Dr Yamila de Armas has occupied an array of posts since finishing her residency in family medicine in her home province of Cienfuegos in 1992. She has served as a family doctor; polyclinic, municipal and provincial health director; medical school dean; and twice vice minister of public health. But few would doubt her toughest job is the one she has now: deputy director of the Havana City Provincial Health Department, in charge of medical services for the 2.2 million people living in Cuba’s complex, sprawling capital. It was here in 2002-2003 that the program was launched to repair, refurbish and expand the country’s nearly 500 community polyclinics. Key to the effort was equipping these facilities with a broader range of new and upgraded medical technology. Dr de Armas offers MEDICC Review her reflections on the results five years later.
Dr Yamila de Armas has occupied an array of posts since finishing her residency in family medicine in her home province of Cienfuegos in 1992. She has served as a family doctor; polyclinic, municipal and provincial health director; medical school dean; and twice vice minister of public health. But few would doubt her toughest job is the one she has now: deputy director of the Havana City Provincial Health Department, in charge of medical services for the 2.2 million people living in Cuba’s complex, sprawling capital. It was here in 2002-2003 that the program was launched to repair, refurbish and expand the country’s nearly 500 community polyclinics. Key to the effort was equipping these facilities with a broader range of new and upgraded medical technology. Dr de Armas offers MEDICC Review her reflections on the results five years later.
MEDICC Review: Why were the polyclinics selected for technology upgrading?
Yamila de Armas: We’ve always considered strong primary care the foundation of the health system-universal, accessible primary care providing prevention, early detection and follow-up of the majority of health problems that families and individuals face in their community. The polyclinic is the backbone of primary care and of our health system as a whole. Since the 1960s, we have kept working on its design, adapting the model to changing needs and circumstances. A local polyclinic now serves an average of 20,000 to 40,000 people living in a given geographic area. It also acts as a hub for a network of family doctor-and-nurse offices, which refer patients to the polyclinic for particular services or to see other medical specialists. And polyclinic physicians also refer patients to hospitals.
After we emerged from the very difficult economic times of the 1990s, it was obvious that our health services’ sustainability depended on revitalization and strengthening of the polyclinics-not just repairs, remodeling and new equipment, but also the transfer of medical technology that in many cases had been available only at the hospital level.
This was a major change. The idea was to make a range of diagnostic and other services more accessible to people by bringing them closer to home, and also to train more professionals and health workers to make use of the technology. Today, each of Havana’s 82 polyclinics offers a set of 24 essential services and 22 medical specialties. A number of polyclinics have additional services, depending on their location and on the epidemiological profile of the population in their catchment area. (See Reed G. Changes to Cuban Health Care Aim to Extend Equity. MEDICC Review. 2005;7(9):5-7.)
MEDICC Review: Why start with Havana?
Yamila de Armas: Havana was the obvious place to start the national program, since it is the most densely populated metropolitan area in the country and has the most social problems. Thus, starting here would have the most immediate impact on a large population base. By now, of course, all polyclinics across the country have been included. This has brought about a change not only in tangible resources, such as equipment and laboratory processes, but also in intangible ones, such as the organization of services. The aim is to empower the polyclinics to address as many health issues as possible at the primary care level.
MEDICC Review: What were the main investments, and what changes did they make in patient care?
Yamila de Armas: Urgent care facilities, for one. Of the 15 municipalities in Havana City province, we selected ten in which one polyclinic would host a Municipal Intensive Care Unit. We chose the municipalities furthest from hospitals. These units were outfitted with new life support equipment, such as ventilators, and staffed by intensive care physicians and nurses. New ambulances were brought into all municipalities to replace the old ones, which were quite deteriorated, and we re-organized the ambulance dispatch system.
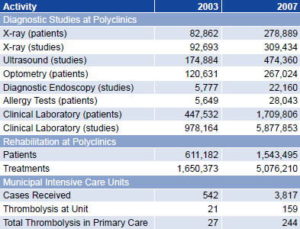
At the same time, the 24-hour emergency services at all 82 polyclinics were expanded, adding vital support cubicles and more observation beds. These services were buttressed by the polyclinic’s enhanced laboratory and imaging services that were part of the overall upgrade. We also introduced thrombolysis for heart attack victims in all polyclinics, using Cuban recombinant streptokinase. These changes are now bearing results: for example, we have brought the ambulance rescue time to under 15 minutes for heart-attack, stroke and trauma patients. And in 2007, 244 people received thrombolysis at the primary care level, nearly ten times more than in 2003 (Table 1).
X-ray and ultrasound equipment were upgraded, and most preoperative and pre-hospitalization studies, including contrast studies, can now be performed at all polyclinics. The clinical laboratories can now carry out a wider range of tests, including nearly all hemochemical studies, and a number of polyclinics have allergy-testing services too. Finally, the transfer of technology has introduced new services, such as optometry and minor surgery, as well as physical and psychological rehabilitation.
As you can imagine, these changes required major organizational and personnel shifts, and more training. We’ve worked hard to offer additional training to family physicians in specific areas, and also to train new technical staff for the polyclinics. Looked at another way, the new equipment and patient services have enhanced the polyclinic as a teaching facility for the medical, nursing and allied health students based there. (See Morales, I et al. Cuban Medical Education: Aiming for the Six-Star Doctor. MEDICC Review. 2008;10(4):5-9.)
Table 1: Impact of New Technologies in Havana City Province Primary Health Care Units, 2003 to 2007
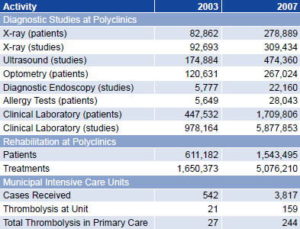
Source: Provincial Public Health Department, Havana City Province, December 2008.
MEDICC Review: You mentioned that specialists in 22 fields also see patients at the polyclinics. How does that work, and what part does the new technology play?
Yamila de Armas: In addition to the specialists based at the polyclinics-such as those in pediatrics, internal medicine and ob-gyn-a number of hospital-based specialists rotate through on a regular basis for patient consultations, teaching, and to provide various treatments. In other words, instead of the patient going to the hospital, the hospital doctor goes to the polyclinic.
The idea is comprehensive care. The family doctor and nurse are still the first line of care. At the same time, continuity is provided by the other specialists and the services offered at the polyclinic.
Let’s take a hypertensive patient. A bit overweight, a smoker. It would have been ideal if we had managed to prevent this person from smoking or gaining too much weight in the first place. But let’s say we didn’t win that battle.
The polyclinic now has a smokers’ clinic to help him stop, a nutritional counselor to help him with diet. But again, let’s say he nevertheless becomes hypertensive. His family doctor and nurse have all the diagnostic tools at their disposal for an early diagnosis, treatment and follow-up. He can be seen by a cardiologist at the polyclinic, where he can have further studies done and also be educated about his condition. And if he should have complications, such as a heart attack, the local emergency system responds, offering thrombolysis if it’s warranted.
He goes to the hospital, and when he’s released, he receives cardiovascular rehabilitation and follow-up in his community once again. Before, the polyclinics couldn’t do all this. Now they can. We are working to close the circle-from health promotion and prevention of disease, to early diagnosis, treatment and rehabilitation. So, it’s not the patients who circulate through the system, but the system that prioritizes patient-centered care at the polyclinics.
MEDICC Review: Challenges ahead?
Yamila de Armas: We’re closely monitoring process and results indicators, including numbers of patient consultations, treatments, diagnostic studies, and the flow of patients between hospitals and polyclinics. We’re assessing final impact on health outcomes, mortality and patient satisfaction. We’re also measuring human resource indicators related to quality of care, such as the number of health professionals in primary care, years of experience in their fields, etc.
Thus far, we see that the number of outpatient consultations with specialists at the polyclinics is growing. These are the same specialists that patients used to see at the hospital (Table 2). This speaks to patient confidence in the process and also proves that services are, in fact, more accessible. We have also found a greater proportion of patients-particularly hypertensives and diabetics-whose chronic diseases are under control and thus have not resulted in complications.
Table 2: Outpatient Consultations in Selected Specialties. Havana City Province Primary Health Care Units, 2003 to 2007

Source: Provincial Public Health Department, Havana City Province, December 2008.
The polyclinic needs to be continually strengthened to respond to new situations and needs. Our population is aging, and this has multiple implications, not just for medical services and technologies, but for society as a whole in terms of consciousness and the culture we need to develop in order to deal with aging. This presents us with a challenge to better integrate our health care services to effectively improve quality of life for older adults, not just to prolong their lives. This, in turn, requires a comprehensive approach.
At the polyclinics, we have multidisciplinary teams of social workers, family nurses, internists, geriatricians, and others devoted to providing integral care to older adults. In addition to medical services, these teams facilitate dental prostheses, offer family and personal counseling, assist with disabilities, and help solve social problems. This work will need to be strengthened and developed as we go forward.
Overall, our first priority is patient satisfaction: to improve the organization of all services at the primary care level, improve their effectiveness and bring them closer to people. We’ve revolutionized what we had, but we still have a ways to go to meet people’s needs with optimum, quality care.