ABSTRACT
Vaccination is one of the most cost-effective interventions for control of communicable diseases. This health achievement could flounder if measures are not taken by health systems to prioritize immunization, increase vaccination rates and educate health professionals to address public concerns about vaccine safety and efficacy. Parents’ refusal to vaccinate their children directly affects public health, because it puts both individual and group immunity in danger; immunization coverage is effective only when high population coverage is attained. The growing number of antivaccination (antivaxxer) groups around the world is alarming, contributing to falling vaccination rates. Troubling consequences include disease outbreaks in several countries globally and in our hemisphere. This article looks at the history and features of antivaxxer movements around the world and proposes ways the Cuban health system, through its National Immunization Program, can address dangers for the population associated with potentially negative influences of social-network antivaxxer campaigns. The paper underscores the role of mass and social media, health professional training and sustained competence, and the importance of a vaccine-related adverse events surveillance system.
KEYWORDS Vaccination, immunization, antivaccination movement, antivaccine groups, primary health care, society, communications media, social media, Cuba
INTRODUCTION
Vaccination is one of the most cost-effective actions to prevent infectious diseases. Every year vaccinations prevent an estimated 2.5 million deaths of children aged <5 years.[1–4]
Despite this indisputable health achievement, vaccination refusal by citizens (parents in particular) and even some health professionals is on the rise. In general terms, vaccine refusal is defined as the temporary or permanent refusal of parents to allow administration of one, several, or all vaccines for their children.[5]
Such refusal imperils immunization as a fundamental pillar of global public health policy and practice. Refusals are based on reservations about vaccination safety not founded on scientific evidence, but rather on lack of information or distorted information from unreliable sources, distrust resulting from false rumors about possible adverse reactions, and occasionally on high costs of vaccines not covered by health systems.[6]
The hesitancy tends to be based on isolated episodes rarely related to problems with the vaccines themselves. Increasingly, hesitancy has led to outright refusal, stoked by a growing antivaccination movement, dubbed “antivaxxers.” This movement’s influence through social and other media is hindering immunization programs, with serious consequences for the public’s health. This is due to the fact that both individual and group immunity are endangered when individuals refuse to be vaccinated or parents refuse vaccination for their children: herd immunity is only effective when a population’s vaccination rates are high.
IMPORTANCE This article explores antivaccination movements’ Internet presence and their activities’ impact on global public health contrasted with broad public understanding and acceptance of vaccination in Cuba, proposing ways to maintain public trust in vaccine safety to sustain the country’s high immunization coverage.
Certain infectious diseases can only be eradicated with vaccination, and antivaccination movements today constitute a major obstacle to reaching that objective.[6,7] At risk are millions of lives due to the reappearance of once- or near-eliminated diseases and indefinite postponement of eradication deadlines for diseases thought to be close to eradication.[8]
This threat makes it ever more important for immunization programs to a) increase vigilance to ensure that vaccines used are of high quality, thoroughly tested for safety and efficacy; b) invest in robust surveillance of vaccine-related adverse events; and c) prepare health workers to address public concerns about vaccine safety and practices by providing them the most current information from both national and international sources, and establishing specific venues for its dissemination.[9] Given the ubiquitous nature of social networks, health personnel should be encouraged to use them, in addition to other media and opportunities, to confront the spread of misinformation about vaccination, contributing their experience and knowledge to the debate.
TO VACCINATE OR NOT TO VACCINATE
Society and antivaccination movements The role of society is fundamental to sustain vaccination programs. Often, however, incomplete or distorted information circulates about vaccine benefits and safety. Moreover, vaccination programs can be “the victim of their own success” for at least two reasons. First, reduced incidence of a particular disease may make people think it is no longer a risk (reduced risk perception). Second, substantial drops in morbidity and mortality following the introduction of vaccines has paradoxically made adverse events more visible, exaggerating perceived vaccine risks, and contributing to weakened adherence to immunization programs.[10] Antivaxxer movements have mainly sprouted in developed countries, but as a result of globalization, they are spreading into low- and middle-income countries as well.
Vaccine refusal is not a new phenomenon; it appeared with the earliest immunization efforts in the world. One 20th-century situation that involved several continents was the 1970 controversy about the safety of the diphtheria, tetanus and pertussis (DTP) vaccine. In the UK, doubts arose following media reports about a London pediatric hospital, claiming that children immunized with the vaccine developed neurological disorders. Many physicians opposed vaccination and reported cases linking DTP with neurological disorders. As a result, vaccination rates fell and three outbreaks of whooping cough followed. Immunization rates rose only after the Joint Committee on Vaccination and Immunization organized a study showing that vaccination-related risk for neurological diseases was extremely low.[11] In the USA, a similar controversy erupted in 1982 when a television documentary reported supposed adverse reactions to DTP. Parent groups began opposing vaccination of their children, but energetic responses from Centers for Disease Control and medical associations kept immunization rates from falling as drastically as they had in the UK.[11]
The biggest controversy in recent years was touched off in 1998, with Dr Andrew Wakefield’s article in The Lancet, questioning the safety of the triple vaccine against measles, mumps and rubella (MMR). Although he did not directly blame MMR for the occurrence of ileocolonic lymphoid nodular hyperplasia and neurological disorders (both commonly associated with autism spectrum disorder) in 12 previously normal children, he affirmed that the parents of 8 of the children associated the date of symptom onset with vaccination, and stated that the disease was the result of an “external trigger.”[12]
This assumption unleashed a media campaign that spread fear among parents, with many in the UK refusing to vaccinate their children. In 2004, Dr Richard Horton, editor of The Lancet, stated that the article should not have been published because it was based on a clear conflict of interest. An investigation by the UK’s General Medical Council revealed that a law firm representing the interests of parents of children supposedly harmed by the vaccine had paid Wakefield to explore evidence of this association. The Council ruled against Wakefield and he lost his medical license.[11] The Lancet retracted the article in 2010[13] and in 2011 the British Medical Journal reported that Wakefield’s arguments were based on weak evidence. Some of the most egregious inaccuracies found were:
- not all the children were correctly diagnosed with autism (only 3 of 9);
- of the 12 children classified as neurologically normal before vaccination, 5 had developmental disorders; and
- onset of symptoms claimed to be within days of vaccination actually had appeared months later.[14]
It has been shown that neurological and autoimmune and degenerative diseases that provoke such controversies are not the result of vaccination,[15] and that benefits (both individual and collective) of vaccination programs far outweigh possible adverse events;[16,17] the scientific evidence on vaccine safety is overwhelming.[16,18]
The effects of mass vaccination on incidence of measles have been well documented throughout the world, and countless studies in the field confirm the efficacy of the MMR vaccine. In fact, research has demonstrated that the various measles vaccines are safe, effective and can be used interchangeably in immunization programs. Natural strains of the virus have never been shown to be transmitted from a vaccinated individual to another. Thanks to an inexpensive and effective vaccine, vaccination with the MMR vaccine constitutes one of the most cost-effective public health interventions in low- and middle-income countries, as elsewhere.[18,19]
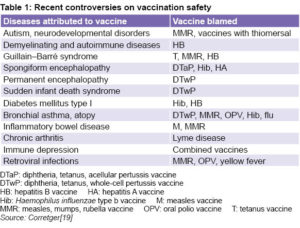
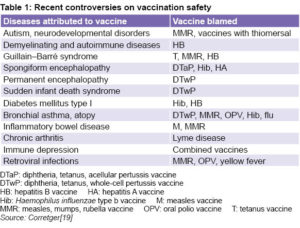
Nevertheless, erroneous associations between vaccine administration and occurrence of different types of diseases now extend to almost all vaccines (Table 1), creating confusion and doubt, and resulting in parental refusal of vaccination for their children. Parents also hesitate to vaccinate their children due to fear of manipulation by the pharmaceutical industry in its eagerness to increase profits, growing interest in natural products for health care and belief in return to a more natural life. They underestimate the true risk of diseases and their consequences, preferring the risk of disease over the “uncertainty” they associate with possible adverse vaccine reactions.[16] Many tout the appeal of freedom of choice as a guiding principle for their actions.[17]
Antivaccination movements on the Internet Antivaxxer ideas have gained followers and spawned an expanded movement now present in many countries. Social media networks have provided its main thoroughfare. Two centuries ago, antivaccination articles in European newspapers and magazines reached an extremely limited readership, but today millions of people visit health pages on the Web.[20]
While provaccination voices grow stronger,[21,22] as does the role of WHO and other global agencies in defense of vaccines,[23] intervention strategies have yet to be effectively implemented at most national levels to stem such a widespread campaign; hence, more vaccination refusals.[24] This movement continues to grow as a consequence of easy access to non–evidence-based claims, spread particularly through the Internet’s social media and other networks, constituting a setback for science and public health progress.[25]
Antivaccine discourse is based on doubts or supposed certainties, arguing that vaccines are ineffective or unsafe, or both. Antivaxxers allege that it is not the vaccines that protect against diseases but rather diseases stop spreading because of improvements in the economy and health. They claim a vaccine can provoke disease because it is made with microbes or “toxic” substances. They dispute the results of vaccine safety studies, hiding or distorting information provided by health authorities. Their arguments allude to parental responsibility to protect children’s health and play on parents’ desire to avoid risks, fomenting distrust in the skills and ethics of professionals who administer vaccines.[6,26]
 Public health authorities and health workers are increasingly concerned about such campaigns’ reliance on digital technology to negatively influence perceptions of vaccines and readiness to accept vaccination. There is no doubt that the threat is growing, as search engines make it easy for people to access antivaccination sites. One study reported that a search for the keyword “vaccination” in seven major search engines (including Google, Yahoo, Netscape, and Lycos) contained antivaccination messages on 43% of sites found.[26]
Public health authorities and health workers are increasingly concerned about such campaigns’ reliance on digital technology to negatively influence perceptions of vaccines and readiness to accept vaccination. There is no doubt that the threat is growing, as search engines make it easy for people to access antivaccination sites. One study reported that a search for the keyword “vaccination” in seven major search engines (including Google, Yahoo, Netscape, and Lycos) contained antivaccination messages on 43% of sites found.[26]
Social media such as Twitter, Facebook and personal blogs enable contact among people and groups with similar ideas through links or suggestions of related content. Many antivaccination groups sponsor their own websites (which both provide “information” and solicit donations) that generate pamphlets and documents that can be downloaded for free or for purchase by their members. Among these are Spain’s “Freedom from Vaccination League,” “Affected by Vaccines,” “Discovery Dsalud,” and “There’s No Pandemic: Stop the Vaccine!” and others. On this side of the Atlantic, there is the Facebook group, “Freedom from Vaccination for a Democratic Chile.”[26] Beyond the Internet, there are groups like “The Refusers,” a musical group that sings antivaccine protest songs (although they deny they are antivaxxer activists, arguing that their songs just promote safe vaccines and freedom of choice).[27]
WHO views antivaccination movements as a growing threat to vaccination programs. In 2019, WHO included a section on vaccine hesitancy in its new five-year strategic plan (WHO 13th General Programme of Work). The WHO Strategic Advisory Group of Experts (SAGE) identified complacency, inconvenience in accessing vaccines, and lack of confidence as main underlying reasons people refuse vaccination for themselves or their children. The group affirmed that health workers (especially in communities) continue to be the most trusted influences on vaccination decisions.[28] WHO’s Global Vaccine Action Plan and SAGE have provided guidance, monitoring indicators and targets for addressing vaccination hesitancy;[23,29] and the Global Vaccine Safety Initiative aims to strengthen national capacities to address the public’s concerns about vaccine safety in a clear, objective, timely manner.[30]
Undoubtedly, today’s public health communication strategies must focus on generating, maintaining or restoring public trust in vaccines and immunization, trust that has been badly damaged by antivaxxer disinformation campaigns on the Internet and beyond. Access to reliable, precise, objective information is essential, for both the public and health professionals,[31] lest public health gains be reversed.
Consequences of reduced global vaccination coverage An emerging health problem in some countries and regions is the occurrence of outbreaks of vaccine-preventable diseases previously considered controlled or eradicated (measles and diphtheria, for example). In 2017, significant measles outbreaks occurred in Europe; most affected were Romania (5560 cases), Italy (5004), Greece (967) and Germany (929).[32] In 2018, the WHO Regional Office for Europe reported 82,596 cases of measles (4 times more than in 2017 and 15 times more than in 2016) and 72 deaths (children and adults). The reasons for this increase vary from country to country. Eastern European health systems did not have the capacity to control the outbreaks or maintain high immunization coverage, while in Western Europe, immunization coverage fell due to distrust in vaccination spread by antivaccination movements.[33,34]
The Americas Region has also experienced outbreaks of vaccine-preventable diseases in recent years. In 2017, PAHO reported that suspected and/or confirmed diphtheria cases appeared in 5 countries: Brazil (39), Colombia (14), Haiti (120), Venezuela (511) and the Dominican Republic (3).[35] In 2018, Colombia, Haiti and Venezuela confirmed cases of diphtheria.[36] In the affected countries, children were unvaccinated.
In the USA in 2019, measles cases reached a 25-year high. From January 1 to April 19, 2019, 626 cases of measles were confirmed in 22 states. This increase is associated with incorrect and scientifically baseless information spread by antivaxxer networks, particularly in states where vaccination is not mandatory. Most children with measles are unvaccinated. Such unvaccinated individuals are the initial locus of an outbreak that can lead to an epidemic.[37,38] Adding inadequate immunization coverage or failure to complete the immunization schedule (due to health system organizational problems) to the effects of antivaxxer movements, the Americas Region can expect a worsening epidemiological profile for vaccine-preventable diseases.
Around the world, parents’ refusal to vaccinate their children is addressed in different ways. In Spain, the Spanish Pediatrics Association’s Advisory Committee on Vaccines, together with its Bioethics Committee, determined it was not advisable to obligate parents to vaccinate their children, but parents should be required to sign a vaccine refusal document, in which they acknowledge having received information about vaccination, its importance and benefits, and risks to unvaccinated children.[39,40] Others hold that courts should oblige parents to vaccinate their children, based on WHO guidelines.[41]
New York City’s mayor declared a public health emergency in April 2019, obligating vaccination in selected neighborhoods where measles outbreaks had occurred,[42] and new legislation in the state has removed school vaccination exemptions for philosophical reasons (permitting only medical exemptions). US medical authorities have asked social networks and popular search engines to censor false information circulating about vaccines, given the threat that antivaccination groups represent in a country where 15 out of 50 states allow philosophical exemptions from school vaccinations.[43]
Antivaccination movements’ challenges for Cuba Since creation of the National Immunization Program (PNI) in 1962, vaccinations are included in primary health care (PHC): against diphtheria, tetanus and pertussis (DTP vaccine), polio (oral polio vaccine, OPV), and the severe forms of tuberculosis (BCG vaccine); and later against other diseases such as hepatitis B, viral meningitis, and Hib.[44,45] Explaining the balance and scale of risk in the risk–benefit equation allows the public to weigh the importance of immunization for individual and community health. Since its beginnings, PNI’s vaccination activities rely on four basic principles: the entire population is targeted; activities are integrated into PHC; they depend on active community participation; and all vaccinations are free of charge.[45]
Since 1999, all Cubans are protected against 13 diseases, previously potentially fatal or disabling. Thanks to biotech development, 8 of the vaccines are manufactured in Cuba; imported vaccines are BCG, MMR and OPV.[45]
Cuba is one of the countries that does not have a recognized antivaccination movement and, in general, PAHO and other expert evaluations have found that parents are both aware of and anxious to vaccinate their children.[45] In 2015, a study in a primary care unit exploring health culture and vaccination in families of children aged <2 years found that vaccination was highly valued. Participants considered vaccinations important, had confidence in PNI, and were satisfied with health service organization and their care from healthcare providers. Mothers considered vaccinating their children a responsibility, part of protecting their children’s health. In addition, they observed coherence in messages from PNI, traditional mass media and social networks, describing information from these media as science based.[46]
Cuba’s vaccine-related adverse events surveillance system One of the main arguments in antivaxxer discourse is lack of vaccine safety, so an important complement to information on the benefits of PNI, which ensures safety and reliability, is the vaccine-related adverse events surveillance system instituted in Cuba in 1999.
Surveillance of vaccine-preventable diseases was adapted to the Cuban context from WHO guidelines for effective management of its Expanded Program on Immunization (EPI). Surveillance performs the basic functions of gathering, analyzing and evaluating information on vaccine quality, efficacy and safety.[47]
Surveillance of vaccine-related adverse events is conducted at the primary care level, family physicians mainly responsible. Ongoing training of health personnel at all levels in the health system in surveillance of possible adverse effects enables decision-making in case management, event management, notification and timely investigation of severe events, all of which contribute to PNI’s credibility and success.[47] In addition, health professionals who are knowledgeable about the realities of adverse events help to prevent rumors that could provoke vaccination refusal in their communities.
Cubans’ increasing access to social media and the Internet in general as a result of expansion of services[48] places the public in contact with information posted on antivaccination groups’ websites, blogs and profiles. Although Cuban citizens are well educated, trust health professionals and are satisfied with PNI, [44] the risk of unscientific influences remains. At this writing, there is no specific strategy to respond to the threat, but we believe it is possible to keep Cuba’s high immunization coverage from falling and avoid outbreaks of vaccine-preventable diseases if there is continuing effective communication on vaccination, particularly in PHC, where physicians and nurses mingle with families and neighborhoods.
Cuba’s public health system, based as it is in PHC, is ideally suited for health professionals to organize educational programs in their communities, enabling residents to critically assess information disseminated by antivaccination sites, building on knowledge of scientific results about the benefits of vaccination in Cuba and the world, where diseases have been controlled, eradicated or kept from becoming public health problems. Important messages to convey include how systematic vaccination with high coverage prevents death and disability of millions of children annually, and that data from the vaccine-related adverse events surveillance system supports that there is low risk associated with vaccination.
Communication should be a continuous process that enables professionals to properly explain vaccine benefits and risks, address the public’s concerns, tackle incipient or persistent rumors about vaccine safety, and prepare responses to any crises regarding vaccine safety that might occur. Such efforts would help prevent dissemination of messages questioning vaccination safety with no scientific basis.
In addition, Cuban health professionals and medical institutions should take advantage of the presence of the 6.47 million Cubans on Internet (56% of the population) to post messages related to results of vaccination drives and the immunity achieved throughout the country. The rates of connectivity continue to climb, with Facebook the most frequently used social media (59.3% of Internet users) in 2018.[49]
CONCLUSIONS
Vaccination is the most effective preventive health intervention, after clean water, in terms of cost–benefit balance in control of communicable diseases. But the growing refusal of parents to vaccinate their children as a result of misinformation spread on the Internet by antivaccination groups puts global public health in danger of outbreaks of diseases such as measles and diphtheria.
High immunization coverage (≥99%) has been achieved in Cuba with the 11 vaccines (against 13 diseases) administered in the national vaccination program, and there are no reports of vaccination refusal.[50] There is public trust in the program and satisfaction with its implementation: Cuban parents consider child vaccination to be a personal and social responsibility.
While this is the situation now, we cannot ignore the danger posed by antivaxxer messages. Cubans have steadily growing access to the Internet, both to scientific information and to misinformation, so effective education and communications strategies are needed for health professionals and the public they serve, to maintain gains in control of infectious diseases.
References

- World Health Organization; United Nations Children’s Fund (UNICEF); World Bank. State of the World’s Vaccines and Immunization. 3rd ed [Internet]. Geneva: World Health Organization; 2009 [cited 2019 Jan 8]. 185 p. Available from: http://whqlibdoc.who.int/publications/2010/9789243563862_spa.pdf
- Cortés García M, Pereira J, Peña-Rey I, Génova R, Amela C. Carga de enfermedad atribuible a las afecciones inmunoprevenibles en la población infanto-juvenil española. Gac Sanit [Internet]. 2004 [cited 2010 Nov 23];18(4):312–20. Available from: http://scielo.isciii.es/pdf/gs/v18n4/original7.pdf. Spanish.
- Bagán J, Fernández G. El valor social de las vacunas: Elementos de reflexión para facilitar el acceso. London: Deloitte Touche Tohmatsu Limited (DTTL); 2015 Apr. Chapter 2. p. 11. Spanish.
- Andrus JK, Bandyopadhyay AS, Danovaro MC, Dietz V, Domingues C, Figueroa JP, et al. The past, present, and future of immunization in the Americas. Rev Panam Salud Pública [Internet]. 2017 [cited 2018 Nov 23];41:e121. Available from: https://doi.org/10.26633/RPSP.2017.121. Spanish.
- Martínez Romero M, Martínez Diz S, García Iglesias F. ¿Por qué los padres no vacunan a sus hijos? Reflexiones tras un brote de sarampión en un barrio de Granada. Anales Pediatr [Internet]. 2011 Sep [cited 2018 Oct 24];75(3):209–10. Available from: http://www.analesdepediatria.org/es/por-que-los-padres-no/articulo/S1695403311002542/. Spanish.
- Zúñiga Carrasco IR, Caro Lozano J. Grupos antivacunas: el regreso global de las enferme dades prevenibles. Rev Latinoam Infect Pediatr [Internet]. 2018 Jan–Mar [cited 2018 Nov 23];31(1):17–21. Available from: https://www.medigraphic.com/pdfs/infectologia/lip-2018/lip181d.pdf. Spanish.
- World Health Organization [Internet]. Geneva: World Health Organization; c2019. Preguntas y respuesta sobre la inmunización y seguridad de las vacunas; 2016 Mar 24 [updated 2018 Apr; cited 2018 Nov 23]. Available from: http://www.who.int/features/qa/84/es. Spanish.
- World Health Organization; United Nations Children’s Fund; World Bank. State of the world’s vaccines and immunization. 3rd ed. Geneva: World Health Organization; 2009.
- Pan American Health Organization; World Health Organization. Vacunación Segura. Vigilancia de los eventos supuestamente atribuidos a la vacunación o inmunización de la vacuna contra la gripe A (H1N1) y prevención de crisis. Washington, D.C.: Pan American Health Organization; 2009 Oct. p. 4. Spanish.
- Ortigosa L. ¿Por qué están reemergiendo en Canarias brotes de enfermedades prevenibles por vacunas? Canarias Pediátr [Internet]. 2012 May–Aug [cited 2018 Nov 23];37(2):77–82. Available from: http://portal.scptfe.com/wp-content/uploads/2013/12/2012-2-1.d.pdf. Spanish.
- The History of Vaccines [Internet]. Philadelphia: College of Physicians of Philadelphia, Educational Resource; c2019. Historia de los movimientos antivacunas; [updated 2018 Jan 10; cited 2019 May 16]. Available from: https://www.historyofvaccines.org/index.php/es/contenido/articulos/historia-de-los-movimientos-en-contra-de-la-vacunaci%C3%B3n#close. Spanish.
- Wakefield A, Murch SH, Anthony A, Linnell J, Casson DM, Malik M, et al. Ileal-lymphoid-nodular hyperplasia, non specific colitis, and pervasive developmental disorder in children. Lancet. 1998 Feb 28;351(9103):637–41.
- Wakefield A, Murch SH, Anthony A, Linnell J, Casson DM, Malik M, et al. Ileal-lymphoid-nodular hyperplasia, non-specific colitis, and pervasive developmental disorder in children. Lancet. 2010 Feb 6;375(9713):445. Retraction of: Wakefield A, Murch SH, Anthony A, Linnell J, Casson DM, Malik M, et al. Ileal-lymphoid-nodular hyperplasia, non-specific colitis, and pervasive developmental disorder in children. Lancet. 1998 Feb 28;351(9103):637–41.
- Deer B. How the case against the MMR vaccine was fixed. BMJ [Internet]. 2011 Jan 5 [cited 2019 May 16];342:c5347. Available from: https://doi.org/10.1136/bmj.c5347
- López MA. Los movimientos antivacunación y su presencia en Internet. Santa Cruz de la Palma [Internet]. 2015 Jan [cited 2019 Aug 29];9(3). Available from: http://scielo.isciii.es/scielo.php?script=sci_arttext&pid=S1988-348X2015000300011&lng=es. Spanish.
- Siddiqui M, Salmon DA, Omer SB. Epidemiology of vaccine hesitancy in the United States. Hum Vaccin Immunother [Internet]. 2013 Dec 1 [cited 2019 Sep 2];9(12):2643–8. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4162046/
- Trilla A. Vacunación sistemática: convencidos, indecisos y radicales. Med Clin (Barc) [Internet]. 2015 [cited 2019 Sep 2];145(4):160–2. Available from: http://www.migueljara.com/wp-content/uploads/2015/08/vacunas-Trilla-Med-Clin-2015.pdf
- Strebel PM. Measles vaccine. In: Plotkin S, Orenstein W, Offit P, editors. Vaccines. 5th ed. Philadelphia: Saunders Elsevier; 2008. p. 352–98.
- Corretger JM, Hernández MT. Controversias de interés sobre la seguridad de las vacunas en niños. In: de Aristeguí Fernández J, editor. Vacunaciones en el niño: de la teoría a la práctica.
- Manual adaptado para los profesionales sanitarios de Andalucía. Sevilla: Junta de Andalucía, Consejería de Salud; 2006. p. 128–43.
- Wolfe RM, Sharp LK. Anti-vaccinationists past and present. BMJ [Internet]. 2002 Aug 24 [cited 2019 May 16];325(7361):430–2. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1123944/
- Hotez PJ. Vaccines Did Not Cause My Daughter´s Autism. The Scientist [Internet]. 2018 Nov 1 [cited 2019 Sep 8] Available from: at https://www.the-scientist.com/reading-frames/vaccines-did-not-cause-my-daughters-autism-64946
- Balakrishnan VS. A crusade against the anti-vaccination movement. Lancet Infect Dis [Internet]. 2019 Apr 1 [cited 2019 May 16];19(4):368. Available from: https://www.thelancet.com/journals/laninf/article/PIIS1473-3099(19)30101-X/fulltext
- World Health Organization, Department of Immunization. Global Vaccine Action Plan. Monitoring, Evaluation & Accountability. Secretariat Annual Report 2018. Geneva: World Health Organization; 2018. 138 p.
- Sadaf A, Richards JL, Glanz J, Salmon DA, Omer SB. A systematic review of interventions for reducing parental vaccine refusal and vaccine hesitancy. Vaccine. 2013 Sep 13;31(40):4293–304.
- Hussain A, Ali S, Ahmed M, Hussain S. Cureus. The Anti-vaccination Movement: a regression in modern medicine. Cureus [Internet]. 2018 Jul 3 [cited 2019 Aug 27];10(7):e2919. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6122668/
- Davies P, Chapman S, Leask J. Antivaccination activists on the World Wide Web. Arch Dis Child [Internet]. 2002 Jul [cited 2018 Oct 24];87(1):22–5. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1751143/
- The antivaccine bands The Refusers Back from the dead [Internet]. [place unknown]: Respectful Insolence; c2004–2019; [updated 2011 Jun 9; cited 2019 Sep 2]. Available from: https://respectfulinsolence.com/2011/06/09/the-annals-of-im-not-anti-vaccine-part-8-1/
- World Health Organization [Internet]. Geneva: World Health Organization; c2019. Emergencias sanitarias. Diez cuestiones de salud que la OMS abordará este año; 2019 [cited 2019 Apr 25]. Available from: https://www.who.int/es/emergencies/ten-threats-to-global-health-in-2019. Spanish.
- World Health Organization. Vaccine hesitance. In: SAGE Meeting Report [Internet]. Geneva: World Health Organization; 2014 Oct [cited 2019 Sep 8]. Available from: http://apps.who.int/immunization/sage/search_topics/meetings/32?search=vaccination+hesitancy
- World Health Organization [Internet]. Geneva: World Health Organization; 2019. Iniciativa global sobre la seguridad de las vacunas. Comunicación sobre la seguridad de las vacunas; [updated 2014 Apr 15; cited 2018 Nov 23]. Available from: http://www.who.int/vaccine_safety/initiative/communication/es/. Spanish.
- Biblioteca del Congreso Nacional de Chile [Internet]. Santiago de Chile: Biblioteca Nacional del Congreso Nacional de Chile; c2019. Noticias. Inmunización y salud pública: la importancia de una buena información. 2018 Apr 18 [cited 2019 Apr 25]; [about 4 screens]. Available from: https://www.bcn.cl/observatorio/bioetica/noticias/vacunas. Spanish.
- European Centre for Disease Prevention and Control. Measles and rubella monitoring, January 2017-Disease surveillance data: 1 January 2016-31 December 2016 [Internet]. Stockholm: European Centre for Disease Prevention and Control (ECDC); 2017 Jan [cited 2019 Apr 25]. 16 p. Available from: https://ecdc.europa.eu/sites/portal/files/documents/measles%20-rubella-monitoring-170424.pdf
- Plaza JA. Diario Médico. Informe de la OMS. Sarampión en Europa. Más vacunados que nunca pero también record de casos [Internet]. 2019 Feb 7 [cited 2019 Apr 24]. Available from: https://www.diariomedico.com/salud/sarampion-en-europa-mas-vacunados-que-nunca-pero-tambien-record-de-casos.html. Spanish.
- Pan American Health Organization [Internet]. Washington, D.C.: Pan American Health Organization;c2019. Gestión y difusión de la información. Alertas epidemiológicas; 2019 [cited 2019 Apr 25]. Available from: https://www.paho.org/hq/index.php?option=com_content&view=featured&Itemid=2291&lang=es. Spanish.
- Tabakman R. Alerta por nuevos casos de difteria en Sudamérica: ¿El regreso de Corynebacterium? Medscape [Internet]. 2017 Dec 12 [cited 2019 Aug 28];Noticias y perspectivas. Available from: https://espanol.medscape.com/verarticulo/5902171. Spanish.
- Asociación Española de Pediatría [Internet]. Madrid: Asociación Española de Pediatría; c2019. Noticias sobre vacunas. La difteria persiste en algunos países americanos; 2018 Sep 3 [cited 2019 Aug 27]; [about 3 screens]. Available from: https://vacunasaep.org/profesionales/noticias/la-difteria-persiste-en-algunos-paises-americanos. Spanish.
- Center for Disease Control and Prevention (CDC) [Internet]. Atlanta: Center for disease Control and Prevention (CDC); c2019. Measles Home. Cases and Outbreaks. Casos y brotes de sarampión en el 2019; [updated 2019 Aug 30; cited 2019 Apr 25]. Available from: https://www.cdc.gov/measles/cases-outbreaks-sp.html. Spanish.
- Measles Is Making a Comeback. Here’s How to Stop It. The New York Times [Internet]. 2019 Mar 11 [cited 2019 Aug 28];Opinion:[about 4 screens]. Available from: https://www.nytimes.com/2019/03/11/opinion/measles-outbreak-vaccines.html
- Asociación Española de Pediatría [Internet]. Madrid: Asociación Española de Pediatría; c2019. Documentos. Rechazo de la vacunación: documento de declaración de responsabilidad de los padres; 2015 Jul 9 [cited 2019 Aug 28]. Available from: https://vacunasaep.org/documentos/documento-de-rechazo-de-la-vacunacion. Spanish.
- García N. Padres que no quieren vacunar: documento de negación de vacunación [Internet]. Zaragoza: Centro de Salud Delicias Sur, CAV-AEP; [cited 2019 Aug 28]. Available from: https://docplayer.es/7198349-Padres-que-no-quieren-vacunar-documento-de-negacion-de-vacunacion-nuria-garcia-sanchez-centro-de-salud-delicias-sur-zaragoza.html. Spanish.
- Vizoso S. La justicia obliga a una madre a vacunar a sus hijos tras la demanda del padre. El País [Internet]. 2019 Aug 27 [cited 2019 Aug 27]; Vacunación:[about 3 screens]. Available from: https://elpais.com/sociedad/2019/08/27/actualidad/1566918743_373335.html. Spanish.
- Pager T, Mays JC. New York Declares Measles Emergency, Requiring Vaccinations in Parts of Brooklyn. The New York Times [Internet]. 2019 Apr 9 [cited 2019 Sep 8]; [about 5 screens]. Available from: https://www.nytimes.com/2019/04/09/nyregion/measles-vaccination-williamsburg.html
- Michelle A. As Measles Outbreak Fades, N.Y. Sets In Motion New Rules On School Vaccinations. Kaiser Health News [Internet]. 2019 Sep 5 [cited 2019 Sep 8]; [about 3 screens]. Available from: https://khn.org/news/as-measles-outbreak-fades-n-y-sets-in-motion-new-rules-on-school-vaccinations/
- López Ambrón L, Egües Torres LI, Pérez Carreras A, Galindo Santana BM, Galindo Sardiña MA, Resik Aguirre S, et al. Experiencia cubana en inmunización, 1962–2016. Rev Panam Salud Pública [Internet]. 2018 [cited 2019 Aug 28];42:e34. Available from: https://doi.org/10.26633/RPSP.2018.34. Spanish.
- Reed G, Galindo MA. Cuba’s National Immunization Program. 2007. MEDICC Rev. 2007 Oct;9(1):5–7.
- Ávila Y. La cultura de la salud y el acto de vacunar en familiares de niños/as menores de dos años. Policlínico “5 de septiembre”, municipio Playa. 2015 [thesis]. [Havana]: “5 de septiembre” Teaching Polyclinic; 2015.
- Galindo Belkys M, Concepción D, Galindo MA, Pérez A, Saiz J. Vaccine-related adverse events in Cuban children, 1999–2008. MEDICC Rev. 2012 Jan;14(1):38–43.
- Puig Y. El proceso de informatización de la sociedad cubana es un hecho. Granma [Internet]. 2019 Feb 18 [cited 2019 Aug 27]. Available from: http://www.granma.cu/cuba/2019-02-18/el-proceso-de-informatizacion-de-la-sociedad-cubana-es-un-hecho-18-02-2019-22-02-12. Spanish.
- Alonso-Falcón R. Informe Global Digital 2019: Cuba entre los países que más crecen en usuarios de internet y redes sociales. Cubadebate [Internet]. 2019 Feb 13 [cited 2019 Sep 8]; [about 4 screens]. Available from: http://www.cubadebate.cu/especiales/2019/02/13/informe-global-digital-2019-cuba-entre-los-paises-que-mas-crecen-en-usuarios-de-internet-y-redes-sociales/#.XXPx-XspDIU. Spanish.
- National Statistics Bureau (CU). Anuario Demográfico de Cuba 2018 [Internet]. Havana: National Statistics Bureau (CU); 2019 Jun [cited 2019 Jul 7]. 143 p. Available from: http://www.onei.cu/anuariodemografi co2018.htm. Spanish.
THE AUTHORS
Belkys María Galindo-Santana (Corresponding author: bgalindo@ipk.sld.cu), physician with dual specialties in family medicine and epidemiology, with a master’s degree in epidemiology and doctorate in medical sciences. Full professor and senior researcher, Pedro Kourí Tropical Medicine Institute (IPK), Havana, Cuba.
Elba Cruz-Rodríguez, physician with dual specialties in family medicine, and public health & epidemiology. Assistant professor, IPK, Havana, Cuba.
Lena López-Ambrón, baccalaureate nurse specializing in public health & epidemiology, with a master’s degree in infectious diseases. Ministry of Public Health, Havana, Cuba.
Submitted: January 04, 2019 Approved: September 06, 2019 Disclosures: Lena López-Ambrón heads Cuba's National Immunization Program