INTRODUCTION
Chronic kidney disease (CKD) constitutes a global public health problem of epidemic proportions. Its main causes are diabetes mellitus, high blood pressure, glomerulopathies and polycystic kidney disease.[1] Much less common nephropathies with known causes specific to some geographic regions have been reported, such as endemic Balkan nephropathy and that caused by Chinese herbs.[2–5]
For over a decade, elevated prevalence and mortality have been reported from a chronic kidney disease of unknown etiology (CKDu) in several geographic zones, mainly in Asia (Sri Lanka and India) and Central America (Guatemala, El Salvador, Honduras, Nicaragua and southern Mexico). It is found in rural communities and primarily affects farmworkers, especially men and those in low-income brackets.[6–11]
CKDu’s high prevalence and incidence in El Salvador has spurred population-based epidemiological research in communities of the Bajo Lempa region to characterize the population affected and risk factors potentially associated with the disease.[9]
We found only three studies to date examining CKDu from a histopathological perspective. In one, 57 patients from Sri Lanka were assessed and authors identified tubulointerstitial damage as the main pathological event, with secondary vascular and glomerular lesions.[10] Another study of eight patients from Salvadoran agricultural communities was carried out in collaboration with researchers from Sweden’s Karolinska Institute. Pathological findings indicated tubulointerstitial disease with extensive glomerulosclerosis. Possible contribution of tubulointerstitial damage to glomerular damage was not ruled out, but they inferred from the relation between the chronic nature of the tubulointerstitial damage and glomerular changes that the latter constituted the primary event.[11] In a third study in Sri Lanka, tubulointerstitial lesions predominated, with no deposits seen on immunofluorescence, leading researchers to discard immune response as a possible cause.[12]
Given CKDu’s high prevalence in El Salvador and the attendant costs of renal replacement therapy, its histopathological characteristics are of particular interest, especially since previous descriptions are scarce and include few patients. Our objective was to characterize the histopathology of CKDu in patients from Salvadoran agricultural communities, describe the evolution of renal damage associated with each disease stage, and assess associations between histopathological alterations and sociodemographic variables.
METHODS
A descriptive cross-sectional study was conducted from March through April 2013, among persons aged ≥18 years in Salvadoran agricultural communities. CKD cases were identified from population-based epidemiological studies in 11 agricultural communities in 4 regions of El Salvador. Inclusion criteria: CKD stages 2 to 3b (glomerular filtration rate 89 mL/min/1.73 m2 to 30 mL/min/1.73 m2 body surface area)[13] who met clinical criteria for CKD. Exclusion criteria: HT, diabetes mellitus, glomerulopathies, polycystic kidney disease and obstructive kidney disease, HIV positivity, any social or clinical condition preventing participation. Of 60 patients who met CKD criteria, 14 were excluded, leaving a study sample of 46 patients.
All underwent clinical study, including interviews covering medical, toxicological and epidemiological information; specialized examination by organ system; blood and urine tests and imaging studies. Complete methods for the entire study are described elsewhere.[14]
Renal biopsies were performed on all participants by percutaneous technique under ultrasonographic control using an automatic biopsy gun (Dana 2.2 Histo, 14-gauge, USA). Biopsy specimens were fixed in neutral buffered formalin; a Sakura tissue processor (Japan) was used. A Leica microtome (Germany) was used to take sections of 2–3 µm for paraffin samples and a Microm cryostat (Germany) for fresh tissue sections.
Stains used were hematoxylin-eosin, periodic acid Schiff, Masson’s trichrome and methenamine silver. Immunofluorescence techniques (VWR thermo scientific, USA) were employed to assess presence, intensity and pattern of immune deposits: IgA, IgG, IgM, complement C1q and C3, and fibrin.
Total number of glomeruli and sclerosed glomeruli, and glomerular size increase were quantified. The Banff classification was used to assess degree of interstitial fibrosis, tubular atrophy, interstitial inflammatory infiltration, vascular lesions and glomerular changes.[15] Mesangial expansion and proliferation of mesangial, endocapillary and extracapillary cells were determined.
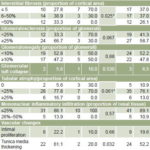
Study variables See Table 1.
Analysis All information was stored in Excel and processed with SPSS version 15.0 for Windows. The Fisher exact test was used to identify possible differences by sex, with significance threshold set at α = 0.05.
Ethical aspects The study protocol was approved by El Salvador’s National Committee for Clinical Research of the Higher Council of Public Health. Written informed consent was obtained from all participants.
RESULTS
Findings by age and sex During a two-month period, histopathological study was performed on 46 biopsies: 36 men (78.3%) and 10 women (21.7%). Mean patient age at time of biopsy was 45.4 years, with 30.6% aged <39 years. The youngest patient, aged 19 years, had severe tubular atrophy, interstitial fibrosis and glomerulosclerosis; his CKD had been diagnosed three years prior to biopsy (Figure 1b).
Table 1: Study variables

KDIGO: Kidney Disease: Improving Global Outcomes MDRD: Modification of Diet in Renal Disease
Interstitial fibrosis was the main lesion observed in the sample (Figure 2a), and was associated with male sex (p = 0.025): 38.9% (14/36) of men had mild to moderate interstitial fibrosis, and 33.3% severe. In contrast, none of the 10 women studied had severe interstitial fibrosis; 3 (30%) had mild to moderate fibrosis; and 7 had <5% (Table 2).
Glomerulosclerosis affecting ≥25% of tissue was present in 58.7% of patients, and was also more frequent among men: 66.7% (24/36) versus 30% (3/10) in women (Table 2). Glomerulomegaly (Figure 2c) of ≥10% of total glomeruli in the biopsy specimen was observed in 22 patients (47.8%), 47.2% (17/36) of men and 30% (3/10) of women (Table 2). Glomerular tuft collapse was found in biopsies from 2 men and 1 woman—all were in CKD stage 3 and none were non-sugarcane agricultural workers.
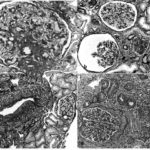
Figure 1: Histopathology of nephropathy in Salvadoran agricultural communities (optical microscopy images)
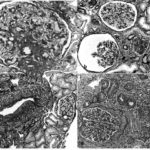
a. Perihilar focal segmental sclerosis lesion in enlarged glomerulus (PAS x 400)
b. Area of scarring with interstitial fibrosis, tubular atrophy, glomerulo sclerosis in 19 year-old sugarcane worker (silver methenamine x 100)
c. Artery intimal proliferation in a sugarcane worker (silver methenamine x 100)
d. Tubular atrophy, mononuclear inflammatory infiltration and glomerulus with basement membrane thickening of Bowman capsule and collagen in the Bowman space in a sugarcane worker in CKD stage 3b (PAS x 200)
PAS: periodic acid Schiff
(available in color online at www.medicc.org/mediccreview/lópez.html)
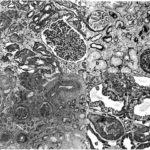
Figure 2: Histopathology of nephropathy in Salvadoran agricultural communities (optical microscopy images)
a. a. Mild to moderate interstitial fibrosis, enlarged glomerulus in a woman in CKD stage 2 (Masson trichrome x 200)
b. Area of scarring and interstitial fibrosis, tubular atrophy, glomerulus with thickened basement membrane of Bowman capsule and Bowman space occupied by collagen in woman in CKD stage 3a (silver methenamine x 100)
c. Extensive area of interstitial fibrosis, tubular atrophy and mononuclear inflammatory infiltration in relation to sclerosed glomeruli in non-sugarcane agricultural worker; enlarged glomerulus (PAS x 200)
d. Tubules with hydropic vacuolation (trichrome Masson x 400)
PAS: periodic acid Schiff
(available in color online at www.medicc.org/mediccreview/lópez.html)
Table 2: Histopathological lesions by sex
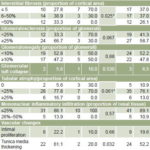
*1st vs. 2nd and 3rd categories combined
Mild inflammatory infiltration was present in 89.1% (41/46) of cases. However, no woman had more than mild inflammatory infiltration.
In 43.5% of participants, there was hydropic vacuolation, focal in all instances (Figure 2d). Tunica media vacuolation in blood vessels was observed in 47.2% (17/36) of men and 30% (3/10) of women. Only 19.6% (9/46) had intimal proliferation. Tunica media thickening was present in 61.1% (22/36) of men and 20% (2/10) of women (Table 2).
Findings by CKD stage There were 15 patients in CKD stage 2 and 31 in stage 3, 11 of the latter in stage 3a and 20 in stage 3b (Table 3). Extent of severe interstitial fibrosis (Figure 1d) increased with advancing CKD stage, from 13.3% of the patients in stage 2 to 63.7% in stage 3a and 100% in stage 3b (Table 3). Similarly, the extent of severe glomerulosclerosis increased over advancing stages, from 26.7% in stage 2 to 54.5% in stage 3a and 85.0% in stage 3b (Table 3). Perihilar focal segmental glomerulosclerosis was observed in only one participant (Figure 1a).
Glomerulomegaly (in ≥10% of total glomeruli) was found in 73.3% of stage-2 patients, 36.4% of stage-3a and 35% of stage-3b patients (Table 3).
Forty-one patients (89.1%) had tubular atrophy, which was mild to moderate in 76.1% (35/46) of patients and severe in 13%. All but one (30/31) stage 3 patient had this lesion; in stage 3b, tubular atrophy was severe in 20% (Table 3). (Figure 2b)
Table 3: Histopathological lesions by CKD stage

CKD: chronic kidney disease
Mononuclear inflammatory infiltration was mild in most patients. Moderate infiltration was most frequent in stage-3b patients, 20% (Table 3).
There was intimal proliferation in 6.7% of participants in stage 2 of the disease; however in stages 3a and 3b it was found in 36.4% and 20% respectively (Table 3).
Thickening of the tunica media in blood vessels was more evident in stage-3b patients (80%); in stage 2, it was observed in only 20%. Similarly, vacuolation of the tunica media was observed in 70% (14/20) of stage-3b patients, versus 20% (3/15) in stage 2 (Table 3).
Findings by occupation Sugarcane workers showed more severe interstitial fibrosis (38.9%) than non-sugarcane agricultural workers (20.8%).
Likewise, they showed more severe tubular atrophy (22.2%) than non-sugarcane agricultural workers (8.3%), and greater mononuclear inflammatory infiltration (22.2% moderate vs. 4.2%) (Table 4).
Glomerulomegaly ≥10% was observed in all three occupational groups, most frequently in those not working in agriculture (3/4, 75%) and least frequently in sugarcane workers (8/18, 44.4%) (Table 4).
Intimal proliferation was only observed in agricultural workers: 29.2% (7/24) of non-sugarcane agricultural workers and 11.1% (2/18) of sugarcane workers (Figure 1c) (Table 4).
Table 4: Histopathological lesions by occupation

C: sugarcane worker NC: non-sugarcane agricultural worker NA: non-agricultural
Thickening of the tunica media of extraglomerular blood vessels was similar in sugarcane workers and non-sugarcane agricultural workers (55.6% and 58.3%, respectively). None of the biopsies showed hyalinosis in the walls of extraglomerular blood vessels.
In one patient there was thickening of the basement membrane in glomerular capillaries, with diffuse vacuolation and protrusion of basement membrane material in spikes at some sites. This person had generalized, diffuse IgG deposits of moderate intensity. The diagnosis was early membranous glomerulopathy with severe tubulointerstitial nephritis.
Other None of the biopsies showed endocapillary, extracapillary or mesangial proliferation. Masson’s trichrome stain did not show fuchsinophilic deposits in any of the glomerular compartments (subepithelial, subendothelial or membranous), nor did it show fibrinoid necrosis or leukocyte infiltration in the tuft. Immunofluorescence techniques to detect immunoglobulins and complement found nonspecific deposits of IgM (25 patients), C3 (18) and C1q (8) in the glomeruli; 16 patients had no deposits. None of the biopsies showed immunoglobulin deposits in the tubules or interstitium.
DISCUSSION
CKDu was found in Salvadoran agricultural communities, predominantly in male agricultural workers, but also in women and adolescents. Thus, various factors that could contribute to developing the disease were taken into account in the clinical study: extreme poverty, environmental contamination due to misuse of agrochemicals, unsafe working conditions with exposure to high temperatures and toxic substances, in addition to excessive use of NSAIDs. In this paper, we analyzed histopathological findings in relation only to age, sex, occupation and disease stage. The two most discussed hypotheses concerning the cause of this new disease are chemical nephrotoxicity, and renal tissue ischemia secondary to dehydration and heat stress under harsh working conditions, so it is important to bear these in mind in interpreting the histopathology.[14]
Biopsy findings ruled out a diagnosis of glomerulonephritis due to incompatibility with the pattern and intensity of deposits seen in immunofluorescence studies.[13] Morphology was consistent with tubulointerstitial nephritis, but in different degrees depending on sex, occupation and CKD stage. Interstitial fibrosis was common to most biopsies and was associated with CKD stage. Some women in CKD stage 2 and some men who did not work in agriculture (that is, were not subject to such extreme working conditions) also had intersticial fibrosis, but to a lesser degree.
Wijkstrom studied eight Salvadoran patients, whose kidney biopsies examined at the Karolinska University Hospital showed mild to moderate tubular atrophy and interstitial fibrosis. They also showed generalized glomerulosclerosis in 29%–78% of patients. From this, the authors concluded that the fibrosis was secondary to the glomerular damage.[11] However, since the patients studied (all male) were in advanced stages of CKD, in which there is usually damage to all kidney tissue compartments,[1] these histopathological findings were only to be expected and cannot be used to establish relative order of appearance.
In our research, glomerular damage was found in most patients: even in women and younger patients, independent of occupation.[13] In patients in CKD stage 3, it becomes more evident, explaining the decreased kidney function.
The severe tubulointerstitial damage with areas of tubular atrophy and severe fibrosis observed in the patient diagnosed with incipient membranous glomerulopathy are not seen in early membranous glomerulopathies; therefore, either there are two coexisting diseases or the damage was secondary to some other process (such as cancer or medication). We cannot discount either possibility.[16,17]
Segmental sclerosis observed in one patient was interpreted as the onset of generalized glomerulosclerosis, because of the appearance of nonspecific IgM and C3 deposits on immunofluorescence that suggested generalized sclerosis beginning as a perihilar lesion.[18] Furthermore, there were no clinical or laboratory findings suggesting an initial glomerular insult.
The glomerulopathy observed in the study is due to glomerulosclerosis with nephron loss.[19,20] Compensatory glomerular hypertrophy is an adaptive mechanism and enlarged glomerular volume leads to development of glomerulosclerosis and high blood pressure.[21,22]
Mononuclear inflammatory infiltration was observed in areas of atrophy and glomerulosclerosis. Chronic pyelonephritis has a similar pathological appearance, but was ruled out due to absence of any clinical, laboratory or imaging history compatible with that diagnosis.[23]
Findings very similar to ours were described for biopsies of 57 CKDu patients in Sri Lanka. Glomerulosclerosis was the most frequent lesion. Although interstitial inflammatory infiltration was absent in 40% of cases, there were only 4 without interstitial fibrosis, suggesting that tubulointerstitial damage is the main pathological event in the CKDu, with glomerulosclerosis occurring secondarily.[10] Other researchers in Sri Lanka have investigated toxic environmental factors as the possible cause of Sri Lankan endemic nephropathy. They found high concentrations of arsenic in urine of CKD patients[24] and high concentrations of cadmium in well water where the patients lived,[25] suggesting these heavy metals as a source of environmental contamination.
Lead is one heavy metal long known to cause damage similar to what we observed. Cramér studied kidney biopsies from patients exposed to lead and found tubular damage and interstitial fibrosis without damage to glomeruli and vasculature.[26] While some of our findings were consistent with longterm exposure to heavy metals, we did not observe nuclear inclusion bodies or any other sign of acute lead poisoning.
This research is the first in the Americas to study the histopathology of a large number of patients in different stages of CKDu. One limitation is lack of ultrastructural study with electron microscopy, which could provide more details to the general description of lesions.
CONCLUSIONS
The most important and striking lesion in the cases studied, interstitial fibrosis, accompanied by glomerular damage (in most biopsies) and classic tubular atrophy, led to the histopathological diagnosis of chronic tubulointerstitial nephritis, since it increased directly with CKD stage. More research is needed to define the fundamental and contributing causes of CKDu, whether toxic environmental or other occupational exposures, chronic ischemia from dehydration, or nephrotoxic medications, all of which are compatible with the histopathological picture we observed and the social and epidemiologic context of the epidemic. Our findings are also consistent with a multifactorial etiology for this disease.