ABSTRACT
Introduction Tuberculosis (TB) is a major cause of illness and death throughout the world. The World Health Organization’s Global Plan to Stop TB 2006-2015 proposes that countries cut TB mortality by half compared to 1990 rates. In Cuba, TB mortality declined steadily throughout the 20th century, particularly after 1960.
Objective Describe TB mortality distribution and trends in Cuba from January 1998 to December 2007 by infection site, sex, age and province, and determine progress towards the WHO’s 2015 target for TB mortality reduction.
Methods A time series ecological study was conducted. Death certificates stating TB as cause of death were obtained from the Ministry of Public Health’s National Statistics Division, and population data by age group, sex, and province were obtained from the National Statistics Bureau. Crude and specific death rate trends and variation were analyzed.
Results TB mortality declined from 0.4 per 100,000 population in 1998 to 0.2 (under half the 1990 rate) in 2007. Clinical forms of the disease, both pulmonary and extrapulmonary, also declined. The highest mortality rates were found in males and in the group aged ≥ 65 years. Rates were also highest in the capital, Havana, with extreme values of 0.73 and 0.39 per 100,000 population at the beginning and end of the period, respectively.
Conclusions Deaths from TB declined steadily compared to total deaths and deaths caused by infectious diseases. The Global Plan to Stop TB target was met well ahead of 2015. If this trend continues, TB is likely to become an exceptional cause of death in Cuba.
Keywords Lung diseases, tuberculosis, mortality, communicable diseases, trends, Cuba
INTRODUCTION
Tuberculosis (TB) is an infectious disease of acute, subacute or chronic evolution that mainly affects the lungs. It is caused by the Mycobacterium tuberculosis complex and is associated with socioeconomic factors such as extreme poverty, illiteracy, poor environmental and hygienic conditions (overcrowding), stress, and lack of health care. Other determining factors are immunological deficiencies, and, ultimately, the virulence of M. tuberculosis and its resistance to drug therapy.[1]
TB is a major cause of illness and death, especially in Asia and Africa. In 2006, an estimated 9.2 million new cases were detected worldwide; 4.1 million patients tested positive to acid-alcohol resistant (acid-fast) bacilli (AFB); of these, 0.7 million were HIV positive; and a total of 1.7 million deaths due to TB were reported. In the Americas, estimated incidence of all forms of TB in 2006 was 330,724 cases, of which approximately half were AFB+, with approximately 40,600 deaths. The United States reported very low TB rates with an incidence of 4.6 cases per 100,000 population and a mortality rate of <1 per 100,000.[2]
In Cuba, the incidence of all forms of TB has declined and is currently one of the lowest in Latin America,[2] sustained at about 7 per 100,000 population from 2001 to 2007.[3] The health ministry’s Public Health Projections for 2015[4] include a proposal for moving toward elimination of TB as a public health problem,[5-7] and Cuba is working with other low-prevalence countries in Latin America and the Caribbean toward lowering incidence to <5 cases per 100,000 population as the first stage in reaching the elimination target.[8]
TB mortality was high in Cuba throughout the Spanish colonial period.[9,10] From 1887 to 1891, it was one of three main causes of death in Havana. In 1902, it was the main cause of death nationally, accounting for 4,001 fatalities or 15.7% of total deaths. [11] Mortality then declined steadily throughout the 20th century.
Yet, before 1959, TB still caused over 1,000 deaths annually.[10] By 1997, this figure had dropped to 82 deaths (0.7 per 100,000) [11] as a result of improved socioeconomic conditions after the 1959 revolution,[12,13] development of a universal healthcare system, and initiation in 1963 of a comprehensive TB control program, which has since progressed through several stages. Initially, treatment involved sanatorial care with continued assessment and risk evaluation. In 1971, this was replaced by controlled ambulatory treatment with isoniazid and streptomycin, administered in two phases for 12 months at community polyclinics. In 1982, Directly Observed Treatment, Short-course (DOTS) was adopted and also administered at polyclinics. This nine-month regimen included a daily dose of isoniazid, rifampicin, pyrazinamide and streptomycin during the first two months, followed by isoniazid and rifampicin twice a week through the 38th week. In 1987, this same regimen was shortened to 28 weeks with an eight-week first phase and 20-week second phase, administered in local family doctor offices. In 1993, the same DOTS regimen was revised to comprise 100 doses, 60 in the first phase and 40 in the second. In 1997, the program was reinforced with a six-month preventive isoniazid therapy aimed at containing the source of infection in pulmonary TB contacts who show positive bacilloscopy.[14]
The World Health Organization’s Global Plan to Stop TB 2006- 2015 calls for countries to cut TB mortality by half compared to 1990 rates.[15] In Cuba, the 1990 mortality rate was 0.5 per 100,000 population,[11] such a low rate paradoxically presenting greater challenges for meeting the WHO goal.
The objective of this article is to describe TB mortality distribution and trends in Cuba from 1998 to 2007 by infection site, sex, age and province of residence, and determine progress towards WHO’s 2015 target for TB mortality reduction.
METHODS
A time series ecological study was conducted on TB mortality in Cuba from January 1998 through December 2007. Death certificates stating TB as the primary cause of death during that period were used to identify the 384 individuals included in the study. The Ninth Revision of the International Statistical Classification of Diseases (ICD-9) was used for the period from 1998 to 2000, and the Tenth Revision (ICD-10) for the years 2001 to 2007.[16,17]
Data sources included mortality figures available in the Ministry of Public Health’s (MINSAP) National Statistics Division, population estimates for 1998 to 2007 from the National Statistics Bureau,[18] and MINSAP’s statistical yearbooks.[3] The following variables were examined: lesion site (pulmonary/PTB and extrapulmonary/ ETB), sex, age and province of residence.
The variation in the crude and specific death rates, as well as the proportional mortality ratio (PMR) in relation to total deaths and deaths from infectious diseases, were calculated. TB mortality distribution and trends were analyzed in two ways: first, crude death rates for the period were analyzed by age and sex. Since no significant differences in population structure were found when comparing 1998 to 2007,[3] age and sex did not introduce confounding biases. Second, in order to make any comparison, standardized rates for the series were estimated using the direct method[19] with a standard population of 100,000, as proposed by the Pan American Health Organization (PAHO), distributed proportionally (pi) by age group, as follows: 0-14 years, p1 = 0.157; 15-24 years, p2 = 0.260; 25-44 years, p3 = 0.323; 45-64 years, p4 = 0.225; ≥65 years, p5 = 0.035. Estimates were made as follows: Te = p1t1 + p2t2 + p3t3 +…+ pntn, where Te = standardized or age-adjusted rate, p = weight (proportion of the population in each age group) and t = age-specific mortality rate for each group.[20]
Global variation and average annual variation in the TB mortality rate for the period studied were determined using the initial and final years of the series as follows:
- Global variation = [(Final year crude death rate minus initial year crude death rate) divided by initial year crude death rate] x 100
- Average annual variation = Global variation divided by (total years minus 1) Global variation and annual variation in the average mortality rate by province were determined using the average mortality rate from the first two and last two years of the series, calculated as follows:
- Global variation = [(Final average rate minus initial average rate) divided by initial average rate] x 100
- Average annual variation = Global variation divided by (total years minus 1)
RESULTS
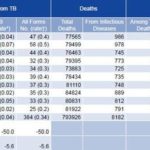
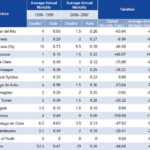
All clinical forms of TB declined during the decade under study. Mortality rates were highest for PTB, reaching a peak in 1999 of 0.45 per 100,000 population, but nevertheless exhibiting a global reduction of 47.4% and an average annual reduction of 5.3%. ETB also declined from 0.04 per 100,000 population in 1998 to 0.02 per 100,000 in 2007, with a total reduction of 50% and an average annual reduction of 5.6%. Age-adjusted rates exhibited the same steady decline as the crude rate values reported and even reached equal value in 2007 (Table 1).
Table 1: TB Deaths and Proportional Mortality in Cuba, 1998 to 2007
PTB: Pulmonary TB ETB: Extrapulmonary TB PMR: Proportional Mortality Rate.
* Specific death rate per 100,000 population
† Crude death rate per 100,000 population
Source: National Statistics Division, Ministry of Public Health, Havana.
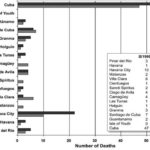
Figure 1: TB Deaths by Province in Cuba, 1998 to 1999
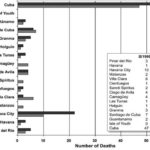
Source: National Statistics Division, Ministry of Public Health, Havana.
TB mortality declined from 47 deaths in 1998 (0.4 per 100,000 population) to 25 in 2007 (0.2 per 100,000 population) (Table 1), although in 1999 the number of deaths increased to 58 (considered an atypical year), mainly due to higher figures for Havana City province (10 deaths in 1998 and 22 in 1999) (Figure 1).
The PMR for TB in relation to total deaths in Cuba was 0.06% in 1998 and 0.03% in 2007 (Table 1), a total decline of 50% and an average annual reduction of 5.6%. The PMR for TB compared to total deaths from other infectious and parasitic diseases was 4.77% in 1998, dropping to 3.16% in 2007 for a total reduction of 33.7% and an average annual reduction of 3.74%. The highest PMRs were observed in 1999 (5.93%) and 2000 (5.91%).
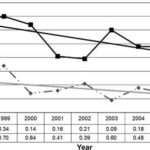
Figure 2: TB Mortality in Cuba by Sex, 1998 to 2007
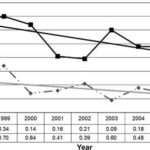
Source: National Statistics Division, Ministry of Public Health, Havana.
More deaths were reported among men than women (290 compared to 94), and male mortality was higher for every year (Figure 2). Following a downward trend at the beginning of the series, an increase in male mortality was observed in 2003, reaching a rate of 0.60 per 100,000 population, which later dropped to 0.31 per 100,000 population in 2007 (a global reduction of 51.9% and an average annual reduction of 5.76%). Mortality also dropped among women from 0.18 per 100,000 population in 1998 to 0.12 per 100,000 population in 2007. The overall decline was smaller compared to that of men (30.7%, with an average annual reduction of 3.4%). The male/female mortality ratio was 3:1.
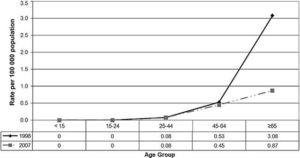
The group aged ≥65 years exhibited the highest mortality rate and the greatest decline (71.75% total reduction, 8% average annual decline) (Figure 3). The mortality rate for the group aged 45 to 64 years also fell from 0.53 to 0.45 per 100,000 population between 1998 and 2007 (15.05% total reduction, 1.7% annual average).
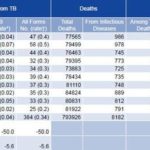
During the period studied, mortality declined in 73.3% (11/15) of Cuban provinces (Table 2). The greatest reductions occurred in Granma, Villa Clara, Ciego de Avila and Pinar del Río provinces; rates remained constant in Sancti Spíritus and Holguín, and no deaths from TB were reported on the Isle of Youth.
Matanzas was the only province showing increased mortality (46.67% total increase and an average annual increase of 5.19%), but this rate represents a total of 3 deaths in 2006-2007, compared to 2 deaths in 1998-1999. The largest number of deaths during the decade studied, 134 (34.9% of total deaths from TB), occurred in Havana City province.
DISCUSSION
During the period studied, the overall decline in TB mortality in Cuba coincided with the relatively small number of new cases reported each year. This low incidence can be attributed to the sustained application of the National TB Control Program (NTCP) over the past 45 years[14] with a DOTS strategy in place since 1982.[6,7] In 2006, the NTCP achieved a 92% treatment success rate and a 94% detection rate of new AFB+ cases,[2] well above the targets established by WHO’s Global Plan 2006-2015.[15]
The NTCP’s impact on TB mortality over time was enhanced by significant social and economic development over the last four decades,[5- 7,21] as well by public access to a free, universal healthcare system, with broad communitybased primary care coverage. [4] By 1974, TB mortality no longer figured among the 10 main causes of death in Cuba;[21,22] since 2003, it has ranked 33rd,[3] therefore considered a rare phenomenon.[11] Crude death rates of <1 per 100,000 population have been reported since 1981.
Figure 3: TB Mortality in Cuba by Age Group, 1998 to 2007
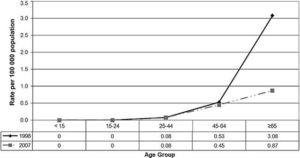
Source: National Statistics Division, Ministry of Public Health, Havana.
In 2007, Cuba met the Global Plan target for reduction of TB mortality, when the mortality rate reached 0.22 per 100,000[15] or half the1990 rate of 0.5 per 100,000.[14] This achievement also constitutes a contribution to attaining Goal 6.C of the Millennium Development Goals (MDGs).[2]
Table 2: Variation in Average Annual TB Mortality in Cuba by Province, 1998 to 2007
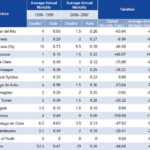
* Average Annual Deaths = total number of deaths divided by number of years
† Global Variation = final average annual mortality rate minus initial average annual mortality rate divided by initial average annual mortality rate x 100
‡ Average Annual Variation = Global variation divided by number of years minus one
Source: National Health Statistics Division, Ministry of Public Health, Havana.
The decline in Cuba’s TB mortality is similar to that registered by most developed countries during the 20th century and the beginning of the 21st.[9,11] In 2006, the majority of industrialized countries, including Canada, United States, Switzerland, Sweden, Denmark, Finland and Germany, reported mortality rates <1 per 100,000 population for all forms of TB. However, other highly developed countries with broad-coverage healthcare programs, such as the UK and Japan, still reported rates of 2 and 3 per 100,000 population, respectively.[2,23]
On the other hand, in many developing countries TB mortality has not steadily declined and remains very high.[24,25] In the Americas in 2006, estimated TB mortality per 100,000 population was 58 in Haiti, 30 in Bolivia, 29 in Guyana, 26 in Ecuador, 16 in Peru, 15 in the Dominican Republic, 13 in Surinam, and 12 in Paraguay.[2] In Africa, the situation is even worse as a result of the HIV/AIDS epidemic aggravated by socioeconomic problems.[ 26,27] In 2006, estimated TB mortality per 100,000 population was 218 in South Africa, 131 in Zimbabwe, and 117 in Mozambique.[2] Poverty, together with high HIV infection rates, drug resistance and weak healthcare systems have been cited as important factors contributing to these high rates,[2,27] since mortality is closely linked to the availability of prompt and effective drug therapy.[1]
Compared to other countries, TB incidence and mortality rates in Cuba have not been greatly affected by the HIV/AIDS epidemic or by multi-drug resistance (MDR). By 2004, HIV prevalence in Cuba was the lowest in the Americas at 0.05%,[28] and MDR reported for Cuba in the last WHO global resistance study (2004) was 0.3%.[29]
PTB is by far the most frequent clinical form of the disease globally[1,5,6] and contributes the largest number of deaths to TB mortality rates in Cuba[10,11] and the rest of the world as concluded in other studies[30-33] and international reports.[2,23] The international literature also includes reports of an increase in ETB,[34-37] mainly in HIV-positive patients, but ETB is rarely seen in Cuba.[7,11]
Most deaths from TB in Cuba occurred in males, who present the highest morbidity, which is consistent with reports in national and international literature.[10,11,26,37,38] The relative decline observed in males in 2001 and 2002 may be random. In some countries, higher mortality rates in females of all ages have been described.[30,38] However, in most poor countries, much higher TB mortality is reported among males.[2,27,31,39]
In countries with low TB prevalence, the disease affects mainly older adults, due to an endogenous reactivation,[5,24] although an increase has been seen in younger people due to the HIV/ AIDS epidemic.[38] Mortality in children is highest in the group aged <5 years.[40-43]
In Cuba, most deaths occur in the group aged ≥65 years, and TB mortality for this group and for children is similar to that of countries with adequate health care systems.[26,40,41,44,45] Increased rates in other age groups do not affect the mortality trend, since the number of deaths is very low, even among HIV/ AIDS patients. Childhood tuberculosis occurs infrequently, and is rare or exceptional in children aged <1 year, with very low rates reported throughout the country[41] and minimal mortality.
Mortality declined over the decade in most provinces with the exception of Matanzas, where a slight increase was reported but not considered significant. In Havana City province, which registered 35% of total deaths, mortality rates declined but still remained above the national average. According to NTCP data, the national increase observed in 1999 was largely the result of greater mortality in this province, linked to an increase in the number of severe cases in some long-term healthcare facilities. This pattern in the capital over time also coincides with descriptions in the literature regarding large urban areas.[46,47] Havana is the most heavily populated city in the country with more than 2 million inhabitants and a large floating population of migrants from the rest of the country, aggravating difficulties posed by the shortage of adequate housing.[21] To obtain a deeper understanding of mortality in Havana City, it would be worthwhile to explore inherent factors in individuals presenting TB that may affect their delay in seeking services and the quality of health care received. Such factors would include comorbidity, educational level and awareness of the importance of cooperating with treatment.
CONCLUSIONS
During the period studied, deaths from TB in Cuba steadily declined with respect to total deaths and deaths from infectious diseases; the target set for 2015 by the WHO Global Plan to Stop TB was met well in advance. If this trend continues, TB may become an exceptional event among causes of death in Cuba. Reducing morbidity and transmission of the disease until its elimination as a health problem in the country remains the NTCP’s primary goal.[7,8] To this end, several measures have been proposed to reinforce the program, particularly in Havana City province. These include strengthening early detection, contact tracing and case finding; stricter follow-up and control of drug treatment and prophylaxis; enhanced laboratory services; and new operations research studies to determine factors associated with TB lethality and mortality. (Annual Report on Infectious Diseases: Provincial Hygiene and Epidemiology Center. Havana, 2008.)
References

- Rieder HL. Bases epidemiológicas del control de la tuberculosis. Paris: UICTER; 1999. p.131-40.
- World Health Organization. Global Tuberculosis Control 2008. Surveillance, Planning, Financing. Geneva: WHO; 2008. [cited 2008 July 31]. Available from: http://www.who.int/tb/publications/ global_report/2008/en/index.html
- Anuarios Estadísticos de Salud 1998-2007. Havana: Ministry of Public Health, National Statistics Division; 1998-2007. [cited 2008 July 31]. Available from: www.sld.cu/servicios/estadisticas/ anuario_res.php
- Ministry of Public Health (CU). Proyecciones de la Salud Pública en Cuba para el 2015. Havana: Ciencias Médicas; 2006.
- González Ochoa E, Armas Pérez L, Alonso A. Tuberculosis in the Republic of Cuba: its possible elimination. Tuber Lung Dis. 1994;75:188-94.
- Marrero A, Caminero JA, Rodríguez R, Billo NE. Towards elimination of tuberculosis in a low income country: the experience of Cuba, 1962-97. Thorax. 2000;55:39-45.
- González Ochoa E, Armas Pérez L, Llanes Cordero MJ. Progress towards tuberculosis elimination in Cuba. Int J Tuberc Lung Dis. 2007;11(4):405-11.
- Pan American Health Organization/World Health Organization. 1ra Reunión Subregional de países de baja prevalencia de tuberculosis. Eliminación de la tuberculosis como problema de salud pública. 1999 Nov 29-Dec 2; San José de Costa Rica, Costa Rica, (OPS-HCP-HCT-165.00). Washington DC: WHO; 2000.
- Beldarraín E. Apuntes para la historia de la lucha antituberculosa en Cuba. Rev Cubana Salud Pública.1998;24:97-105.
- Toledo HJ, Padilla O, Vidal I, Rodríguez I. Mortalidad por tuberculosis en Cuba, 1987- 1993. Rev Cubana Med Trop. 1996;48:209-13.
- González Ochoa E, Borroto Gutiérrez S, Armas Pérez L, Díaz C, López E. Mortalidad por Tuberculosis en Cuba, 1902-1997. Rev Cubana Med Trop. 2003;55:5-13.
- Spiegel JM, Yassi A. Lessons from the margins of globalization: appreciating the Cuban paradox. J Public Health Policy. 2004;25(1):85-110.
- Araujo L, Llorens J. La Lucha por la Salud en Cuba. Mexico: Siglo XXI, 1985.
- Ministry of Public Health (CU). Programa Nacional de Control de la Tuberculosis. Manual de Normas y procedimientos. Havana: ECIMED; 1999. p.15-18, 39-45.
- World Health Organization. The Global Plan to Stop TB, 2006-2015. Actions for life – towards a world free of tuberculosis. Geneva: WHO; 2006.
- Pan American Health Organization-World Health Organization. Clasificación Estadística Internacional de enfermedades. 9th ed. 1975;1(353):57- 62.
- Pan American Health Organization-World Health Organization. Clasificación Estadística Internacional de enfermedades y problemas relacionados con la salud. 10th ed. 1995;2(554):29-48.
- National Statistics Bureau (CU). Capítulo XV – Salud Pública y Asistencia Social. [cited 2008 July 31]. Available from: www.one.cu/aec2006/ aec2006indicec15.htm
- Jenicek M, Cléroux R. Epidemiología. Principios. Técnicas. Aplicaciones. Madrid: Salvat SA;1988.
- Ahlbom A, Novell S. Fundamentos de Epidemiología. Madrid: Siglo XXI de España. SA;1988.
- Ministry of Economics and Planning (CU) [Internet]. [cited 2008 August 1]. Available from: http:// www.cubagob.cu
- Ríos NE, Tejeiro A. Evolución de la mortalidad en Cuba analizando un trienio de cada periodo revolucionario. Rev Cubana Med Gen Integr.1987;3Suppl:S29-89.
- World Health Organization. Global tuberculosis database. Powered by The Global Health Atlas: [cited 2008 February 20]. Available from: http:// www.who.int/globalatlas/autologin/TB_login.asp
- Raviglione MC, Zinder DE, Kochi A. Global Epidemiology of Tuberculosis. JAMA. 1995;273:220-5.
- Dolin P, Raviglione MG, Kochi A. Global tuberculosis incidence and mortality during 1990- 2000. Bull WHO. 1994;72:213-20.
- Dye C, Watt CJ, Bleed DM, Mehran Hosseini S, Raviglione MC. Evolution of tuberculosis control and prospects for reducing tuberculosis incidence, prevalence, and deaths globally. JAMA. 2005;293:2767-75.
- Dye C. Global epidemiology of tuberculosis. Lancet. 2006;367:938-40.
- Pérez J, Pérez D, González I, Díaz M, Orta M, Aragonés C. Approaches to the management of HIV/AIDS in Cuba: case study. Perspectives and practices in antiretroviral treatment. Geneva: WHO; 2004.
- Montoro E, Lemus D, Echemendía M, Armas L, González E, Llanes MJ, et al. Drug-resistant tuberculosis in Cuba. Results of the three global projects. Tuberculosis. 2006;86:319-23.
- Schneider E, Moore M, Castro KG. Epidemiology of tuberculosis in the United States. Clin Chest Med. 2005;26:183-95.
- Kim YJ, Pack KM, Jeong E, Na JO, Oh YM, Lee SD, et al. Pulmonary tuberculosis with acute respiratory failure in South Korea. Eur Respir J. [serial on the internet]. 2008 Jul 24. [cited 2008 July 31]. Available from: http://erj.ersjournals.com/cgi/content/abstract /09031936.00070907v2
- Nájera JC, Sánchez HJ, Ochoa H, Arana M, Salazar MA, Martín M. Demographic, health services and socio-economic factors associated with pulmonary tuberculosis mortality in Los Altos Region of Chiapas, Mexico. Int J Epidem. 2008;37(4):786-95.
- Sabetay C, Enache D, Plesea E, Zaharia B, Stoica A, Rosca A, et al. Intestinal tuberculosis in children. Differential diagnosis and treatment. Chirurgia (Bucarest). 2000;95:179-91.
- Saraceni V, King BS, Cavalcante SC, Golub JE, Lauria LM, Moulton LH, et al. Tuberculosis as primary cause of death among AIDS cases in Rio de Janeiro, Brazil. Int J Tuberc Lung Dis. 2008 Jul;12(7):769-72.
- González OY, Adams G, Teeter LD, Bui TT, Musser JM, Graviss EA. Extra-pulmonary manifestations in a large metropolitan area with a low incidence of tuberculosis. Int J Tuberc Lung Dis. 2003;7:1178-85.
- Cagatay AA, Caliskan Y, Aksoz S, Gulec L, Kucukoglu S, Cagatay Y, et al. Extrapulmonary tuberculosis in immunocompetent adults. Scand J Infect Dis. 2004;36:799-806.
- Hoshino H, Ohmori M, Uchimura K, Yamauchi Y. TB epidemiology in an elderly group in Japan. Kekkaku. 2008;83(5):423-9.
- Tocque K, Convrey RP, Bellis MA, Beeching NJ, Davies PD. Elevated mortality following diagnosis with a treatable disease: tuberculosis. Int J Tuberc Lung Dis. 2005;9:797-802.
- Hansel NN, Merriman B, Haponik EF, Diette GB. Hospitalizations for tuberculosis in the United States in 2000: predictors of in-hospital mortality. Chest. 2004;126:1079-86.
- Palomino JC, Leão S, Ritacco V. Tuberculosis 2007. From basic science to patient care. 1st ed. [monograph on the internet]. [cited 2008 February 20]. Available from: www.TuberculosisTextbook.com
- Abreu G, González E, Armas L, D’Fana J, Borroto A, Llanes MJ, et al. Tuberculosis en niños de 0-14 años. Cuba, 1994-2003. A Pediatr (Barc). 2007;66(3):248-53.
- Marais BJ, Gie RP, Schaaf HS, Hesseling AC, Obihara CC, Nelson LJ, et al. The clinical epidemiology of childhood pulmonary tuberculosis: a critical review of literature from the pre-chemotherapy era. Int J Tuberc Lung Dis. 2004;8:278-85.
- Adams LV. Childhood tuberculosis in the developing world. Pediatr Ann. 2004;33:685-90.
- Gisselbrecht M. Tuberculosis in elderly persons living in institutions. Rev Mal Respir. 2004;21(5 Pt 3):8S106-13.
- Lubart E, Lidgi M, Leibovitz A, Rabinovitz C, Segal R. Mortality of patients hospitalized for active tuberculosis in Israel. Isr Med Assoc J. 2007 Dec;9(12):870-3.
- Franco J, Blanquer R. Mortality for tuberculosis in Spain from 1970 to 1993: changes in epidemiological trends during the acquired immunedeficiency syndrome epidemic. Int J Tuberc Lung Dis. 1998;2:663-9.
- Menzies D. Tuberculosis in big cities. The urban factor in tuberculosis. Conference on Global Health and the 1996 Annual Meeting of the IUATLD. Paris, France. 2-5 October 1996. Tuber Lung Dis. 1996;77 Suppl 2:S16.
THE AUTHORS
Edilberto González Ochoa (Corresponding Author: ochoa@ipk.sld.cu), epidemiologist. Senior researcher and consulting professor, Pedro Kourí Institute of Tropical Medicine, Havana, Cuba.
Grisel E. Risco Oliva, epidemiologist, master’s degree in entomology. Municipal Hygiene and Epidemiology Center, Regla Municipality, Havana, Cuba.
Susana Borroto Gutiérrez, family medicine specialist, master’s degree in epidemiology. Pedro Kourí Institute of Tropical Medicine, Havana, Cuba.
Abel Perna González, biostatistician. National Statistics Division, Ministry of Public Health, Havana, Cuba.
Luisa Armas Pérez, pulmonologist. Adjunct researcher and adjunct consulting professor, Pedro Kourí Institute of Tropical Medicine, Havana, Cuba.
Submitted: March 3, 2008 Approved: October 13, 2008