INTRODUCTION
In 2000, global estimates indicated 171 million people had diabetes mellitus (DM), projected to reach 366 million by 2030.[1] As DM evolves, it produces endothelial dysfunction and changes in energy metabolism that lead to atherosclerosis in medium- and large-caliber arteries, creating lesions in coronary, cerebrovascular and peripheral arteries. In diabetics, atherosclerotic plaque tends to develop earlier, evolve more quickly and be more diffuse. All these factors contribute to DM patients having two to four times greater risk of a cardiovascular event than nondiabetics, with cardiovascular disease (CVD) being the main cause of death in these patients.[2] In 2008, WHO reported a combined mortality rate from CVDs and DM of 245 per 100,000 population for adults aged 30 to 70 years.[3]
Cardiac mortality for diabetics with no known coronary disease is the same as that for non-diabetics with a history of acute myocardial infarction, which is why clinical guidelines consider diabetics at high risk for CVD.[2]
Presence of cardiac autonomic dysfunction, common in diabetics,[4] is a factor that influences the frequently silent appearance of myocardial ischemia. Hence the importance of identifying individuals with high risk for cardiovascular events, even prior to symptom onset. DM also affects vascular endothelium, causing endothelial dysfunction.[5] The American Diabetes Association[6] therefore recommends performing stress tests on asymptomatic diabetics who present a minimum of two additional risk factors (such as hypertension, dyslipidemia and smoking). This approach, however, is still controversial.
How can silent ischemia be detected in diabetics? The first step in diagnosing silent ischemia in asymptomatic DM with two or more additional risk factors is a stress test,[7] whether with a treadmill or bicycle ergometer.
Ergometry provides valuable functional results—not only for detecting ischemia, but also for assessing functional capacity, as well as behavior of arterial pressure and arrhythmia on exertion.[7] Its availability and utility make it the first option for patients without diabetic neuropathy who are able to do physical exercise.
In patients with low functional capacity, imaging techniques such as echocardiography or myocardial perfusion scintigraphy (MPS) are more helpful, since they have acceptable sensitivity and specificity, and allow pharmacological stressors (dobutamine in echocardiogram; dipyridamole or dobutamine in MPS) to substitute for physical exercise.[8–12] An alternative for patients able to do physical exercise would be a stress MPS, which combines data from a stress ECG and functional capacity with that from an MPS.
MPS with single-photon emission-computed tomography (SPECT) is a validated nuclear medicine technique for obtaining functional information about the heart by demonstrating myocardial ischemia. If images are synchronized with ECG (gated SPECT or gSPECT), a single study can provide data on myocardial perfusion as well as intraventricular synchronism and ventricular function (left ventricular ejection fraction and systolic wall thickening, which permit assessment of segmental wall-motion abnormalities).[10] gSPECT can be extremely useful in diagnosis and risk stratification in patients with CVD. Nuclear cardiology techniques have been used in Cuba since the 1980s and are currently available free of cost to patients in several tertiary care centers.
Two other imaging techniques, although not used in the same way as echocardiography and MPS to detect ischemia, provide complementary data useful for diagnosis. The first is the coronary calcium score obtained through computed axial tomography (CAT);[11,12] it quantifies calcium in coronary arteries and is therefore an indicator of CVD, although since it provides structural rather than functional information, it cannot detect ischemia. The second method is measurement of endothelial function, which can be assessed in the brachial artery by using ultrasound to measure flow-mediated endothelium-dependent vasodilation, as described by Celermajer.[13] Marcus[14] found that impairment of endothelium-dependent vasodilation in coronary resistance vessels (<450 μm in diameter) may be associated with perfusion abnormalities in diabetics, even in the absence of stenotic lesions in epicardial coronary arteries, suggesting the presence of microvascular CVD. This test is more widely available, since it requires only ultrasound equipment and an echocardiographer trained in the technique
DIAGNOSTIC APPROACH TO DETECTING SILENT ISCHEMIA IN DIABETICS
There are several different algorithms for detection of silent ischemia in diabetic patients. The experience of our working group at Cuba’s cardiology and endocrinology institutes is reviewed below. All data have been published previously as cited.
As part of multicenter research coordinated with the International Atomic Energy Agency, we studied a group of 59 diabetic patients, comparing them with a control group of 42 participants (who were not diabetic but had coronary risk factors) to detect silent ischemia through MPS, coronary calcium score and endothelial function assessment.[15]
We found that 69% of DM patients with stress-induced ischemia in MPS had impaired endothelium-mediated vasodilation, which can be interpreted as a manifestation of endothelial dysfunction. However, only 43% of nondiabetic patients with other atherosclerotic risk factors had involvement of endothelium-mediated vasodilation.[15]
These results are supported by the findings of Papaioannu,[5] who used ultrasound to measure endothelium-dependent and independent vasodilation in the brachial artery in a subgroup of 75 asymptomatic diabetics in the Detection of Ischemia in Asymptomatic Diabetics (DIAD) study; it was determined that ≥8% endothelium-dependent vasodilation had a negative predictive value of 93% for CVD.
Perfusion abnormalities have been detected in a relatively high percentage (25%–50%) of asymptomatic diabetics in different series.[16,17] Two studies have been conducted in Cuba to date using gSPECT: one by Peña,[18,19] which included 220 patients and found ischemia in 29.1%; and the second by Peix,[15] that found 33% of patients with DM had ischemia versus 16% of those without (p = 0.04). Figure 1 presents an example of a diabetic patient with silent myocardial ischemia diagnosed by gSPECT.
To date, MPS has been used in only two other studies to examine prevalence of ischemia in asymptomatic diabetics: the DIAD study[4] and that of Scholte,[20] which detected ischemia in approximately 20% and 33% of cases, respectively, independent of the number of risk factors. However, unlike the Peix study, neither of these used physical exercise as a stressor or had control groups.[15]
Presence of coronary calcium is associated with risk of cardiac events, with 1–99 Agatston units indicating low risk; 100–400, moderate risk; and >400, high risk.[21] A prospective study by Anand[11] followed a two-stage strategy: a calcium score was derived for all patients through multislice CAT scan, followed by gSPECT for those who scored >100 Agatston units and for a random sample of those with scores of ≤100. Some 32% of MPS showed perfusion abnormalities corresponding to ischemia. Scintigraphic abnormalities diagnostic of ischemia were present in 23% of patients with Agatston scores of >100, 48% of those with scores of >400 and 71% of those with scores of >1000. The authors found that the more diffuse the ischemia the worse the clinical evolution; that the calcium score was better than established risk factors at predicting silent ischemia and cardiac events in persons with DM; and that a coronary calcium score of 0 to 10 Agatston units was associated with normal scintigraphy and excellent prognosis.[11]
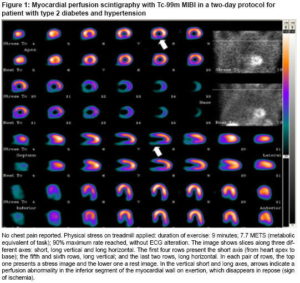
Figure 1: Myocardial perfusion scintigraphy with Tc-99m MIBI in a two-day protocol for patient with type 2 diabetes and hypertension
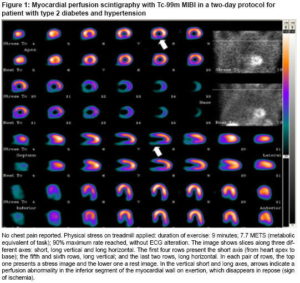
No chest pain reported. Physical stress on treadmill applied: duration of exercise: 9 minutes; 7.7 METS (metabolic equivalent of task); 90% maximum rate reached, without ECG alteration. The image shows slices along three different axes: short, long vertical and long horizontal. The first four rows present the short axis (from heart apex to base); the fifth and sixth rows, long vertical; and the last two rows, long horizontal. In each pair of rows, the top one presents a stress image and the lower one a rest image. In the vertical short and long axes, arrows indicate a perfusion abnormality in the inferior segment of the myocardial wall on exertion, which disappears in repose (sign of ischemia).
Source: Nuclear Medicine Department, Cardiology and Cardiovascular Surgery Institute, Havana, Cuba
The color scale appears at the right of the image. The top of the scale represents 100% radiopharmacological uptake.)
In the Peix study, coronary calcium levels in diabetic patients averaged 74 Agatston units compared to 5 in controls (p = 0.01).[15] Eight diabetics had calcium scores of >100, which in only three cases coincided with presence of perfusion abnormalities on MPS. In two studies in Japan and Israel using CAT scans to compare asymptomatic diabetic with nondiabetic patients,[22,23] prevalence of coronary plaques was 80% to 93% in asymptomatic diabetics, and significant coronary stenosis was more prevalent in diabetics than in the control group. Scholte[24] found that 41% of plaques were not calcified, thus undetectable by calcium scoring, while Raggi[12] found coronary artery calcification in 40% of diabetics. An appropriate approach for these patients could be the combination of both tests: coronary calcium score and myocardial perfusion scintigraphy, thus providing important complementary data.
The two-stage strategy (calcium score followed by perfusion scintigraphy for patients with scores of >100) combines both types of data: structural (through coronary calcium) and functional (through MPS-detected ischemia). However, even this should be viewed with caution because, while more useful in cases of calcified epicardial coronary lesions, this approach could miss noncalcified soft plaques and microvascular angina. Microvascular angina is a diagnosis of exclusion once ischemia is detected in a patient with typical angina and normal epicardial coronary arteries. Missing the presence of noncalcified soft plaques, and so excluding MPS, would be a drawback of this strategy. Presence of DM in addition to peripheral vascular diseases, carotid disease, peripheral neuropathy, autonomic dysfunction, family history of CVD or renal insufficiency confers additional risk and reinforces the need for testing to detect ischemia; we therefore recommend performing MPS in such cases, even if the calcium score is less than 100.
Peña[18,19] found that alterations in lipids, fasting blood sugar, hypertension, smoking and family history of heart disease increased risk of a positive gSPECT two- to five fold. An LDL level of ≥100 mg/dL was the variable conferring greatest estimated risk, while an HDL level of <44 mg/dL was the most important standardized variable when several factors were present.
In the Peix series, DM was the only significant risk factor associated with perfusion abnormalities (p = 0.03). However, coronary calcium of >100 Agatston units, abnormal endothelium-dependent vasodilation (<5%) and a cholesterol/HDL index of >4 were associated with perfusion abnormalities in asymptomatic diabetics.[15]
Another interesting aspect that can be evaluated through nuclear techniques is cardiac autonomic innervation, which is frequently impaired in individuals with DM; such impairment constitutes an independent marker of poor prognosis, probably due to increased rates of sudden death from malignant ventricular arrhythmia. The most common method is SPECT scintigraphy with metaiodobenzylguanidine, a norepinephrine analogue, labeled with iodine-123 (123I). Patients with DM and cardiac autonomic neuropathy have reduced myocardial metaiodobenzylguanidine uptake, which has been associated with long-term adverse cardiovascular events.[25]
After completion of the DIAD study and publication of its five-year results,[4,26,27] although screening did not have an impact on adverse cardiac events overall, it was useful in classifying patients as high risk (moderate-to-severe abnormalities and ischemia on stress ECG) and low risk (small defects or normal perfusion). Hence it would be preferable to test for ischemia more selectively rather than testing all diabetics.
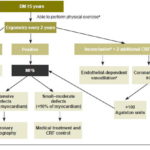
We suggest that asymptomatic patients who have had DM for at least five years and are able to do physical exercise take an ergometric test every two years to detect silent ischemia. For those with inconclusive ergometry and two risk factors in addition to DM, we suggest including an endothelium-dependent vasodilation test and coronary calcium score prior to performing an imaging stress test (either stress echocardiography or MPS).
In patients who are unable to do physical exercise, an alternative to consider is pharmacological stress with dobutamine or dipyridamole (either echocardiography or MPS). Figure 2 presents an overview of this algorithm proposed for diagnosing silent ischemia in diabetics.
Interestingly, in 79% of patients in the DIAD study with ischemia on initial MPS, ischemia resolved in the third year.[26] This pattern was associated with intensified treatment using aspirin, statins and angiotensin-converting enzyme inhibitors. However, the authors point out that since the study was not designed as a treatment trial, this association cannot be considered evidence of a causal relation.
Our working group is currently conducting a third-year assessment of the diabetic group studied. To date, we have observed resolution of ischemia in 71% of cases, also coinciding with intensified medical treatment and more aggressive control of coronary risk factors (Peix A, Cabrera LO, Castillo I, Heres F, Rodríguez L, Padrón K, Valiente J, Llanes R, Mendoza V, Licea M, Gárciga F, Dondi M; unpublished data), similar to the DIAD results. This line of inquiry requires more extensive prospective studies, emphasizing the need for early diagnosis of ischemia in these patients through diagnostic techniques available in Cuba and described above. Early detection of ischemia will support customized individual treatment with both medications and appropriate management of behavioral risk factors.
Figure 2: Proposed algorithm for detecting silent ischemia in asymptomatic diabetic patients
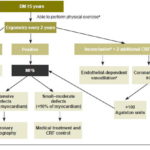
DM: diabetes mellitus CRF: coronary risk factors MPS: myocardial perfusion scintigraphy a If patients cannot perform exercise, pharmacological stress can be applied with dobutamine or dipyridamole(with echocardiogram or MPS) b When patient does not reach submaximal heart rate: 85% of maximum (220 minus age) c Altered endothelium-dependent vasodilation provides information on endothelial function to better orient treatment
CONCLUSIONS
Noninvasive imaging techniques have been shown to be extremely useful in diagnostic and prognostic assessment of coronary disease in individuals with DM, but such techniques must always be judiciously applied and in combination with clinical examination, evaluating atherosclerotic risk factors and applying an appropriate diagnostic algorithm