before 1959 The fight against TB in Cuba began with the 1890 creation of the Anti-Tuberculosis League in Santiago de Cuba. The organization of public services against TB coincided with the first US military intervention in 1899 and founding in 1902 of the national Anti-Tuberculosis League, which, although national in scope, was often hampered by funding constraints or lack of an effective strategy.[10,11]
The Anti-Tuberculosis League was a private society. Negotiations with the Ministry of the Interior in 1903 secured four wards for the League in Havana’s Hospital No. 1 (now General Calixto García) dedicated to TB patients. At that time, dispensaries were created to treat the sick: the first was the Furbush (1906) in Habana Vieja (Havana); the Esperanza Sanatorium (also in Havana) opened in 1908, with 60 beds.[10]
The TB section of the Ministry of Health and Welfare was created in 1926, the National Board against Tuberculosis the following year, and one year later the Hartmann Dispensary opened in Santiago de Cuba. The National Tuberculosis Council was created in 1936. By 1936, the Esperanza Sanatorium had 450 beds, having annexed 362 from the Lebredo Hospital. In 1937, dispensaries for outpatient TB treatment were set up in the cities of Santa Clara, Matanzas, and Pinar del Río. In 1945, the Respiratory Airways Institute was established in the General Calixto García Hospital in Havana.[10,11]
There were also the Grancher and Martí preventoria (infectious disease hospitals) in San Miguel del Padrón and Cojímar (now in Havana Province) with 180 and 200 beds, respectively. The Grancher preventorium treated infants and children aged < 6 years, and the Martí treated children aged 6–12 years. Both institutions hospitalized children of families with TB, for a preventive regimen supervised by doctors and educators. In 1944, there were 10 dispensaries: 5 in Havana and 1 each in the cities of Pinar del Río, Matanzas, Santa Clara, Camagüey, and Santiago de Cuba.[10]
Before 1959, the fight against TB focused primarily on medical treatment, hygiene and diet provided in sanatoriums and dispensaries throughout the country, using a clinical rather than epidemiological approach. Diagnosis and followup were based on radiology, and bacteriology services were limited. BCG vaccine existed but was seldom used.[11]
During the first half of the 20th century, the disease continued to occur mostly among the economically disadvantaged classes, living in slums under conditions of overcrowding, poor hygiene and malnutrition. Assistance by institutions dedicated to fighting TB was inadequate, limited to attempts to make some improvements in the lives of these patients and their families,[10]
PNCT (1963) The shift towards health promotion and disease prevention introduced by the government in 1959 led to establishment of a national Tuberculosis Department, which launched a series of TB control measures, chief among them, the design and implementation of the PNCT, Cuba’s first National TB Control Program,[12,13] which provided TB diagnosis, treatment and prevention measures covering the entire Cuban population.
Development of the PNCT began in 1961, when MINSAP was established to coordinate and lead formation of a single, universal, public health system.[14] That year, MINSAP organized the First National Meeting of TB Hospital and Dispensary Directors. This was the first activity to promote coordination of efforts to effectively manage TB patients and the disease across the country. In the First National Hygiene and Epidemiology Forum, held in 1962, a compulsory reporting system was put in place for communicable diseases, including TB, laying the groundwork for the control program, which was approved the same year. MINSAP’s National Tuberculosis Commission organized a network of dispensaries, doctors’ offices and TB hospitals; extended BCG vaccination coverage; implemented X-ray screening for TB; and provided training to medical and technical personnel.[11,15]
The PNCT’s major objectives were to:
- prevent infection in uninfected people,
- prevent sequelae in people already infected,
- detect unknown cases (early and timely diagnosis), and
- treat and care for the sick.
Its policy/action guidelines included:
- protect healthy people, not just treat the sick,
- prevent transmission of the infectious agent (vaccination, chemoprophylaxis),
- carry out population-wide control measures, and
- use simple and effective methods and techniques.[15,16]
Based on these objectives and guidelines, the PNCT was implemented in 1963 under the direction and supervision of MINSAP’s National TB Commission, and supported by a nationwide network of 27 TB dispensaries, 8 sanatoriums and 24 smear microscopy laboratories. MINSAP’s resources also included 302 polyclinics, 46 rural hospitals and 96 rural health posts, where PNCT activities were also performed.[11]
The program’s criteria for diagnosis and followup were essentially radiological. Without microbiological diagnosis, duration of specific treatments was often prolonged unnecessarily. Prevention included BCG vaccination for newborns in hospitals and chemoprophylaxis of contacts and hyperreactive children (tuberculin reactions ≥15 mm).[11]
A plan to develop TB microbiology and bacteriology laboratories was launched in 1965 by the Cuban network of general polyclinics, requiring personnel training. In 1966, polyclinics began to be actively involved in monitoring patients and their contacts, performing tuberculin screening and BCG vaccination in schools, and integrating these activities into their work plans. The PNCT was further strengthened in 1968 by TB prevention strategies and ratification of data registration criteria, followed by more general use of bacteriology for better patient followup and management. These changes improved understanding of the magnitude of the TB problem, fostering training in a new specialty to comprehensively address TB: pulmonology.[13]
In the early years of the PNCT, patients were managed through notification and registration of new cases and their treatment with TB drugs distributed free of charge.[15] In this first stage of TB control, between 1959 and 1969, the widespread availability of drugs at all levels of the health system, an improved understanding of their effectiveness, and rational use of second-line regimens associated with surgery made important contributions, as were structural improvements in the organization of public health. All of these helped decrease the prevalence of active disease, mortality, and the need for dedicated TB hospital beds.[12]
Also influential were the social transformations carried out throughout the 1960s, making important improvements in the economic, social, and material conditions of the Cuban population. A national campaign virtually eliminated illiteracy, new jobs were created, workplace health and safety conditions were improved, population-wide health education campaigns carried out, childcare centers built, and nutrition improved for children and the general population.[17] In this context, social assistance programs for TB patients were launched, such as ensuring full access to free treatment, including hospitalization, which relieved families of the burden of patient care. In 1970, new legislation was passed, guaranteeing full salary support to TB patients throughout the duration of their treatment.[15]
In late 1969, despite reductions in morbidity and mortality, PNCT managers examined the need for other technical and administrative changes in keeping with scientific advances in TB prevention, control and treatment. Moreover, the lengthy duration of TB treatment resulted in more nonadherence by patients and lack of followup by physicians.[12]
PNCT modifications (1970) After nearly seven years of operation, a thorough study was conducted of the latest global developments in TB prevention and control, as was a comprehensive evaluation of the PNCT. As a result, changes to the program were made, which, in this author’s opinion, were instrumental in the subsequent success of TB control in Cuba. These changes, approved in 1970, were primarily based on research, a strong epidemiological foundation, the use of bacteriology for diagnosis and case monitoring, and directly observed outpatient treatment fully integrated into health services.[11]
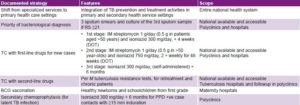
Table 1: Cuba’s National TB Control Program, 1970: main strategies, features and scope
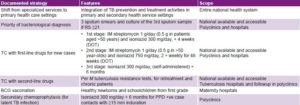
DOT: directly observed treatment IM: intramuscular RS ≥21: respiratory symptoms 21 days or longer TC: tuberculosis chemotherapy
The PNCT modifications described below were not immediately implemented throughout Cuba; first, pilot tests were carried out in two areas, called verification zones, to demonstrate if and how they worked in practice. The areas chosen were 10 de Octubre (corresponding to the current municipality of the same name plus parts of the current Arroyo Naranjo and San Miguel del Padrón municipalities) in Havana, and the northern part of the former province of Oriente (now Holguín Province). The study lasted one year, starting on May 1, 1970, in Havana and on June 1, 1970, in Oriente. Assessment of results at the end of the pilot test was positive, and the model was adopted for extension throughout Cuba.[18]
PNCT tasks to be performed were extended to primary health care settings, focusing on screening general-practice patients for respiratory symptoms (RS) lasting ≥21 days; diagnosis by direct sputum examination and culture; outpatient treatment; and contact tracing. The features introduced into the program were novel: fundamental elements included full population coverage, three direct sputum examinations and culture of the third sample for all patients with RS ≥21 days, and outpatient directly observed treatment (DOT) in three phases (Table 1).[11,19,20]
International studies provided Cuban experts with important knowledge to be considered in designing these changes, including the high percentage of sputum conversion (change from positive to negative) achieved with DOT and the small proportion reported of patients lost to followup; better results obtained by microbiology, which could be performed in primary care settings in Cuba by that time; and the importance of installing X-ray equipment in Cuba’s primary care health units.[11]
Globally, it had been shown that about 2.3% of infected persons developed forms of primary infection with residual calcified lesions; upon disease reactivation (usually in those aged ≥15 years), an inflammatory reaction could cause caseous and cavitated lesions. As a result, purulent material could be expelled from the bronchi, causing respiratory symptoms such as cough and expectoration. In Cuba, other clinical forms with chest pain, dyspnea and hemoptysis were much less frequent in new presentations, and granulomatous forms with hematogenous spread were rare.[19]
The adult respiratory tract had been identified as the most important source of TB contagion.[19] Thus, a symptomatic population enables identification of risk groups to optimize use of basic resources, such as direct smear.
It was decided to identify infectious patients with RS ≥21 days and perform bacteriological sputum exam to search for acid-fast bacilli, a test with a reported sensitivity of 60%–80% but 99% diagnostic specificity.[21] Thus, sputum examination was indicated for the 0.6% of patients seen at community polyclinics who showed lengthy RS. This measure was basic to setting up effective control programs, since 70% of smear-positive cases were symptomatic. Epidemiological control of extrapulmonary TB did not constitute a problem, since these patients are usually asymptomatic and few expel bacilli.[19]
Direct sputum examination is better than X-ray at predicting lung lesion progression and treatment success. And from an epidemiological point of view, a bacteriological exam shows which patients are infectious and therefore a higher threat to the community, enabling transmission interruption. Rational use of bacteriology also permits affordable countrywide screening.[19] However, while radiography only shows lung shadows, with 70% specificity, it does provide information on the type of initial lung injury and helps detect and define major complications, such as pneumothorax and pleural effusion.
It was posited that elimination of sources of infection could be achieved with DOT using optimally effective drugs such as streptomycin and isoniazid. Chemotherapy objectives were defined in the 1970 PNCT reforms as: (1) early patient conversion to smear negative, to interrupt transmission and (2) long-term final healing. The new guidelines indicated that resistant cases or relapses would be subject to a program with the following schedules: three-drug regimen (ethionamide 1 g/day, cycloserine 500–750 mg/day, and pyrazinamide 1.5 to 2 g/day), one of which could be replaced by one or two first-line drugs.[19]
After the 1970 reforms were in place across Cuba, most patients began treatment as outpatients. New cases, which until 1969 were admitted to specialized hospitals and given triple first-line therapy until becoming culture negative, instead received DOT in primary care settings.[11] At each scheduled visit to the polyclinic (daily or weekly), patients were given oral doses of medication (supervised by a nurse) and streptomycin injections. Very sick patients, especially at treatment initiation, were admitted to hospital for a short time and then discharged for outpatient treatment.[12]
Before starting treatment, each patient had a tuberculin test (Mantoux PPD-RT23 2 UT) or was given a chest X-ray if diagnosis was bacteriological. After starting treatment, monthly followup included clinical examination to assess drug side effects and direct sputum microscopy. If microscopy was positive in the fourth month, the sample was sent for culture and sensitivity testing, and chemotherapy continued unchanged until the sixth month. If the sputum was still positive and sensitivity testing showed any kind of drug resistance, the patient was hospitalized and treated with second-line drugs.[20]
The changes in the new program (1970) meant that patient treatment and followup became the responsibility of the 3500 general practitioners working in polyclinics, supported by 134 pulmonologists. The 2834 beds available before 1970 for patients with pulmonary TB (0.3/1000 population, or 7.1% of Cuba’s 40,101 hospital beds) were reduced to 500 countrywide once the new PNCT was consolidated.[11]
An assessment conducted after eight years of the new program, showed the following results:
- The prevalence of patients with RS ≥21 days countrywide was between 0.6% and 0.7% in primary care settings.
- The TB detection rate in symptomatic individuals tended to decrease in direct proportion to the decline in TB incidence.
- Cooperation of patients with RS in providing a first sputum sample decreased substantially after 1976, and this behavior was not modified over the eight years.
- Polyclinics detected 47% of cases in this period based on RS. General hospitals increased diagnosis while diagnosis in TB hospitals decreased (only complicated cases were admitted to specialized hospitals).
- Bacteriological diagnosis by sputum microscopy detected about 75% of cases, with culture contributing the remaining 25%.
- The number and proportion of outpatient TB cases increased with years of program operation, consistent with the move of control activities to primary health care.[21]
The 1970 PNCT changes are considered by this author to be at the core of comprehensive action that radically changed the philosophy of the fight against TB in Cuba, shifting the focus from secondary to primary care. That is, the verticalized, specialty focus of the program, relying on TB experts and pulmonology services, was transferred to primary health care settings at the grassroots level, implemented across the country by community-based polyclinic teams. A cornerstone of these radical changes was to directly relate diagnostic activities, patient outcomes and contact prevention to microbiology results. This provided scientific confidence in diagnosis and led to better followup of patients during treatment, with monitoring by direct sputum examination. It was also an important element in ensuring interruption of disease transmission and provided critical information for epidemiological analysis.[15,20,22]
Greater reliance on microbiology was possible because of developments in the specialty and building of laboratories, already begun in the 1960s. Provincial hygiene and epidemiology laboratories were established to provide resistance testing and preliminary characterization of strains, culture media preparation for smaller regional laboratories, and services to dispensaries and small hospitals in their area. Regional laboratories in turn provided services to community polyclinics, mainly microscopy and strain isolation.[22]
The hub of this network was the National Hygiene, Epidemiology and Microbiology Institute (INHEM), whose TB department was charged with supervision, research and teaching, and served as a national reference center. Bacteriology techniques were standardized in 1965, then published and distributed to all existing laboratories. By 1969 the Hygiene, Epidemiology and Microbiology Laboratory Network comprised 79 general microbiology laboratories—28 of them with TB departments—[22] compared to the 6 that existed in Cuba in 1958 (4 in Havana and 2 in eastern Camagüey Province). There was a steady increase in culture assays in Cuba after these laboratories became operational,[22] and several training courses were set up for technicians and other professionals. Another critically important element was the introduction of treatment variations, including first- and second-line drugs.
The implementation of these new PNCT actions highlighted the need for professional development and continuing education programs, which led to formulation of courses for all primary care personnel, including managers, physicians, nurses, community health workers, and laboratory technicians in polyclinics and hygiene and epidemiology laboratories, that is, staff managing and interacting with TB patients, their families and contacts.[20]
An assessment of main program outcomes since its beginning reflects a net decline in incidence rates, largely due to more specific diagnostic activities based on microbiology. However, mandatory reporting, introduced in 1962, plus pressure by the Tuberculosis Department’s senior management on doctors to report all new and existing cases, reduced under-reporting, reflected in higher rates documented for 1963 and 1964. Also, many new cases were diagnosed in the course of a national TB survey applied by the Department to a large section of the Cuban population.[12]
Later, incidence rates dropped from 65/100,000 in 1965 to 31.2 in 1970. With the updated program, incidence fell further, to 17.8/100,000 in 1971 and 11.6/100,000 in 1979, eight years into the revised PNCT.[23] The downward trend continued, generally attributable to PNCT implementation, including DOT introduced in 1971, and directly observed treatment short-course (DOTS) strategy in place since 1982.[24] The changes made in 1970 related to case definition included the requirement of bacteriological confirmation of diagnosis, thereby reducing the number of new cases reported, and then in 1994–1995 sputum-negative individuals who met clinical and radiological criteria were included as patients.
The continuing decline in incidence was interrupted in the early 1990s, when Cuba faced an economic crisis that affected all spheres of life, including public health.[25] As a result, TB incidence more than tripled between 1991 and 1994, reaching 14.7/100,000 in 1994.[26] Because of this increase, cases began to be reported by clinical-radiological criteria, starting in 1994; it was decided to err on the side of sensitivity to ensure that no case was missed; this could have resulted in some overestimation of incidence in the following years.
Socioeconomic determinants contributing to this TB increase included housing (overcrowding) and food scarcity. The adverse economic conditions also exacerbated susceptibility of malnourished or alcoholic individuals.[27] Malnutrition had been eliminated as a social phenomenon since the 1960s, with a sustained increase through 1989 of caloric supply as part of balanced food intake. But from 1991, food supplies were drastically limited, and daily caloric intake decreased from 3130 in 1990 to 1863 in 1993, equivalent to 78% of mean requirements.[26]
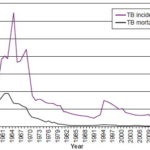
As the economy recovered, new adjustments were made to the PNCT and it regained high priority. TB once again began a steady decline, incidence falling below 10/100,000 in 2001 and reaching 6.1 in 2012 (Figure 1). Thus, despite setbacks during the economic crisis, between 1969 (the year before the PNCT revisions) and 2012, TB incidence fell from 43.1 to 6.1/100,000 population, a net decrease of 85%. This supports effectiveness of measures taken from 1970 forward.
Figure 1: Pulmonary TB incidence and mortality in Cuba, 1954–2012
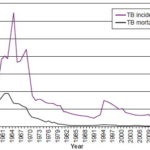
Source: National Statistics Division, Ministry of Public Health (CU)chemotherapy
The program also performed satisfactorily with respect to mortality, which decreased from 15.4/100,000 population in 1964 to 7.3/100,000 in 1970, and further to rates as low as 1.8/100,000 in 1979, 1.4 in 1980, 0.4 in 2000 (Figure 1) and 0.3 in 2013.[28] Mortality was not influenced by the increase in cases observed in the early years of the 1990s.[29]
By 2009, incidence of 7/100,000 and mortality of 0.2/100,000 were reported, a result that led health authorities to propose elimination of TB,[30] as a goal for the country and priority for the PNCT.
CONCLUSIONS
The 1970 changes to Cuba’s PNCT enabled important reductions in TB incidence and mortality in later decades, and allowed health authorities to propose elimination of the disease as a current public health objective.