MEDICC Review: Looking back on Forum 2009, how would you assess its particular contribution?
Niviola Cabrera: I think it will be remembered for focusing on social as well as technological innovation and the importance of integrating the two for better and more equitably distributed health outcomes. We’re accustomed to hearing of research and innovation regarding tangible technologies—which receive more global funding—but historically, we haven’t heard as much about the intangibles of social and organizational innovation. Or about the need to combine the two.
Seeing what Cuba is doing along these lines was one of the benefits of holding the 2009 Forum in Havana. It enabled local health professionals to present on topics such as public health applications of developing-country biotech research, and allowed participants a first-hand look at our efforts to generate more effective, equitable healthcare strategies and better services.
MEDICC Review: Your division oversees research and innovation in health: how are research priorities set?
Niviola Cabrera: In a country like ours, where resources are scarce, we can’t afford to carry out research for the sake of science alone: we have to use it to solve our most pressing population health problems and improve the quality of healthcare. Take maternal mortality, for instance. We’re not at all satisfied with the rates we have achieved [46.9 per 100,000 live births in Cuba, compared to 87.6 in Latin America and <10 in Canada, Eds.] Research needs to tell us more, to pinpoint where the problems lie. So, this line of investigation is a top priority. Our role—the role of researchers—is to provide scientific evidence that tells decision-makers what is happening and why, so they can act.
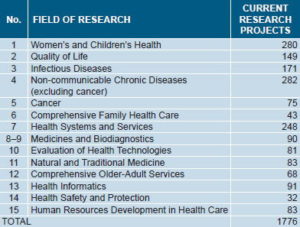
One resource we have in abundance is trained scientists, over 1900 in the health system qualified as researchers by the Ministry of Science, Technology and the Environment (CITMA, its Spanish acronym). By agreement with CITMA, the Ministry of Public Health is responsible for developing research programs in 15 fields, such as women’s and children’s health, quality of life, infectious diseases, chronic non-communicable diseases, and so on. [See box for full list, Eds.]
After rigorous assessment, some 48 health institutions have been accredited as Science and Technological Innovation Units, including high-level research facilities, medical sciences universities, pharmaceutical plants, hospitals and community polyclinics. One Unit takes the lead in research within a particular field, although projects can be formulated and pursued by other institutions. Each project needs approval by the scientific and ethics committees of the principal investigator’s institution plus the recommendation of a panel of three outside experts, who judge the project on the basis of relevance, potential impact of results, and feasibility.
MEDICC Review: Let’s return to the big picture of priority setting. Where do you begin?
Niviola Cabrera: That’s an interesting question, because our starting point has changed. Before 2009, priorities were developed at the top, and then handed down; but last year, we decided to turn this process on its head and begin at the local level. We carried out a national exercise beginning in the municipalities, then extended it to the provincial and national levels. Our objective was to identify the most important health problems, felt needs, that required research and innovation. We started with the epidemiological profile of each municipality and province, and then discussed all aspects of health status, services, and social determinants, until we reached a consensus.
The seven-month process involved physicians, nurses, psychologists, sociologists, dentists, health technologists, engineers, and educators, among others, who were all involved in the health system at various levels. Making the process more participatory has also made it more scientific. The opening question we asked was: ‘What health problems merit research, the results of which could enrich practice and contribute to partial or total solutions?’ Through a methodology that allowed us to evaluate the magnitude and severity of each problem, as well as the capacity of research to help solve it and the feasibility of the research itself, we were able to generate the top priorities for study in each territory.
This last is important since health problems are, of course, different in different communities, municipalities, and provinces. For example, cancer has been on the increase, particularly in the country’s eastern provinces in the past few years. Infant and maternal mortality are not homogeneous, etc. The “bottom-up” methodology allowed us to dig deeper in each locale, and to plan research to achieve greater equity in distribution of resources and services.
On a national level, this exercise revealed the most pressing problems, and thus the priority lines of research in the 15 fields I mentioned above—our compass. I should add the caveat that Cuba’s health indicators overall are quite good, especially when compared to other developing countries, so “high” prevalence for us may be “low” prevalence for another country. It is a matter of keeping a watchful eye on trends, of not being satisfied, and working within our own context, which challenges us to do better. [See box for priority lines of research identified, Eds.]
MEDICC Review: How do you take the difficult step from research results to changes in policy or health strategies? Is the voice of researchers heard?
Niviola Cabrera: Change is never easy, especially when it implies changes in strategies or in the way people do things on a daily basis. The Minister [of Public Health] has been especially insistent that research results be incorporated into every new decision, for the sake of the health system’s development. But of course, not everyone at all levels sees this so clearly.
When research findings come in, they are presented at the top level of the Ministry if they require national action. For example, back in 2006, our national cancer program was completely overhauled, with the creation of a new National Cancer Unit, as a result of a series of studies indicating where the problems were and why we weren’t getting the results we wanted. That’s one example of a major shift in policy.

In general, the institutions obtaining research findings present them at the national, provincial or local level, with recommendations for change in strategy or practice. Once again, taking the example of cancer, the results of 51 research projects recently came in and were presented with recommendations directly to the Minister, and another 81 are due shortly. It’s worth noting that, in the process, we also discovered that we don’t have enough evidence in some areas to act. For example, we have good evidence on incidence and mortality trends but insufficient evidence about risk factors or quality-of-life measures for cancer survivors; we have enough knowledge base in technologies used in interventions but not enough to evaluate the quality of their application nor the “intangibles” of the organization of cancer care.
Once results are presented, then the recommendations are considered and evaluated, bringing in other opinions. I think key to the whole process is the scientific reputation of the institutions doing the research; sound research methodology; and integration of researchers from both inside and outside the health system to involve them in solving serious health problems.
MEDICC Review: Are there research strategies that the Cuban health system has found particularly effective or useful?
Niviola Cabrera: Yes, especially action research strategies. That is, research that is broad and population-based, and that goes beyond diagnosing a health problem, or in the case of individuals, their particular set of health problems. Incorporated into the research strategy are actions to achieve more immediate transformation of outcomes, and not only in health.
One example is the national disabilities study, conducted from 2001 to 2003, that involved over 30,000 health professionals, including some 11,000 family doctors and 3,000 family nurses, as well as specialists in other fields. Over 226,000 Cubans with disabilities were studied—not only their health situation and specific problem, but also their social situation, their housing conditions, whether they were in school or working, how their family was coping, and what genetic factors were present. This resulted in more immediate solutions to many of their problems than would have been possible applying another kind of research; it also resulted in changes in strategies over the longer term in many sectors influencing the wellbeing of Cubans with disabilities.
The same research paradigm has been applied to several studies of chronic diseases.
MEDICC Review: Where are the major gaps in health and medical research today in Cuba?
Niviola Cabrera: I would identify three: first, our epidemiological research often yields a description of the problem but lacks the necessary design complexity to give us information on cause and effect, to tell us whether our programs are being successful. We also need to incorporate more social scientists into research, especially for qualitative research on such vital issues as quality of life. It’s not enough to know that people live a certain lifestyle; we need to know why. We need to know more not just about risk, but about social and cultural factors that protect health.
Finally, basic research facilities still feeling the effects of the economic crisis of the 1990s, and investigations in this field have been significantly reduced. This is a serious problem for the future, and thus recovering and enhancing basic research capacities are priorities at the national level over the next five years.
MEDICC Review: How do you see a research agenda in the context of South-South cooperation?
Niviola Cabrera: South-South cooperation has tremendous importance for us, and the Global Forum has served as a platform to increase collaboration in key areas. Right now, a number of our scientists are heading to Brazil, as a result of a proposal at the Forum, to increase cooperation in applying biotechnology to major health problems in both countries.
Research is vital to all our global cooperation—from evaluating human resources training and the results of the vision restoration program (Operación Milagro), to assistance establishing statistical records’ systems in other Third World countries. This last is critical for many of the African nations with which we have cooperation agreements.
We’ve also found that research methodologies are more easily adapted from one developing country to another. For example, the design of the chronic vascular diseases study underway in total population on Cuba’s Isle of Youth (ISYS) is being adapted for rural El Salvador, which is facing an epidemic of renal disease among young men. The Cuban experience is proving valuable, as we’re able to transfer the technology in a way that is appropriate to a new context, guided by the Salvadoran health ministry.
The most important thing is that South-South cooperation offers an important route for countries to build their own capacities, to reinforce their health systems with new knowledge, and also benefit from vaccines and technologies formulated in developing countries like their own. The transfer of technologies, of know-how, and the more favorable intellectual property schemes among developing nations, help overcome important barriers to health for our countries, where the majority of the world’s people—and its poorest people—live.