ABSTRACT
The Ebola virus is a pathogen that causes high morbidity and mortality in epidemic events during which health personnel are frequently infected. Such an epidemic occurred in West Africa, prompting WHO to issue a call in 2014 for health personnel to be dispatched to affected countries. Cuba responded and signed an assistance agreement under which 265 Cuban health professionals, members of the Henry Reeve Emergency Medical Contingent, volunteered their services in the Republic of Guinea, Sierra Leone and Liberia. This article presents Cuba’s strategy of medical aid and organization of the three medical teams formed; refers to the teams’ contribution to epidemic control in treatment centers where they worked alongside other personnel; and describes measures taken in Cuba to prevent the virus from entering the country through returning volunteers or other means. In the centers where Cuban medical teams worked with other health professionals in West Africa, case fatality decreased from 80%–90% to 24%, contributing to control of the epidemic; no Ebola outbreaks occurred in Cuba. During the epidemic, two Cuban health professionals died of malaria and one physician fell ill with Ebola. This paper includes an overview of the treatment and evolution of the latter case, a doctor who contracted the disease in Sierra Leone and was treated in Geneva and Havana.
KEYWORDS Ebola virus, treatment, strategy, followup, medical collaboration, Republic of Guinea, Sierra Leone, Liberia, Cuba
INTRODUCTION
Ebola virus disease (EBOV) was first identified in Africa in 1976, and was initially known as Ebola hemorrhagic fever.[1] Ebola virus affects both human and nonhuman primates, and EBOV can be serious, frequently fatal.[2]
In December 2013, a case of EBOV occurred in Guinea, in a border area near both Liberia and Sierra Leone. Given the absence of early detection and subsequent lack of measures to control virus transmission, the disease spread rapidly. The 2014–2016 epidemic in Liberia, Sierra Leone and Guinea was the largest to date, involving twice the number of cases reported over the four decades since the virus was first identified (1548 deaths from 2361 infected in 1976–2013; 11,310 deaths from 28,616 cases reported as probable, suspected or confirmed in 2014–2016, the latter reported by WHO in June 2016).[3] Recurrence is a continuing threat in the region since the virus remains in survivors’ body fluids.[4,5] A small outbreak in the Democratic Republic of the Congo in April–July 2017 claimed four lives.[6] Another outbreak there resulted in 17 deaths in May 2018; it has continued through 2019, posing danger to other African countries.[7]
IMPORTANCE At a time when a new outbreak of Ebola threatens public health in Africa and in a globalized world, this article describes Cuba’s contribution to combat the 2014–2016 Ebola epidemic in West Africa through collaboration with WHO, including training and organization of medical volunteers, infection control measures and preparedness to prevent an outbreak in Cuba upon the return of these health professionals.
In 2014, faced with the rapid spread of EBOV in West Africa, WHO declared “a public health emergency of international importance.”[8] That September, the UN and WHO put out a call for international medical collaboration to respond to the crisis and the social disaster caused by the epidemic.[9] Cuba responded on October 9, 2014 and sent a delegation to Geneva, led by its Minister of Public Health, who offered the WHO Director Cuban medical collaboration to treat the affected population. Collaboration agreements between Cuba’s Ministry of Public Health (MINSAP) and WHO were signed, under which Cuba would supply the medical and nursing personnel and WHO would finance the health professionals’ expenses in the field (a stipend to cover costs of food, lodging, etc.), with no payment to Cuba for their services.
Before 2014, there were no specific vaccines or treatments for EBOV in humans. The principal treatment consisted of supportive measures to help maintain osmotic balance, anti-inflammatory medications for fever and pain, and specific treatment for any other concomitant infection, such as malaria, tuberculosis etc. [10,11] Clinical diagnosis and correct monitoring of patients during the disease course are crucial to avoid spread of infection and to control epidemics.
CUBA´S STRATEGY TO COMBAT EBOLA
Preparing the Cuban collaborative mission A recruitment appeal elicited responses from more than 10,000 health workers willing to volunteer in West Africa. The 465 professionals selected (all men) had the relevant specialties and experience in disasters and epidemics, primarily through their work as members of the Henry Reeve Emergency Medical Contingent created for such circumstances. They received initial intensive training from Pedro Kourí Tropical Medicine Institute (IPK) personnel in Havana and WHO, followed by two further training stages, described later.
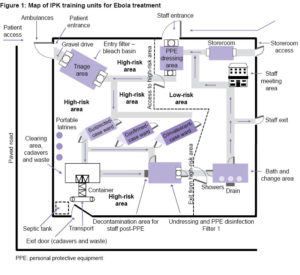
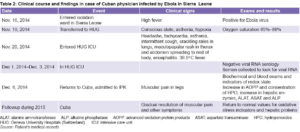
A training site was built at IPK with tents for treatment and recovery (in conditions similar to those in existing Ebola treatment centers (ETC) in Africa (Figure 1), where medical personnel learned and practiced biosafety measures such as dressing and undressing using personal protection equipment (PPE); moving through areas where suspected, confirmed or convalescing cases might be located; and exiting these areas observing correct biosafety measures. These exercises established the foundation for health personnel performance in epidemic zones. The algorithm for the biosafety measures is outlined in Box 1.
Cuba also sent medical teams to other African countries (Angola, Democratic Republic of the Congo, Gabon, Burkina Faso and Guinea-Bissau) near those experiencing Ebola outbreaks, to train Cuban and African doctors in procedures for handling Ebola patients. This training was also conducted in Jamaica and Venezuela.
Box 1: Biosafety procedures established at IPK training and Ebola treatment centers (ETC) in Africa
Admittance into the red zone, where patients are treated, is always in groups of three professionals (a doctor and two nurses or two doctors and a nurse). All personnel must wear personal protection equipment (PPE) consisting of a one-piece gown of impermeable material covering the entire body, except face and hands. Special goggles and an N-95 respirator protect the face. Cuban professionals added an extra seal around the face with cloth tape, a procedure later adopted by workers in other African ETCs. Double sets of gloves protect the hands and a protective apron covers the front of the gown. Coworkers use a permanent marker to note on the gown the name and profession of the person entering the red zone, along with time of entrance.[12]
Undressing is one of the procedures with highest risk of contamination and must be undertaken in strict observance of established steps. In the area designated for undressing, an experienced hygiene worker soaks the entire PPE with 0.5% sodium hypochlorite solution before it is removed. An expert supervises each step of the undressing procedure in order to avoid violation of safety measures from fatigue, a major reason for noncompliance with protocol, and to avoid any increased risk of contagion to individual health professionals and the community of workers.[12]
Heavy perspiration can cause the temperature inside PPE to be 4 or 5 degrees above room temperature (38–40 °C). As this can cause the wearer to lose two or more liters of liquid from sweating, there are limits to the time they can stay at the ETC.
Three treatment areas for EBOV patients were established in both training and treatment settings: the Treatment Center, the Transit Center and the Community Center.
The second stage of training for those headed to the affected countries was conducted at in-country ETCs and directed by WHO experts. The third preparatory phase consisted of training in the ETC treatment area (red zone) with patients confirmed to be infected by the virus.
A br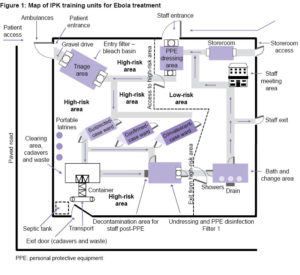 igade of 165 professionals traveled to Sierra Leone for second-stage training including 5 coordinators. A total of 160 were sent to five ETCs: 40 to Maforki, Port Loko, staffed by Partners in Health (Harvard, USA); 52 to Kerry Town with Save the Children; 30 to Waterloo/Addra under the direction of the Sierra Leone government; 21 to the Ola During Children’s Hospital; and 17 to Freetown.
igade of 165 professionals traveled to Sierra Leone for second-stage training including 5 coordinators. A total of 160 were sent to five ETCs: 40 to Maforki, Port Loko, staffed by Partners in Health (Harvard, USA); 52 to Kerry Town with Save the Children; 30 to Waterloo/Addra under the direction of the Sierra Leone government; 21 to the Ola During Children’s Hospital; and 17 to Freetown.
Another team of 60 professionals went to Liberia (including 3 coordinators), where they underwent second-stage training in ETC MOD 1 in Congo Town, in collaboration with WHO and health authorities from Liberia and the USA. They continued to be based there. A third team of 40 professionals (including 2 coordinators) traveled to Guinea for second-stage training, conducted by WHO experts in the Forécariah Transit Center. Once certified, they started working in the Coyah ETC, which the Cuban brigade helped to build. They were thus the last brigade to start their work and the last to leave the endemic zone.
Working sessions between high-ranking Cuban and WHO officials were held to establish agreements concerning organization and working conditions for volunteers. WHO officials recommended a four-week maximum of continuous presence in epidemic areas for volunteers, to avoid burnout. However, the Cuban delegation expressed preference that its medical teams stay at least six months in the affected countries, to better take advantage of their training and avoid constant redeployment and distribution of newly arrived medical personnel. Cooperants were consulted on this aspect and confirmed their willingness and commitment to the longer stay.
Organization of sanitary control, epidemiological surveillance, and diagnosis and treatment of possible Ebola carriers in Cuba To avoid spread of the infection in Cuba from possible contagious Ebola cases, international sanitary control was organized in Cuban airports. IPK built a special room for treating patients with EBOV (biosafety level 3) and purchased a high-security (also biosafety level 3) laboratory to process patient blood samples. A quarantine ward was prepared at IPK for travelers coming from areas with EBOV outbreaks, which functioned during the epidemic and through 2016. Blood samples from individuals placed in the quarantine ward and from patients with Ebola—should any present themselves—would be sent to the Canadian National Microbiology Laboratory in Winnipeg, designated by WHO to conduct diagnostic testing for any eventual Ebola cases in Cuba.
A total of 150 Cubans and 60 foreigners were admitted to the quarantine ward and kept in isolation for 21 days, monitored clinically and epidemiologically by three physicians and six nurses. The doctors, nurses and lab workers who cared for these possible Ebola cases in Cuba received training on the disease, its diagnosis, its treatment and protective measures against infection.
Cuban medical team activity in West Africa From Cuba, a technical commission led by MINSAP (composed of its officials, as well as Civil Defense, the Cuban Red Cross, IPK, and WHO/PAHO representation in Cuba) supervised the ongoing work of the Cuban medical missions in the countries affected by the epidemic.
To prevent Ebola virus infection, Cuban cooperants were instructed to avoid physical contact with local residents. Given that the main mode of contagion from Ebola is interpersonal contact via secretions, Cuban professionals also observed other prevention measures such as wearing long-sleeved shirts, using disinfectant gels, and wetting the soles of their shoes in trays of 0.5% sodium hypochlorite solution whenever they visited shopping centers or other public places.
To prevent malaria, which is endemic in Africa and the primary cause of death there, chemoprophylaxis was administered and use of repellents required. All cooperants had their temperature taken daily before breakfast, and were questioned about possible signs and symptoms of illness, receiving rapid medical attention if any responses were positive.
An indispensable requisite for the safety of Cuban personnel working in the ETCs was knowledge of Ebola’s clinical and epidemiological characteristics, as well as biosafety and infection control measures. They put into practice knowledge and procedures learned in their first- and second-stage training, including appropriate conduct in ETCs, correct PPE dressing and undressing procedures, appropriate handwashing techniques and the importance of wearing gloves for every procedure, norms concerning personnel circulation (entering and exiting high-risk zones), and observance of safety barriers. ETC red zones have three wards: one for individuals suspected of carrying the virus; one for those probably infected; and one (separated into areas for men and women) with confirmed EBOV. The wards are separated from one another by three plastic barriers placed parallel to one another with a meter between them and the area of lower risk, according to norms established for these patients.
Since the start of Ebola outbreaks, hundreds of health workers and NGO personnel have been infected for failing to comply with biosafety norms, with case fatality of greater than 50%.[13] Despite strict biosafety measures, frontline Cuban cooperants in the ETCs were not free of risk.
Shift assignment followed norms for rotation of medical and nursing personnel set by the technical commission in Cuba and international norms established by WHO. ETC work routines and biosafety measures followed a pattern similar to that employed in the IPK training unit (Box 1). Staff was on duty for shifts of six or twelve hours (8:00 AM to 2:00 PM; 2:00 PM to 8:00 PM, 8:00 PM to 8:00 AM). Shorter hours were later established due to loss of fluids and electrolytes through perspiration—resulting from PPE’s hermetic enclosure—which produces fatigue and fainting, and can increase risk of infection. Based on experiences with prior Ebola outbreaks, professional staff were divided into three working groups: one to attend to patients; a second to prepare medications and hydration solutions; and a third to observe and alert the teams to any risks.
Analysis for Ebola virus RNA in blood samples of individuals suspected of Ebola infection and those supposedly cured was conducted in a WHO-certified laboratory. This allowed for rapid transfer of infected patients to the area for confirmed cases and facilitated ETC exit by virus-free patients.
During the training sessions, WHO experts advised against any direct contact with patients, handling of intravenous catheters or of contaminated biological fluids. Cuban medical personnel, who are not accustomed to keeping their patients at a distance, and understand the importance of such interventions in healing and recovery, did insert catheters, assisted patients with drinking and eating, and bathed and dressed patients in order to promote hygiene and increase their chances of survival. The advantage of this form of handling infected patients has been demonstrated in developed countries with P4 (biosafety level 4) units where many survived and were discharged in good health. The Cuban teams obtained a higher survival rate with patients by carrying out these actions without violating safety procedures.[12]
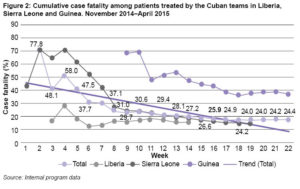
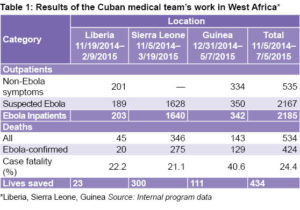
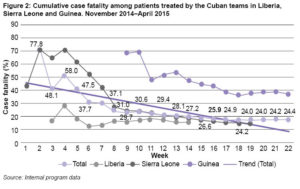
 The results of the work of the Cuban medical teams are presented in Figure 2 and Table 1. Initially, the fatality rate in ETCs was 80%–90%. This was reduced to 24% through comprehensive treatment of clinical manifestations (vomiting, diarrhea, fever) and administration of parenteral electrolytic solutions to patients to restore and maintain electrolyte balance.
The results of the work of the Cuban medical teams are presented in Figure 2 and Table 1. Initially, the fatality rate in ETCs was 80%–90%. This was reduced to 24% through comprehensive treatment of clinical manifestations (vomiting, diarrhea, fever) and administration of parenteral electrolytic solutions to patients to restore and maintain electrolyte balance.
In 2017, WHO rewarded the Henry Reeve Emergency Medical Contingent’s work with the Dr Lee Jong-Wook Memorial Prize for Public Health.[14] The volunteers were also featured in video documentaries and testimonies in a book by Enrique Ubieta Gómez, Red Zone: The Cuban Experience with Ebola.[15]
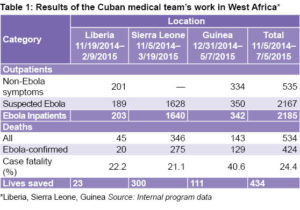
A CUBAN HEALTH PROFESSIONAL WITH EBOLA:OVERVIEW OF TREATMENT AND CLINICAL COURSE
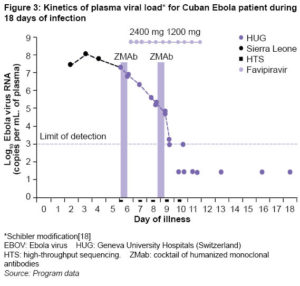
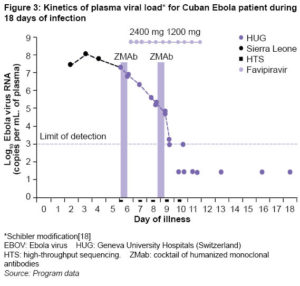
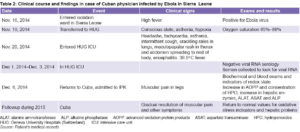
Despite strict biosafety measures, a 43-years-old Cuban doctor who worked in Sierra Leone was infected with Ebola virus. After admission to an isolation ward in Sierra Leone, he was transferred to the Geneva University Hospitals (Switzerland) where he was treated with a cocktail of humanized monoclonal antibodies (ZMab, Mapp Biopharmaceutical, USA), considered a promising candidate for Ebola treatment,[16] as well as favipiravir, an antiviral that inhibits RNA polymerase (released for use during the 2014 Ebola epidemic, with good results).[17,18] Treatment with the two medications reduced viral load in a few days and made RNA virus undetectable (Figure 3). In December 2014, when the patient was declared cured and not contagious, he returned to Cuba and was admitted to the IPK Hospital during periods in 2014–2015, where he began additional treatment with Vimang, a Cuban antioxidant product extracted from mango tree bark and known for its beneficial effect on infection.[19] He continued to be monitored for various biomarkers, as noted in Table 2. To date, he has shown none of the sequelae observed in other survivors, such as vision and central nervous system problems, among others.[20,21]
LESSONS LEARNED
At the time of writing, there are still no specific treatments for EBOV. Some triple monoclonal antibodies have shown promising results[16] and antiviral medications and injections are being developed.[16,17] Conventional treatment in epidemics is intravenous water and electrolytes to recoup the loss of liquids from diarrhea and vomiting, and reestablish electrolyte balance; oxygen therapy to maintain high saturation levels; medication to lower fever, reduce pain and maintain blood pressure within normal ranges to reduce vomiting and diarrhea; and blood transfusions.[22] Cuban cooperants enhanced treatment with attention to personal hygiene, feeding and oral rehydration of their patients as part of medical and paramedical care, while still observing biosafety measures and obtaining good survival results.[12] This provided an important lesson, that this type of patient care should be included in the treatment regime, breaking the barriers of prejudice and fear of contagion associated with Ebola.
As mentioned above, administration of ZMab and favipiravir to the infected Cuban cooperant quickly reduced viral load to undetectable levels (Figure 3). The efficacy of triple humanized monoclonal treatment is still debated because clinical trials have been few[17], and the single clinical trial of favipiravir found it ineffective in patients with a high viral load, observing adverse renal reactions.[23] So perhaps biological conditions, specific virus variant, and initial viral load contributed to the favorable outcome in the Cuban patient and could be useful prognostic factors for treatment in future epidemics.
While use of antioxidants to modify the redox environment in patients with acute and chronic disease has been the subject of multiple studies, antioxidants are considered nutritional supplements, not drugs. One reason is that oxidative stress is not classified as a disease but is associated with a broad spectrum of diseases and is unrelated to any specific syndrome.[18] According to the Napralert Natural Products Data Base (University of Illinois, USA), extract of mango tree bark is an antioxidant widely used in natural medicine in many countries to treat infections.[24] The Cuban extract, known by its commercial name Vimang, showed good clinical and laboratory results when administered to the Cuban patient (Table 2) and could be considered for inclusion in treatment regimens for Ebola patients after the acute phase of illness.
This was the only Cuban medical volunteer to fall ill with Ebola. After recovery, he returned to Sierra Leone to complete his mission, and is now back in Cuba. Two others became ill with malaria and died, one in Guinea and the other in Sierra Leone.
One lesson the world learned from the 2014–2016 Ebola epidemic was that global health authorities did not recognize the international emergency nature of this epidemic in time. Another observation is that many governments did not become involved in providing care for sick people in Africa whose numbers were increasing daily—until the first case of Ebola was reported outside the continent in July 2014.[25] Others did send both human and material resources; and in any case, the greatest burden was borne by local public health authorities and professionals, as well as nongovernmental organizations (including Médecins Sans Frontières), which established services to diagnose, treat and prevent Ebola’s spread.[26]
Cuba was an example of a country with limited resources responding quickly and effectively to WHO’s call, by sending teams of health professionals trained in patient management and establishing a strategy to limit or prevent outbreaks of the disease within its own borders after volunteers returned.
CONCLUSIONS
Given the slow and inadequate international response initially to the Ebola epidemic, the Cuban health system played a prominent role, in number of professionals mobilized, technical quality of their intervention, and their disciplined sense of responsibility. Training experienced health workers before leaving for the ETCs in the affected countries ensured the quality of their work and protection against infection by the virus. Without neglecting the necessary sanitary controls designed to minimize risk to professionals and the possibility of introducing the pathogen into Cuba, these Cubans cared for patients in close collaboration with international, national and local health authorities, with high levels of commitment to their work.
Nevertheless, the epidemic tested Cuba’s capacity to mobiize in the face of health emergencies far from its national borders, as well as to effect measures to stop EBOV infection from becoming a health problem in the country itself. The experience proved that, even with limited resources, proper international and domestic health control measures can avoid outbreaks and epidemics of the disease. Finally, the Cuban health professionals who volunteered, successfully addressing the disease, also brought back lessons in clinical care and human solidarity in emergency situations, highly useful for future missions of the Henry Reeve Emergency Medical Contingent and other Cuban global health cooperation efforts.
ACKNOWLEDGMENTS
Thanks to all the Cuban health professionals who fought Ebola in West Africa; to Dr Jérôme Pugin and specialists from the Geneva University Hospitals for their care of the Cuban Ebola patient; to Dr Felix Báez, infected with the virus, for his valuable contribution and for allowing collection of samples for followup; to IPK specialists who taught training courses and the doctors assisting them in quarantine upon return; and to all those who worked with Cuban collaborators to stem Ebola in West Africa.
References

- Zampieri CA, Sullivan NJ, Nabel GJ. Immunopathology of highly virulent pathogens: insights from Ebola virus. NatImmunol. 2007 Nov;8(11):1159–64.
- Kuzmin IV, Schwarz TM, Ilinykh PA, Jordan I, Ksiazek TG, Sachidanandam R, et al. Innate immune responses of bat and human cells to filoviruses: commonalities and distinctions. J Virol. 2017 Apr 15;91(8).
- Singh RK, Dhama K, Malik YS, Ramakrishnan MA, Karthik K, Khandia R, et al. Ebola virus – epidemiology, diagnosis, and control: threat to humans, lessons learnt, and preparedness plans – an update on its 40 year’s journey. Vet Q. 2017 Dec;37(1):98–135.
- Jiang T, Jiang JF, Deng YQ, Jiang BG, Fan H, Han JF, et al. Features of Ebola virus disease at the late outbreak stage in Sierra Leone: clinical, virological, immunological, and evolutionary analyses. J Infect Dis. 2017 Apr 1;215(7):1107–10.
- Deen GF, McDonald SLR, MarrinanJE, Sesay FR, Ervin E, Thorson AE, et al. Implementation of a study to examine the persistence of Ebola virus in the body fluids of Ebola virus disease survivors in Sierra Leone: methodology and lessons learned. PLoSNeglTrop Dis. 2017 Sep 11;11(9):e0005723.
- Mérens A, Bigaillon C, Delaune D. Ebola virus disease: biological and diagnostic evolution from 2014 to 2017. Med Mal Infect. 2018 Mar;48(2):83–94.
- France Presse. La OMS declara el Ébola “emergencia de salud pública” mundial. El Mundo [Internet]. 2019 Jul 17 [cited 2019 Aug 15];Internacional:[about 2 screens].Available from: https://www.elmundo.es/internacional/2019/07/17/5d2f651ffdddffb9698b46f3.html. Spanish.
- Corporación de Radio y TV Españolas Online [Internet]; c2019. Madrid: Radio y Televisión Españolas. Noticias. La Organización Mundial de la Salud (OMS) decreta una alerta mundial por el brote de Ébola;2014 Aug 8 [cited2019Aug 21]. Available from: http://www.rtve.es/noticias/20140808/organizacion-mundial-salud-decreta-alerta-mundial-brote-ebola/989502.shtml.Spanish.
- Karamouzian M, Hategekimana C. Ebola treatment and prevention are not the only battles: understanding Ebola-related fear and stigma. Int J Health Policy Manag. 2014 Dec 2;4(1):55–6.
- Geisbert T, Hensley L, Larsen T, Young H, Reed D, Geisbert J, et al. Pathogenesis of Ebola hemorrhagic fever in cynomolgusmacaques. Am J Pathol. 2003 Dec;163(6):2347–70.
- Manejo clínico de los pacientes con fiebre hemorrágica: Guía de bolsillo para personal sanitario de primera línea 2014. Geneva: WorldHealthOrganization; 2014 Dec.154 p. Spanish.
- Carballo Herrera R. Memorias de un enfermero cubano cara a cara con el Ébola en Guinea Conakry. Rev Cubana Enferm. 2018;34(2). Spanish.
- Maguina Vargas C. Enfermedad por el virus del Ébola. Rev Med Hered. 2015;26(3):195–201. Spanish.
- World Health Organization [Internet]. Geneva: World Health Organization; c2019. Media Center. Dr Lee-Jong-wook Memorial Prize for Public Health 2017; 2017 May 26 [cited 2019 Aug 21]; [about 2 screens]. Available from: https://www.who.int/mediacentre/events/2017/wha70/lee-jong-wook-prize/en/
- Ubieta Gómez E. Zona Roja: la experiencia cubana del Ébola. Havana: Editorial Abril; 2016 Apr 1. 254 p. Spanish.
- Moekotte AL, Huson MAM, van der Ende AJ, Agnandji ST, Huizenga E, Goorlis A et al. Monoclonal antibodiesforthetreatment of Ebola virus disease. Expert Opinion Invest Drug [Internet]. 2016 Oct 8 [cited 2019 Aug 22];25(11):1325–35. Available from:https://www.tandfonline.com/doi/full/10.1080/13543784.2016.1240785
- Moneriz C, Zapata S. Avances científicos en las estrategias terapéuticas contra la enfermedad por virus del Ébola. Biosalud [Internet]. 2016Dec [cited 2019 Aug 21];15(2):87–105. Available from:https://temas.sld.cu/ebola/2018/04/05/avances-cientificos-en-las-estrategias-terapeuticas-contra-la-enfermedad-por-virus-del-ebola/. Spanish.
- Schibler M, Vetter P, Cherpillod P, Petty TJ, Cordey S, Vieille G, et al. Clinical features and viral kinetics in a rapidly cured patient with Ebola virus disease: a case report. 2015 Sep;15(9):1034–40.
- Núñez SellésAJ, Guevara García M, Álvarez León A, Pardo Andreu GL. Experiencias de la terapia antioxidante con Vimang en la atención primaria de salud en Cuba. Rev Cubana Salud Pública [Internet]. 2007 Jul–Sep [cited 2019 Agu22];33(3). Available from: http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S0864-34662007000300017&lng=es.
- Petrosillo N, Nicastri E, Lanini S, Capobianchi M, Caro A, Antonini M, et al. Ebola virus disease complicated with viral interstitial pneumonia: a case report. BMC InfectDis. 2015 Oct 16;15:432.
- Ji YJ, Duan XZ, Gao XD, Li L, Li C, Ji D, et al. Clinical presentations and outcomes of patients with Ebola virus disease in Freetown, Sierra Leone. InfectDisPoverty. 2016 Nov 3;5(1):101.
- Ducharme J. Experimental Ebola Treatments Look Successful in Lab Studies, Says the CDC. TIME [Internet]. 2019Jul 10 [cited 2019 Aug 22];Health:[about 2 screens]. Available from:https://www.cdc.gov/vhf/ebola/treatment/index.html
- Sissoko D, Laouenan C, Folkesson E, M’Lebing AB, Beavogui AH, Baize S, et al. Experimental treatment with favipiravir for Ebola virus disease (the JIKI Trial): ahistorically controlled, single-arm proof-of-concept trial in Guinea. PLoS Med [Internet]. 2016 Mar [cited 2019 Aug 22];13(3):e1001967.Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4773183/
- Napralert Database [Internet]. Illinois: University of Illinois; c2019 [cited 2019 Aug 22]. Available from:http://apps.who.int/medicinedocs/es/m/abstract/Js21282en/
- Kaner J, Schaack S. Understanding Ebola: the 2014 epidemic. Global Health [Internet]. 2016 Sep 13 [cited 2019 Aug 22];12(1):53. Available from: https://globalizationandhealth.biomedcentral.com/articles/10.1186/s12992-016-0194-4
- Liu J. Pushed to the Limit and Beyond: A Year into the Largest Ever Ebola Outbreak. 2015. Médecins Sans Frontières [Internet] 2015 Mar 3 [cited 2019 Aug 22]. Available from: http://www.msf.org/en/article/ebola-pushed-limit-and-beyond
THE AUTHORS
Jorge Pérez Ávila (Corresponding author: jorge.perez@ipk.sld.cu), physician specializing in pharmacology with a master’s degree in clinical pharmacology and infectology. Consulting professor and associate researcher, Academic Department, Pedro Kourí Tropical Medicine Institute (IPK), Havana, Cuba.
Daniela Núñez-Monteagudo, pharmacist, Pharmacy Department, Pharmacy and Foods Institute, University of Havana, Cuba.
Mayra Muné-Jiménez, microbiologist with a master degree in virology and a doctorate in health sciences. Full professor and senior researcher, Virology Department, IPK, Havana, Cuba.
Lizette Gil del Valle, Biochemist. Associate professor, senior researcher and head, Department of Pharmacological Research, IPK, Havana, Cuba.
Madelyn Garcés-Martínez, physician specializing in microbiology with a master’s degree in epidemiology. Associate professor, adjunct researcher and head, Department of Biosafety, Health and Hospital Epidemiology, IPK, Havana, Cuba.
Roberto Fernández-Llanes, physician specializing in microbiology with a master’s degree in virology. Full professor and senior researcher, IPK, Havana, Cuba.
Lorenzo Somarriba López, physician specializing in health administration. Assistant professor and head, Epidemic Management, Ministry of Public Health, Havana, Cuba.
Submitted: January 03, 2019 Approved: September 08, 2019 Disclosures: None