For this domain, all three countries demonstrated strong government involvement and willingness to set up institutions to lead the response. South Africa and Zimbabwe have involved more line ministries in the national coordination taskforce to improve inter-ministerial cooperation and streamline the delegation of responsibilities.
Policy framework Within a few weeks of its formation, the Rwandan Joint Task Force for COVID-19 put forward a national policy on COVID-19 prevention within communities, places prone to large gatherings of people, markets, and other crowded places such as bus stations.[13] Clinical tools and guidelines were quickly developed and shared to help heath care providers manage testing, and also offer instructions as to how to access services after exposure.[13] By March 2020, various containment and mitigation measures had been put in place.[14] These included lockdowns, restricted movement between Kigali and other provinces, reducing the number of traders in markets and closing markets with high rates of transmission, closing schools and churches, and isolating regions with transmission clusters in lockdown.
A similar response was observed in South Africa. Building on the declaration of COVID-19 as a national disaster by the Minister of Cooperative Governance and Traditional Affairs, a national policy including various clinical tools and guidelines were put in place in South Africa.[15]
At the time this article was written, our search could not find a COVID-19 policy on the Zimbabwean Ministry of Health and Child Care website. However, the Ministry of Health and Child Care had published a COVID 19 National Preparedness and Response Plan.[3] The plan includes prevention, containment and mitigation strategies for different COVID-19 transmission scenarios.[16]
The existence of a COVID-19 national policy that covers the major response areas in public domain or on the government websites is critical for guiding national responses. In this context, Rwanda moved with respective alacrity, establishing policies that allowed for rapid introduction of strict prevention and control interventions.
Risk communication and community engagement Our literature search showed that all three countries have employed the use of SMS text alerts, videos, infographics and posters to alert the public to the dangers of
COVID-19. Public and private radio and television were also used to disseminate information. A compendium of key messages has been developed and these guide other partners involved in the COVID-19 response in the development of information, education and communication activities. There were no clear differences among the three countries in risk communication and community engagement strategies.
Surveillance, rapid response teams and case investigation All three countries have set up systems actively involved in case detection, quarantine and isolation. In South Africa, community health workers conduct house-to-house screening and testing, especially in vulnerable communities. In Rwanda and Zimbabwe, rapid response teams investigate suspected cases and support the surveillance task force at subnational levels through data reporting, capacity building and supportive visits.[3] However, in Zimbabwe, there were reports of rapid response teams in the first wave (July–August 2020),[17] but at the time of this writing there was no literature available which would reveal whether the number of these increased during Zimbabwe’s COVID-19 resurgence from mid-December 2020 through the end of January 2021.
Infection prevention and control A major component of the COVID-19 response has been infection prevention and control (IPC). All three countries have implemented COVID-19 IPC response plans, albeit with logistical and personnel challenges.[17] In Rwanda and South Africa, various mitigation measures were put in place; including limiting visits to healthcare facilities, screening all patients for COVID-19 symptoms and patient triage. Healthcare facility staff receive routine training on COVID-19 risk reduction.[18] Similarly, in Zimbabwe, IPC reference materials for reducing COVID-19 exposure risks were developed rapidly and distributed in health facilities and within communities in an effort to better capacitate healthcare workers (HCWs) to provide safe community environments. The literature in this review revealed that the Zimbabwean IPC response was affected by staffing shortages, lack of motivation among HCWs and personal protective equipment (PPE) shortages.[17] In this regard, Rwanda and South Africa had more engaged volunteer health workers[19] and reassigned HCWs who had switched to employment outside the health sector.
Case management and continuity of essential services All three countries have active case management systems functioning at varying degrees of efficiency. Their objectives are to provide timely high-quality care for COVID-19 patients; to ensure adequate capacity for managing COVID-19 cases during all phases of the pandemic, including during case surges; and to ensure routine essential health service delivery continuity and utilization during all phases of the pandemic and beyond.
In Rwanda, clinical management guidelines were continuously updated to reflect new guidance from WHO. South Africa utilized various action plans recommended by WHO, among them mapping vulnerable populations, as well as public and private health facilities and workforces, thereby identifying alternative facilities for treatment. Similarly, Zimbabwe released guidelines for the clinical management of COVID-19 that covered testing, case management, antiviral treatment and patient discharge. While there was evidence on the existence of such guidelines in all three countries, our literature search did not reveal evidence on the quality or efficiency of case management.
Essential services in Rwanda remained functional, if depleted. However, movement restrictions and bans on public transportation impeded access to non-COVID healthcare services. For instance, one study reported that less than half of HIV–positive patients attended their antiretroviral collection clinic appointments during the first lockdown period in March–April 2020.[20] In South Africa, the healthcare facilities were continuously assessed to ensure continued capacity in delivering primary and other essential services. Furthermore, the private for-profit healthcare system in South Africa in general is very active in care management; mainly attending to patients with medical insurance.
In Zimbabwe, although essential services remained open during the lockdown period, movement restrictions and fear of contracting COVID-19 at healthcare facilities affected utilization of such services for other public health threats.[21] A report by the Zimbabwean Ministry of Health and Child Care revealed that during the period of April–June 2020 there was a 59% reduction in the number of clients tested for HIV who received their results; 15% reduction in the distribution of HIV self-test kits; 99% reduction in voluntary medical male circumcisions performed; a 49% reduction in patients tested for syphilis; 46% reduction in pregnant women booking for first prenatal appointment; 51% reduction in newly diagnosed HIV patients initiated on antiretroviral therapy and a 29% decline in viral load sample collection in Zimbabwe. One observation is that Rwanda and Zimbabwe could benefit from scaling up telehealth utilization, as reportedly used in South Africa,[22] to support essential services’ continuation during the pandemic.
National laboratory system COVID-19 tests in Rwanda were initially performed at the National Reference Laboratory (NRL) before a new testing strategy was introduced to decentralize capacity through peripheral district laboratories. The Rwandan laboratory system started off (in March 2020) with the capacity to test close to 1000 samples per day but in 4 months (by July 2020), the testing capacity increased 15-fold with a shift from manual RNA extraction to an automated system providing results more quickly (pooling system).[11,23,24] This was due in part to the introduction of a mobile laboratory unit in May 2020 that doubled the country’s COVID-19 testing capacity, its mobility facilitating mass testing throughout the country.
The South African COVID-19 response laboratory is led by the National Institute of Communicable Diseases (NICD). Rapid testing expansion was enabled by a large network of private and National Health Laboratory Services (NHLS) laboratories. As with Rwanda, South Africa has employed mobile laboratories to expand testing.
Zimbabwe has a national-level laboratory system whose objectives include capacitating laboratories to perform molecular diagnosis using real-time reverse transcription polymerase chain reaction (RT-PCR) with demonstrated quality and biosafety; ensuring adequate supplies of test kits and reagents; increasing access to testing at provincial level using GeneXpert (Cepheid); strengthening COVID-19 testing support systems including data collection and analysis, waste and sample management; and establishing and strengthening COVID-19 testing quality assurance systems. Major impediments to this system are inadequate resources, specifically the lack of test kits and an ineffective sample transportation system to the few available testing centers.
The success of the Rwandan laboratory system has been attributed to population and governmental goodwill, research-based actions, optimized use of available human resources, and the use of limited resource funding models to support the established public laboratory and health system governance structures.[25] In this regard, there was very little available literature on how Zimbabwe approached scaling up research-based testing. The South African COVID-19 laboratory response relies on sufficient resources, now available at the national level, and includes routine genomic typing of the COVID-19 variants as part of surveillance.
Role of private sector in national response The COVID-19 response in all three countries has seen governments working closely with stakeholders from across the private sector, civil society, academia, professional associations, the private nonprofit sector, community-based organizations and international organizations. In all three countries, for example, a key role for the private for-profit healthcare systems has been in the provision of COVID-19–related treatment and care;[26] PPE for medical staff in under-resourced hospitals; and rapid test kits, hand sanitizers and food hampers to vulnerable communities.[27,28] There was no literature in our review showing any marked differences in private sector engagement in COVID-19 responses in all three countries.
Points of Entry All three countries are in compliance with WHO International Health Regulations (IHR).[29] The purpose of the IHR is to “prevent, protect against, control and provide a public health response to the international spread of disease in ways that are commensurate with and restricted to public health risks, and which avoid unnecessary interference with international traffic and trade.” In Rwanda, a negative COVID-19 PCR test is required at any of the entrance points. A repeat test is conducted upon arrival while travelers are in a mandatory 24-hour quarantine.
South Africa and Zimbabwe require a negative COVID-19 PCR test taken 72 and 48 hours, respectively, prior to arrival. No retesting is conducted at the airport. The Zimbabwean point-of-entry approach leverages a mature strategic information (SI) system. (The Zimbabwean port-of-entry screening system has screened over 120,000 individuals over the 6 months from June through November, 2020). The festive season period saw the Zimbabwe–South Africa Beitbridge border post experiencing a huge influx of people crossing the border. There were reports of a high number of fake COVID-19 clearance certificates by travelers from Zimbabwe resulting in South African authorities resorting to testing every traveler passing through the border post before allowing them to enter the country.[30] Another threat faced by both Zimbabwean and South African COVID-19 responses are people entering both countries using undesignated entry points. The Rwandan strategy of repeat testing could help South Africa and Zimbabwe address the threat of the fake COVID-19 certificates.
COVID-19 logistics, supply and procurement implementation/ operational plan We found very little literature on COVID-19 logistics, supply and procurement implementation in the three countries. The available evidence suggests that all three countries have set up systems to map available resources and supply systems in their healthcare sectors. However, just like other African countries, Rwanda, South Africa and Zimbabwe have been affected by shortages of diagnostic kits due to disruptions in the global supply chain.[31] Furthermore, reports of COVID-19 procurement-related corruption (concerning contracts for products and services related to COVID-19) have hampered the response in South Africa[32,33] and Zimbabwe.[34,35]
The COVID-19 response has exacerbated the need for South Africa and Zimbabwe to establish measures to curb corruption within their governments. In this regard, the Rwandan model could serve as an exemplar. The Rwandan government formulates and implements anti-corruption efforts mainly via homegrown initiatives, minimizing corruption by eradicating opportunities for misconduct, focusing on governance reforms and maintaining a zero-tolerance policy towards corruption.[36] Political will, strong leadership, the active role played by the anti-corruption agency and effective governmental reforms have made Rwanda’s anti-corruption activities largely successful in the context of the pandemic.[36]
DISCUSSION
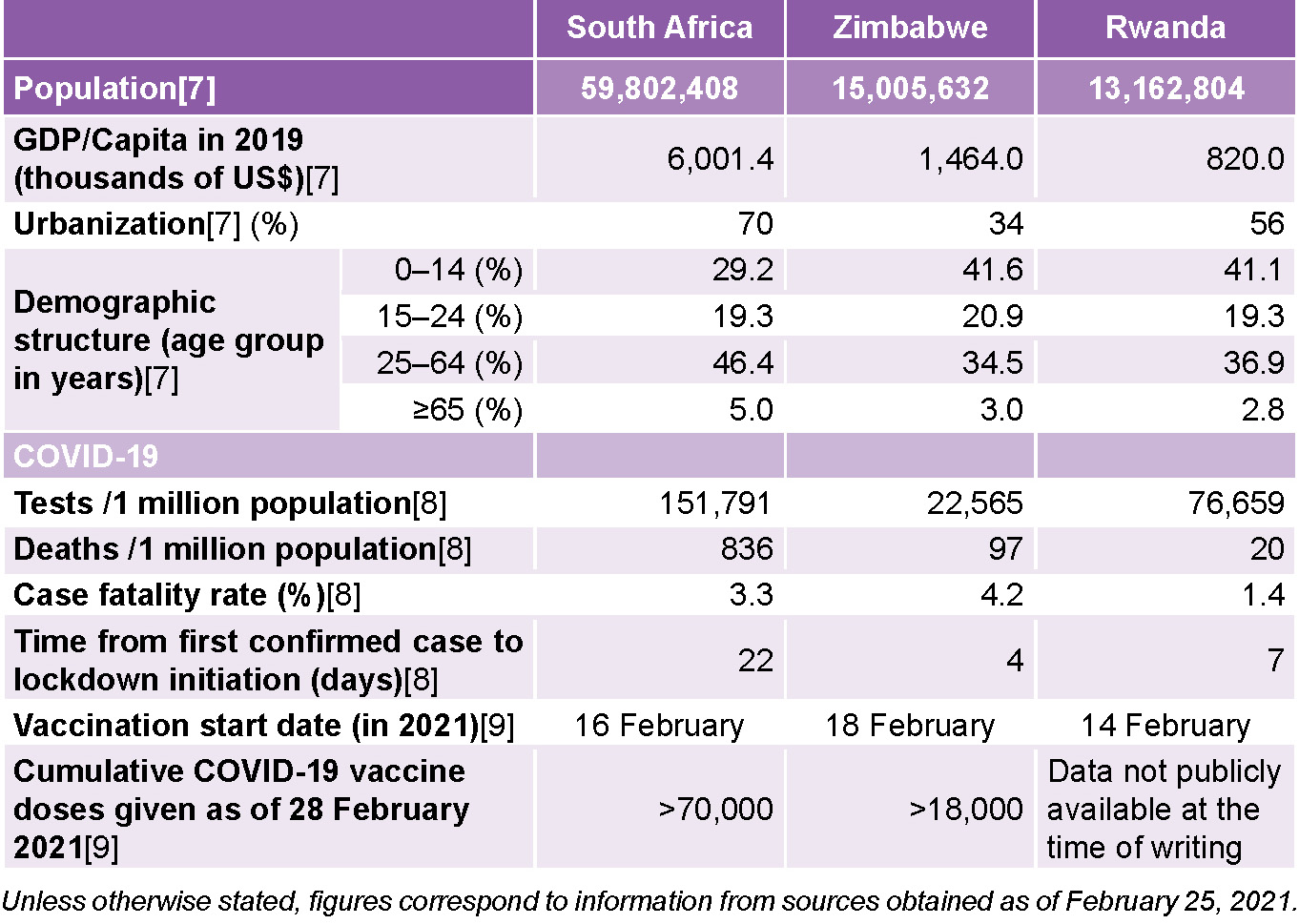
COVID-19 burdens in these countries vary, with South Africa experiencing the worst epidemic of the three. The ten comparison domains discussed above influence the burden of COVID-19 in each of the countries, albeit there are concerns on the reliability of reported data due to the poor surveillance systems in place in Africa.
In general, countries with strong, coordinated government responses have experienced far less severe COVID-19 epidemics than countries with more ad hoc or laissez faire approaches. While most African countries have under-resourced health systems, many of them also have very robust public health systems, an important asset in disease mitigation and containment during a pandemic.
Our findings revealed some critical response areas where the three countries could learn from each other. For instance, Rwandan response could learn from South Africa and Zimbabwe on inter-ministerial coordination and involve more line ministries in the national coordination taskforce to improve inter-ministerial cooperation and streamline delegation of responsibility. Regarding framing and implementing policies, South Africa and Zimbabwe could learn from Rwanda to improve their speeds in implementing and establishing COVID-19 policies and making them available in the public domain. The existence of a COVID-19 national policy that covers major response areas in the public domain or on government websites is critical to guiding the response in any country.
Zimbabwe could learn from Rwanda and South Africa in devising innovative ways to improve the health worker staff complement as these are critical frontline workers in the pandemic response. Rwanda and Zimbabwe could learn from South Africa’s rapid expansion of telehealth services to ensure the continuation of health services during the lockdown period. Finally, South Africa and Zimbabwe could learn from Rwanda’s response to corruption, which has hampered their two countries’ supply chains and logistics. In Rwanda’s case, political will and strong leadership, the active role played by the anti-corruption agency, and effective governance reform have prevented mismanagement of COVID-19 resources or procurement processes.
Between 2015 and 2017, the doctor–inhabitant ratio improved in Rwanda, from 1:15,428 to 1:8,592, while the nurse–inhabitant ratio improved from 1:1200 to 1:1070.[37] Rwanda is among the few countries in Africa to have achieved universal health coverage based on a vision of inclusiveness, equity, and comprehensive and integrated services, with a focus on primary health care (PHC).[37] Not surprisingly, Rwanda has been ranked first in Africa and sixth globally in managing the COVID-19 pandemic and making information about the pandemic accessible to the public.[38]
According to the World Bank, Rwanda has 0.1, South Africa 0.9, and Zimbabwe 0.2 physicians per 1000 population.[39] The same source reports that Rwanda has 1.2, South Africa 1.3, and Zimbabwe 1.9 nurses or midwives per 1000 population.[38] Regarding COVID-19 deaths per 1 million population, Rwanda has 14 (ranked 34th in Africa), South Africa 730 (ranked 1st in Africa) and Zimbabwe 77 (ranked 13th in Africa).[40] Interestingly, South Africa, with the highest proportion of physicians, also shows the highest proportion of Coronavirus deaths per 1 million. It is also worth noting that South Africa has become the first country in Africa to receive a shipment of COVID-19 vaccines.
CONCLUSIONS
Frequently, analyses about Africa are based on viewpoints formulated outside the continent. We have intentionally avoided this approach. Our perspective is based on a narrative literature review, consisting mainly of documents elaborated by African policymakers. Nevertheless, it has some limitations. Firstly, as an analysis based on a literature review, steps in systematic evidence synthesis were omitted. These include quality assessment of the findings. Second, our search was limited in scope and depth. For instance, we did not screen references in the reviewed papers. However, findings in the present study still offer important insights as to similarities and differences in COVID-19 response strategies across three countries in Africa that have experienced varying impacts from the pandemic.
The findings allow for each country’s COVID-19 response leaders to learn from the others and may also serve as a guide for similar settings with limited resources on the best practices for curbing the pandemic’s spread.
For example, Rwanda could learn from South Africa on strategies to ensure continuation of essential services during lockdown. South Africa and Zimbabwe could learn from Rwanda’s response to corruption, a factor that has hampered the two countries’ supply chains and logistics. Zimbabwe could learn from Rwanda and South Africa in devising innovative ways for strategic health worker deployment. All three countries can benefit from exchanging lessons they have been learning during the pandemic and by establishing routine meetings to share their experiences.