INTRODUCTION
In recent decades, few diseases have caused as severe an impact in the world as AIDS. This condition, caused by the human immunodeficiency virus (HIV), undoubtedly was the most important infectious pandemic in the second half of the 20th century and continues to be an important global public health priority.[1]
An estimated 34 million people in the world were living with HIV in 2011, 30 years into the epidemic.[1,2] Globally, women make up 50% of those living with HIV, but in regions such as sub-Saharan Africa, the proportion can be as high as 59%. The Joint United Nations Program on HIV/AIDS (UNAIDS) released alarming data for 2011: an estimated 1.2 million women contracted HIV that year, over one million more than in 2001.[1] According to the same source, HIV infection rates in women aged 15–24 years were double that of men the same age.[1,2]
In Latin America, >36% of those infected with HIV are women, but in the Caribbean, >50% are women.[2,3] Although the epidemic in the Caribbean is concentrated in men who have sex with men (MSM), research has found that 22% of MSM reported also having sex with women, which increases risk of heterosexual HIV transmission.[2]
The increasing figures for women infected with HIV highlights their vulnerability, due to a combination of biological factors and gender inequality.[4–6] Biologically, women are more likely than men to be infected during heterosexual sex, because a larger mucosal surface is exposed and there is greater concentration of virus in semen, which remains in the vagina for a longer time. Socially, because of cultural norms in “machista” societies, women are often economically, socially and emotionally dependent on men, making it difficult for them to negotiate protected sex. Often, women have sex only with their stable partner and in these conditions the woman’s vulnerability to contracting HIV tends to be the result of her partner’s behavior (bisexuality, injectable drug use, unprotected sex with several partners) rather than her own.[7–9]
The political, economic and social transformations that began in Cuba in 1959 have benefited women’s equality.[10] Nevertheless, women still suffer the consequences of patriarchal patterns established centuries ago, which are reflected in aspects of daily life such as disparities in burden of housework, responsibility for children and role distribution in couples’ relationships.[11,12]
In 1986, Cuba diagnosed its first HIV case and also began its National HIV/AIDS Prevention and Control Program.[13] In the beginning, the Program focused on active case-finding in groups considered at risk at the time, including Cubans who had worked overseas and returned to the country, institutionalized persons and those diagnosed with other sexually transmitted infections (STI).
Screening of all pregnant women was also indicated as a first step in decreasing vertical transmission.[14] In 1995, Cuba began to produce its own diagnostic reagents, which enabled expansion of screening to other population groups at all levels of the country’s health care system.
The Cuban program includes other important components:
- Prevention, through educational programs aimed at the general population, but especially targeting vulnerable groups such as MSM and young people; counseling services; training of youth counselors and volunteers; peer training; and free or very low-cost condom distribution. All this work is done in close coordination with other national agencies, including the Ministry of Culture, the National Sex Education Center (CENESEX, the Spanish acronym) and the Federation of Cuban Women (FMC, the Spanish acronym).[15–18]
- Strict screening of all donated blood and blood products, which has eliminated HIV transmission from this source in Cuba.
- Prevention of vertical transmission of HIV, which includes routine HIV testing of pregnant women during the first and third trimesters; preconception counseling for women with HIV; provision of antiretroviral drugs starting in the fourteenth week of pregnancy; planned cesareans for pregnant women with HIV; and a recommendation against breastfeeding accompanied by provision of breast milk substitutes for infants. For all babies born to HIV+ mothers, a dried blood spot sample is taken at 15 days of age and PCR tested for viral DNA using; treatment with zidovudine is begun two hours after birth and continued for six weeks; and serological monitoring is done through 18 months of age.[14]
- Comprehensive care of persons with HIV, which includes no-cost access to nationally produced generic antiretroviral drugs, psychological and nutrition services, support for social integration and legal protection.[13–19]
In Cuba, the HIV/AIDS epidemic began slowly, but overall incidence has been increasing since the late 1990s, from 23.2 per million population in 2000 to 50.1 in 2010, by the end of which a total of 12,217 cases of HIV had been diagnosed.[20] Of those infected with HIV, 80.6% are men and 19.4% are women.[21]
Women account for 25.7% of HIV infections in the group aged 15–24 years and 20.8% of those aged 24–35 years.
Another characteristic of the HIV epidemic in Cuba is that the majority of infected persons live in urban areas and over half (51.2%) in Havana.[21,22] In 2011, it was reported that 43.6% of HIV+ Cuban women were living in Havana.[12,21,22] The authors of this article work with people with HIV/AIDS from different Havana municipalities and have directly observed a growing number of HIV infections in women; hence our interest in this study to describe HIV patterns among women in Havana Province during the 26 years of the Cuban epidemic.
METHODS
Cuba’s capital, Havana, is located in western Cuba; it has provincial status and, until the end of 2009, was known as City of Havana Province. It covers 728.26 km2, divided into 15 municipalities. Its mean population in 2011 was 2,130,431, with a population density of 2925.4 inhabitants per km2.[20]
Type of study and subjects This was a descriptive study, based on surveillance data, of women (aged >14 years) resident in Havana diagnosed with HIV from 1 January 1986 (the year in which the first case was diagnosed) through 31 December 2011. All reported cases were studied—a total of 1274. Havana was chosen because it was the only province for which we had access to case information.
Data source Information was obtained from the limited-access HIV/AIDS database of Cuba’s Ministry of Public Health (MINSAP, the Spanish acronym).
Variables The following variables were used:
Age at diagnosis Subjects were classified by age at diagnosis (age groups in years): 15–19, 20–29, 30–39, 40–49, 50–59, ≥60.
Education Level of education completed: illiterate (did not complete primary school); primary school (6th grade completed); middle school (9th grade completed); high school (preuniversity or middle-level technical studies completed); university (higher education completed).
Screening group Active screening for HIV infection is done in several population groups and at all levels of Cuba’s health system, as part of the National STI/HIV/AIDS Prevention and Control Program.
Screening groups are classified for HIV testing as follows:
- Provider-identified—individual who does not belong to any predefined risk group but is assessed by physician as being at risk because of sexual and/or social behavior and an HIV test is indicated
- Contact—individual who is a contact of a person with HIV or AIDS
- Donor—individual tested in order to donate blood
- Emigrant—individual applying for departure to countries that require HIV testing to issue an entry visa
- Self-identified—individual who personally requests HIV test at a health service
- STI—individual diagnosed with an STI, such as syphilis, gonorrhea, condyloma acuminata, herpes simplex, chlamydia, trichomoniasis, hepatitis B or C, or bacterial vaginosis
- Pregnant—prenatal HIV test indicated
- Hospital patient—tested while an inpatient
- Nephrology—individual with chronic renal insufficiency in dialysis
- Other—institutionalized persons, tuberculosis patients, anonymous testing, hemophiliacs, organ or tissue donors, foreign residents in Cuba.[13]
Municipality of residence at diagnosis The woman’s place of residence when she was diagnosed. The 15 municipalities included were: 10 de Octubre, Arroyo Naranjo, Boyeros, Central Havana, Cerro, Old Havana, Playa, Plaza, Marianao, La Lisa, Cotorro, San Miguel del Padrón, Regla, Guanabacoa, and East Havana. These municipalities belonged to City of Havana Province through 2009, after which the name became simply Havana, although it retained its status as a province with all 15 municipalities.
Year of diagnosis Year patient was diagnosed, 1986–2011.
Year of AIDS diagnosis Year in which patient first developed an AIDS-defining condition or first had a CD4 T-lymphocyte count <200 per mm3.
AIDS-defining condition The US Centers for Disease Control and Prevention (CDC) 2008 classification was used: wasting syndrome (unintended loss of >10% of usual weight, plus fever and diarrhea for >30 days, not attributable to other causes), pulmonary tuberculosis, Pneumocystis jirovecii pneumonia, neurotoxoplasmosis, and others (invasive cervical cancer, esophageal candidiasis, cerebral cryptococcosis, cryptosporidiosis, disseminated cytomegalovirus infection, isosporiasis, histoplasmosis, Kaposi sarcoma, non-Hodgkin lymphoma). The AIDS definition includes patients without an AIDS-defining condition but a with CD4 T-lymphocyte count <200 per mm3.[23]
Late presentation/late diagnosis of HIV Defined as initial HIV diagnosis coinciding with AIDS onset, i.e., an AIDS-defining condition or a CD4 T-lymphocyte count <200 per mm3 at time of HIV diagnosis or within one year of HIV diagnosis.
Vital status at close of study period Whether the person was alive or deceased at the end of 2011.
Year of death Year patient died, 1986–2011.
Data analysis Data were entered into an Excel database and analyzed using SPSS 13.0 statistical software. Statistical analysis was based on absolute and relative frequency distributions. The following were calculated:
- cumulative HIV incidence (number of new HIV cases over mean female population in the year in question per million population) for each year of diagnosis;
- AIDS case incidence (number of new AIDS cases over mean female population for the year in question per million population) for each year;
- cumulative HIV/AIDS incidence by municipality of residence (total number of new HIV/AIDS cases in municipality over mean female population in the municipality for the entire study period, per 10,000 population); and
- case fatality rates (number of AIDS deaths over number of HIV/AIDS cases—excluding patients with unknown status at end of 2011—per 100 prevalent cases) for each year of diagnosis.
- Analysis of late presentation was done by five-year periods.
Results were displayed in tables and figures.
Research ethics MINSAP authorization was obtained for access to its HIV/AIDS database. Patient names were stripped from data entries, leaving only case numbers. Data were used solely for research purposes. The study was approved by the Enrique Cabrera General Teaching Hospital research ethics committee.
RESULTS
Younger age groups were the most affected by HIV: 38% were aged 20–29 years and 25.2% aged 30–39 years. Cumulatively, 75.8% of HIV cases were aged ≤39 years. Frequency of women diagnosed aged ≥50 years was low (Table 1).
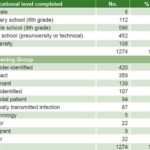
Educationally, the largest group had completed middle school (46.8%), followed by high school (35.4%); 8.5% of the women had a college education, and high school and college graduates together accounted for 43.9%. The 6 (0.5% of 1274) persons who were illiterate had been diagnosed with developmental delays, two moderate and four mild (Table 2).
Table 1: HIV cases in women by age at diagnosis, Havana, 1986–2011

Table 2: HIV cases in women by educational level and screening group, Havana, 1986–2011
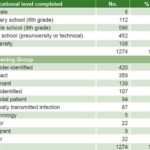
The main screening groups were provider-identified (33%) and contact groups (28.2%); 10.9% were diagnosed during prenatal screening (Table 2).
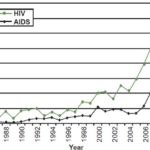
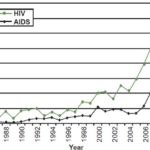
HIV incidence in 2011 more than tripled from 2001 (increasing from 41.7 per million population in 2001 to 151.7). The AIDS case-rate began to increase significantly in 2006, when it almost doubled from the preceding year (from 13.1 cases per million population in 2005 to 22.8 in 2006). Although both rates have increased, the AIDS case-rate did not rise as fast as HIV incidence (Figure 1).
Figure 1: HIV and AIDS incidence in women, Havana, 1986–2011
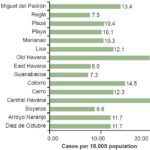
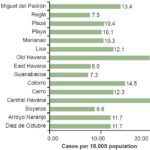
Central Havana and Old Havana municipalities had the highest cumulative incidence (19.4 and 19.2 per 10,000 population respectively), while Guanabacoa had the lowest (7.3 per 10,000 population) (Figure 2).
In total, 488 women were diagnosed with AIDS (38.3%) during the study period. The most frequent AIDS-defining conditions were wasting syndrome (14.8%) and Pneumocystis jirovecii pneumonia (7.4%). Other conditions that occurred less frequently were invasive cervical cancer (1), esophageal candidiasis (4), disseminated cytomegalovirus infection (3), cerebral cryptococcosis (7), cryptosporidiosis (8), histoplasmosis (3), non-Hodgkin lymphoma (5), and Kaposi sarcoma (4). No clinical disease was present in 58.2% of diagnosed AIDS cases (Table 3).
Figure 2: Cumulative HIV incidence in women by municipality, Havana, 1986–2011
Late presentation or diagnosis of the disease occurred in 94 individuals (7.4% of persons with HIV and 19.3% of AIDS cases), with a mean age of 38.9 years. By the end of 2011, 167 women with AIDS had died, 158 (94.6 %) of AIDS-related causes and 9 (5.4%) of other causes (two from automobile accidents, three from chronic renal failure due to pre-existing kidney disease, one severe bronchial asthma attack, one pulmonary thromboembolism, one case of mycosis fungoides, and one suicide).
Table 3: AIDS cases in women by AIDS-defining condition, Havana, 1986–2011

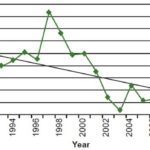
Figure 3: AIDS case fatality trend in women, Havana, 1990–2011
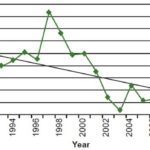
Case fatality rates began to decline in 1998 and have remained stable at approximately 1% since 2006 (Figure 3).
DISCUSSION
This study found that the most frequent ages at diagnosis were 20–39 years, in contrast to the global situation: 22% of new HIV infections in women worldwide occur in those aged 15–24 years.[1,2] An HIV study in Latin American countries found the highest percentages of adult women aged >24 years living with HIV/AIDS in the Dominican Republic (56.1%), Argentina (32.7%) and El Salvador (32.4%).[24]
A 2011 study of persons with HIV/AIDS in Cuba,[21] found that 64.2% were aged 25–44 years. Most of the men were in that group (63.7%), while women, in contrast, were more concentrated in the group aged 20–39 years (66.6%), similar to our findings. This is only to be expected given that women in Havana account for close to half the HIV infections among women in Cuba. An HIV prevention study found that only 11% of women used condoms, the percentage lower in adult women (aged >15 years) than in men.[25]
The main cause of contagion according to persons living with AIDS was “having sex without a condom,” followed by “trusting one’s partner,” which half of the women mentioned.[21] According to the Survey on Indicators for HIV Infection Prevention in 2011, one third of the Cuban population aged 15–49 years said they had low risk perception, which corroborates the importance of continuing to address this contributing factor to HIV infection in women.[26,27]
With regard to educational level, the greatest proportion of women living with HIV in this study had completed middle school. The Cuban population has a high educational level[28] because education is compulsory through ninth grade, and persons with HIV are no exception. Of persons living with HIV, 62.1% have completed high school or college.[21] However, it has been reported that, unlike the overall Cuban population, among those with HIV, women are relatively less educated than men.[29] This was seen in Havana women, where the largest group had a middle-level education.
Education is a proxy for population vulnerability to HIV. Papers from Venezuela and Chile show that low educational level is associated with insufficient knowledge about HIV.[30,31] Educational level has been associated with knowledge about prevention methods, the probability of actually using these methods during sexual relations, and to a certain extent with perception of risk of contracting HIV.
However, in reality, educational and knowledge levels do not always correlate with appropriate risk perception; and this is coupled with a division of domestic roles that assigns less decision-making power to women, and the role of “sexual expert” to men. All this influences Cuban women’s reluctance to demand condom use during sex.[12]
The greatest number of cases were provider identified or contacts of other HIV+ people, similar to other Cuban findings.[22] This fact highlights the importance of HIV diagnostic work by doctors and nurses, above all in primary health care; doubly so because these two screening groups are generally asymptomatic.
HIV incidence in the female population in our study is continuing to rise, along with general incidence in Cuba, a fact that has been observed in other studies.[22,32] We believe that several factors are involved in this trend, some already mentioned, such as a somewhat lower educational level and the trend toward older ages; both factors associated with low risk perception. Added to this is the effect of increased active screening in Cuba.
AIDS case rates increased much more slowly than HIV rates. Many factors are known to be involved in the progression from HIV to AIDS, including pre-existing health conditions, nutritional status, psychological factors, individual lifestyle, associated comorbidities, antiretroviral therapy (ART) and adherence, among others. Many of these factors can be managed or modified and they are addressed in Cuba’s comprehensive care program for persons living with HIV/AIDS, which offers a course, Learning to Live with HIV/AIDS, for individuals newly diagnosed.[15]
The higher incidence our study found in Old Havana and Central Havana municipalities coincide with other studies conducted in Cuba.[33,34] These two municipalities are adjacent; both are densely populated and are important tourism districts. Additionally, both have marginalized neighborhoods and areas of widespread antisocial behavior (illegal drug sales and use, gambling) and so-called sitios de encuentro, or hook-up sites, of illegal sex trade.
Women who live in these areas are not immune to the influence of these negative factors on their sexual behavior, since it is precisely marginalized conditions that are conducive to risky sexual behaviors, such as a high number of partners, unprotected sex under the influence of drugs or alcohol, or sex involving violence.[11,12]
Wasting syndrome, a condition initially called “slim disease” in African communities, is the clinical event reported most frequently as a marker of AIDS[35] and was also observed in this study. Opportunistic infections do not present homogeneously, because they depend on factors including means of transmission and degree of immune system compromise. Most appear when cellular immunity has weakened considerably, with a CD4 T-lymphocyte count < 200 per mm3. However, Kaposi sarcoma and the different forms of tuberculosis can develop with higher CD4 counts.
Others, such as toxoplasmosis, histoplasmosis and cryptococcosis, generally appear with a CD4 T-lymphocyte count < 100 per mm3, and cytomegalovirus and Mycobacterium avium-intracellulare complex appear when it is < 50 cells per mm3. Studies done in other countries have reported wasting, Pneumocystis jirovecii pneumonia and tuberculosis as the most frequent opportunistic infections.[36–38]
The observed proportion of HIV cases diagnosed late was low in comparison to some populations. A study of the Spanish VACH cohort[39] found that 18% of diagnosed HIV cases involved late presentation. In the United States, a study of intravenous drug users revealed 25% of cases presented late.[40]
In Cuba, increasing frequency of late presentation has begun to be noticed.[41,42] A study of all cases in Havana through 2007[43] found that late presentations increased starting in 2002; 8.5% of cases were diagnosed late, predominantly in men. However, this also happened to women, similar to what we found. The persistence of late presentation reflects the need to continue working with women, and suggests that screening approaches for early detection are still inadequate.
Case fatality rates began a downward trend in 1998, consistent with reports from other national and international studies. According to UNAIDS, the annual number of AIDS deaths worldwide has decreased because of ART availability.[1,3] Studies in African and European countries have reported lower mortality in women, directly related to ART use.[44–47] Development of highly active ART (HAART) has undoubtedly been one of the most important advances in modern medicine, and internationally, expanded access to HAART has been the most notable achievement in the response to the AIDS crisis. Coverage has reached 70% in Latin America and 95% in Cuba.[4,48]
One limitation of this study is that data were obtained from a pre-existent registry and not from direct case observation. This reduced the range of variables that could be analyzed and so interfered with ability to detect possible associations among some variables, since not all were current. The possibility of under-reporting cannot be ruled out. Nevertheless, in our literature review, we found no prior studies of HIV in women in Havana; we therefore believe that this study will open the door to new prospective studies.
Dissemination of these results will make it possible for the agencies responsible to strengthen their strategies, focusing primarily on prevention in this group, which is demonstrably vulnerable to HIV. It will also contribute to expanding the scientific community’s knowledge about this disease, focusing on women in particular.
CONCLUSIONS
This study reports on several characteristics of HIV infection among women in Havana from 1986 through 2011. A salient facet of increasing HIV and AIDS rates in the last decade is that they are affecting a predominantly young population with a middle-school educational level. The existence of late diagnosis is an incentive to maintain active screening of vulnerable groups and the overall population, regardless of age, which should serve as the basis for developing more effective prevention programs targeting this population.