ABSTRACT
Cuba’s public health system is well known for its integrated first line services based on family medicine. Less publicized is the country’s experience in public hospital management. After a harsh economic crisis in the first half of the 1990s had brought the Cienfuegos hospital near to collapse, from 1996 onwards the hospital management team took advantage of the incipient economic recovery to launch an ambitious recovery process. This article reconstructs this endeavor, based on annual hospital reports, scientific publications by the hospital staff, and interviews with key decision-makers.
First the endless waiting list for elective surgery was tackled through a more efficient use of the surgery department, and an increase of ambulatory surgery. Next, overall hospital efficiency was improved in the aim to drastically reduce the average length of stay, reaching a decrease from an average stay of 12 days to a little more than 6 days in 1999. Also the emergency department was reorganized, setting up a triage system based on a color code, linked to specific emergency protocols. Attention for improving the clinical efficiency for AMI and stroke coincided with a drop in their intrahospital lethality.
Clinical guidelines for the most important diagnoses were collectively developed, adapting international evidence to the local setting. An individual and collective performance evaluation system was elaborated in a participatory way, and further evolved into a ‘total quality management’ process.
This experience of Cienfuegos hospital provides an interesting example on how a public hospital – embedded in a well developed national public health system – can be effective and efficient, even in circumstances of limited resources.
Keywords Hospital management, public health system, health services organization, strategic planning, Cuba
1. Introduction
Defined by the United Nations Development Program (UNDP) as the decade of globalization [1], the 1990s showed a complex socio-economic evolution of the Latin-American and Caribbean (LAC) region, in which state reform and trade liberalization were omnipresent [2]. In most countries, market oriented reforms were also applied to the health sector [3,4,47]. Financial limitations and managerial problems within the public health sector have been used as triggers for privatization policies, claiming that private medical care offers better quality and efficiency, while alleviating national government budgets [5]. Meanwhile, strong evidence exists that these claims are ideologically biased [6,7].
In the past century, public health systems have had a decisive impact on the favorable evolution of the health status of populations in developing countries. While this need for a well developed public health system remains essential, since decades many public health institutions suffer from limited resources, but also poor management. The option to further develop rational planning and efficient management of the public sector – rather than privatizing health systems – has long time been marginalized within the international health policy debate.
Cuba is a noteworthy exception. Cuba, a small and singular nation in the LAC-region, was extremely hit by the breakdown of the Soviet Union, which led to a sudden reduction of the country’s foreign trade by almost 80% and a fall in gross national product (GNP) of 34% between 1989 and 1993. The United States reinforced the now almost 50-year economic blockade, deepening the suffering of the Cuban people [8].
Nevertheless, Cuba is well known to have been able to limit the social and health consequences of this dramatic period, with the health system playing a pivotal role [9,10]. At international level Cuba remains one of the notable exceptions of maintaining an exclusive public health system with a strong community oriented health services network and a well developed and quite effective primary care [11]. Ample bibliography exists by now on Cuba’s public health strategy of answering this crisis by the further development of its first line health services through full coverage of the population by family doctors and nurses, ensuring direct accessibility, free services and integrated care [12,13].
Less known – but definitely also important – is the Cuban experience in public hospital management. During the 1990s also the Cuban hospitals came under strain, and – not unlike the rest of society – had serious difficulties to cope with their function. The experience of the main public hospital of Cienfuegos provides interesting elements on how public services – embedded in a well developed national public health system – can cope with such socioeconomic constraints.
This article presents an analysis of the initiatives that were developed in the main hospital of the Cienfuegos province from 1996 onwards, taking the incipient socioeconomic recovery as an opportunity to improve the output of the hospital.
2. Method
2.1 The public hospital of Cienfuegos
The basic structure of the Cuban health system is the health area, covering about 30,000 inhabitants. Each area ensures all first line care. For this it can count on family doctors and nurses (1/800–1500 inhabitants) working in the neighborhoods, and supporting specialists and technical backstopping (X-rays, echography, gastroscopy, biomedical laboratory, etc.) in the policlinic (one per health area), where there is no ‘in-patient’ department. At the secondary level we find, on average, one referral hospital per 150,000 inhabitants. Finally, the tertiary level is composed by university hospitals and specialized institutes.
Fig. 1. Time line of management interventions in the public hospital of Cienfuegos, Cuba.
Cienfuegos, one of the smallest of Cuba’s provinces, is located in the center and south of the Island, with a population of 401,575 inhabitants in 2008. It has a relatively important industrial development, and plays an essential role in the actual relaunching of Cuba’s economy.
The General University Hospital Dr. Gustavo Aldereguia Lima (GAL) is the main hospital in the province, fulfilling at the same time the role of referral hospital and of tertiary care facility. It has services for medical and surgical disciplines, gynecology and obstetrics, and neonatal care. Today it has 640 beds, hospitalizing an average number of about 22,000 patients per year. They are taken care of by 512 medical doctors (including 162 residents), 906 nurses, and 408 technical staff. Currently some 150 of these health workers, mainly physicians, are on international mission abroad [14]. Moreover, the hospital is a main pre-grade training site for part of the thousands of Latin-American medical students in Cuba [15].
2.2 The managerial process
After its onset in 1989, Cuba’s harsh socio-economic crisis deepened over the first half of the nineties. This crisis had an important impact on the functioning of the hospital. The number of hospitalizations fell from 19,000 in 1988–1989 to less than 14,000 in 1994–1995. When in 1995 the country started a long period of slow economic recovery, the Cienfuegos hospital was near to collapse. The low resolution capacity produced prolonged hospital stays, leading to a strange combination of decreased numbers of hospitalizations and high occupancy rates in the 742 hospital beds. Moreover, the long waiting list for elective surgery, caused by financial and technological exhaustion, led to public and managerial desperation.
When in 1996 new hospital directives were appointed, they were confronted with staff demotivation, service disorganization and technical indiscipline, with growing public discontent as an inevitable consequence. A managerial team was set up to take the situation in hands, and to work out a recovery process. One of the authors (PO) was director of the hospital from 1996 onwards.
The main question was: where to start? How and with whom to initialize a transformation? Through a series of discussions with key local actors (hospital staff, community representatives and politicians), the management team identified the main challenges at that time, and a strategy was developed to revert the situation.
Soon, the strategic value of accurate and timely information for decision making was felt. In 1997, a computerized information system was introduced to guide the managerial process, and hospital staff was (re)trained in essential concepts of public health surveillance and epidemiology. Gradually this information system became a core piece of the hospital’s evidence based management strategy. This article analyses the rationale, the intervention process and the results of the different initiatives that were developed (see the timeline in Fig. 1).
2.3 Research methodology
The reconstruction of the managerial process is based on three complementary sources. First, a review of the annual hospital reports over the period 1996–2008. Second, a series of national and international publications by the hospital staff over the period under study, in which specific items of the process have been developed. Third, unstructured interviews with key decision-makers in the hospital, to ensure the understanding of the rationale and the difficulties that had to be overcome.
Organizational interventions are described and their impact is analyzed. For two key health problems – acute myocardial infarction and stroke – outcomes in terms of hospital mortality are added. Finally, emphasis is put on the process of introducing a system of individual and collective performance evaluation and its evolution towards a total quality management process.
3. Results
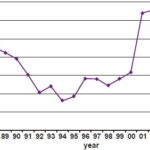
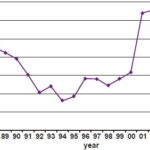
The number of hospitalizations (Fig. 2) gives a clear account of the overall functioning of Cienfuegos hospital between 1987 and 2006. From 1989 onwards, i.e. the onset of the crisis, a sharp decrease is observed. During the bottom years of the crisis 1992–1995 the lowest number of hospitalizations is observed. In 1996, the incipient economic recovery coincides with the start of the managerial initiatives at the hospital. The sharp increase in hospitalizations from 2001 onwards is due to the fusion with the Cienfuegos maternal hospital in the same facilities.
3.1 1996: waiting list for elective surgery
Since the onset of the economic crisis, due to an increasing lack of essential surgical equipment and supplies, the number of surgical interventions had been diminishing year after year. Endless waiting lists for elective surgery arose. These were identified as an important public health problem, and a cause of major anxiety and dissatisfaction in the population and among the hospital staff. If technical and organizational challenges to solve this problem could be overcome, results would be visible in the short run and would ensure support among staff and public for further managerial action.
Fig. 2. Number of hospitalizations per year (Cienfuegos Hospital, 1987–2006).
In consultation with the hospital surgery staff, it was proposed to reach – in the shortest time possible – the same productivity as in 1989, i.e. before the onset of the crisis. This objective was accepted as challenging but realistic. In a second phase, as the need for surgical interventions in a defined population remains quite stable overtime, overall surgical needs were estimated and a surgery ‘production’ plan was developed. By grouping interventions of the same type and optimizing working time for doctors and nurses the functioning of the surgery unit was reorganized to ensure its optimal use during the day. Existing material needs were tackled through a better planning process and a slightly increased hospital budget.
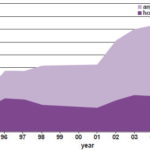
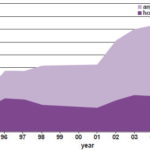
Moreover, adopting and adapting the international recommendations for ambulatory surgery, a growing part of the interventions was realized without hospitalization. Thanks to new surgical techniques, improved anesthetic agents and practices, and better managed ambulatory surgical facilities, ambulatory surgery is now possible for a whole series of interventions that do not require mayor post-operative care [16]. In Cienfuegos hospital, the use of ambulatory techniques increased from about 40% of the surgical interventions in 1995 to near to 80% in 2007. This evolution was coordinated with the first line health services, as the increase of ambulatory surgery had to be combined with an adequate follow-up of these patients by the family doctors.
Fig. 3 shows the evolution of the number of surgical interventions in the hospital from 1987 until 2008. During the bottom years of 1993–1995, about 6000 interventions were realized. In 1996, an increase to almost 10,000 interventions is observed. The further increase to 15,000 and more interventions from 2002 onwards, was mainly the consequence of the inclusion of gynecological interventions, following the integration of the maternal hospital in the same facilities. These overall figures prove the strategy to be sustainable over time.
3.2 Cutting the length of stay
Over the same period another essential intervention was developed to increase hospital efficiency and the adequate use of limited resources: the reduction of the length of stay in all hospital services. Besides the increase of ambulatory surgery, the main strategy was directed towards an improvement of the resolution capacity through a more efficient case management, avoiding all unnecessary waiting time during diagnostic procedures and between diagnosis and intervention.
The average length of stay of 12 days during the crisis years was brought back to a little more than 6 days in 1999. As a consequence, the number of hospital beds could be reduced from 742 in 1996 to 500 in 1999. This reduction paved the way to a fusion with the Cienfuegos maternal hospital in 2001. This hospital was located in an old and exhausted building, and its absorption led to a general hospital with a total capacity of 640 beds today, including 150 maternal and 30 neonatal beds [17].
3.3 Reorganizing the emergency department
During 1998, emergency care was at the centre of the attention. As in so many countries, the emergency department of the Cienfuegos hospital suffered from serious congestion. While the Ministry of Health tried to diminish the pressure on the hospitals implementing a national program to improve emergency care at to the first line [18], the Cienfuegos hospital staff was also looking how to improve efficiency at its emergency department.
A new classification system was organized, based on a color code for incoming emergencies: red for emergencies, yellow for medical need, green for referral to the family doctor. As specific emergency protocols were developed, this triage system ensured a much better patient flow in the emergency service. It was further improved by the introduction of a spatial division of the emergency quarters in a yellow and a red zone. This new intervention made the patient satisfaction and the general population’s view on the hospital change dramatically [19].
The process of developing clinical efficiency for emergencies was linked to the revision of strategies in case of (natural and manmade) disasters. Interventions were directed to improve the reception and care of accidents in which many persons are involved. Based on international principles regular exercises were organized with all involved services [20,21]. Shortcomings were tackled through the development of an alert and mobilization plan, through the specification of clear procedures for each of the teams, linked to a better mobilization of the available human resources and a standardization of tasks for all, while also training was provided [22–24].
Fig. 3. Proportion of ambulatory surgery in the Cienfuegos hospital (1995–2006).
3.4 Reviewing clinical efficiency for AMI and stroke
From 1999 onwards, an initiative was set up to improve clinical efficiency for important acute and life threatening health problems: acute myocardial infarction (AMI) and stroke.
Like in most countries, also in Cuba cardiovascular disease is a peaking cause of death [25]. In Cienfuegos province, the number of hospital admissions for AMI doubled over the period 1990–2003. Knowing that – for poor resource countries like Cuba – angioplasty is not a realistic option, the efficiency of thrombolysis as a first choice emergency intervention was tested, using nationally produced Streptokinase.
A strategy at the first care level to improve timely hospital admission for AMI was combined with better emergency care in the hospital. The thrombolytic treatment unit was transferred from the intensive care unit (3rd floor) to the emergency service. In AMI patients with ST elevation arriving at the hospital, an overall thrombolysis rate of over 60% was reached, with a “door to needle” time of 30 min for more than 90% of them [26,27]. Results had an impact on national policy. Trombolysis is now the standard treatment in Cuba and became widely available. Besides its use in hospital emergency departments, the creation of pre-hospital treatment units in each municipality has reinforced its impact [28].
This emergency treatment of AMI further led to an overall reorganization of the intensive cardiologic care strategy. Until then, patients with serious cardiologic problems as AMI were assisted in a ‘classic’ intensive care unit (ICU), where they consisted about 25% of all ICU-patients. Once their condition improved, they were translated to a medium care unit (MCU), and afterwards to the cardiology service to complete the evaluation and rehabilitation [29,30].
From 2001 onwards, intensive care services were reorganized with the opening of a cardiologic intensive care unit (CICU), which ensure a continuous and homogeneous MCI-care in all phases [27]. This new setting was beneficial by obtaining a reduction on mortality after intervention of 7.9% (26.9% vs. 19.0%, p =0.03) which in absolute figures meant 20 more survivors [31].
Following the lessons learnt from the approach to AMI, in 2001 a comparable approach was also implemented for stroke, the third cause of death in Cuba [25]. The ‘fast track’ approach for stroke can be summarized into 10 components all starting with the word “early”: awareness of the warning signs, medical contact, life support, referral, treatment in the emergency department, brain imaging, admission to the stroke unit, rehabilitation, education for patients and carers, and secondary prevention.
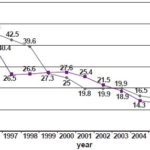
Fig. 4 gives an overview of the intrahospital lethality for AMI and stroke between 1995 and 2007. The start of the overall managerial process (1996) coincides with a first moment of decreasing lethality. The process of enhancing the clinical efficiency for AMI (1999) and stroke (2001) are also accompanied by a decrease in intrahospital lethality.
Fig. 4. Intrahospital letality by acute miocardial infarction and stroke (Cienfuegos, 1995–2007).
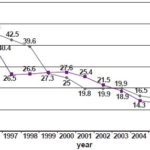
For both AMI and stroke, the changing case mix as a consequence of greater general awareness and earlier hospital admission, makes it difficult to evaluate the evolution of intrahospital mortality. Case fatality rate for coronary hearth disease declined by 40–50% between 1990 and 2003. While over the same period admission rates for stroke doubled in Cienfuegos hospital, case fatality rates fell with 48% [25,32,33]. These results might suggest that less severe cases were admitted, explaining at least part of the mortality reduction. Morbidity and mortality trends should be understood as a combined consequence of an increasing average age of the population, an earlier admittance to the hospital, and better quality of care [28,25].
3.5 Clinical guidelines and surveillance
A process of developing ‘guidelines to clinical practice’ was started over 1999–2000. Using the well known Japanese managerial technique of ‘quality circles’, a task force was set up to produce, socialize and assess the most important clinical guidelines [34]. All important health problems were tackled (in terms of frequency, severity, vulnerability, financial feasibility, public health need and public demand): pneumonia, AMI, stroke, appendicitis, ectopic pregnancy, etc.
In the local context of limited resources and (at the most) ‘suboptimal’ technological support, a conceptual approach towards evidence based clinical management was developed, applying the classical principles of clinical epidemiology of Feinstein [35], and the more novel concepts of evidence based medicine developed by Sacket [36]. The quality of the available data was improved through information standardization and continuous digitalized data collection. Collective fast track-analysis by the staff involved ensured an immediate discussion of the problems and proposals for solutions to improve clinical practice.
Step by step, clinical guidelines were collectively developed. For each topic a group of experts developed a proposal that was discussed and amended through a collective and participatory process with the whole staff. These guides were based on international evidence and adapted to the local setting. First its technical and organizational aspects were developed, after which administrative elements were added.
3.6 Individual and collective performance evaluation
From 2002 onwards all physicians, including specialists and professors, are evaluated on a yearly basis with a locally developed ‘performance evaluation’ method.
In a preparatory phase, 32 hospital health workers of different disciplines and levels and 21 staff members with (also) administrative responsibilities collectively designed a performance evaluation method, looking at working discipline, technical quality and results, ethics in human relation, learning attitude, creativity, etc. [37].
This individual evaluation is complemented by a comprehensive evaluation of the functioning of the hospital departments. Also here, the methodology was collectively developed through brainstorming sessions: by weighting the group’s ideas by successive approximations, ten factors were identified as indicators for the level of development of each department. Based on a self-evaluation by the head of department, a second evaluation by the corresponding deputy director and a third by an external expert, a conclusive report was developed. The tool is considered to be a useful, flexible, cheap and easy-to-apply instrument for evaluating medical departments [38].
Based on these two instruments, a yearly overall evaluation compares all services in the hospital, and within these services all personnel, with an overall quotation from A to D. All members know their anonymous ranking in their team. The combination of individual and collective evaluations leads to constructive discussions on how to improve service functioning.
3.7 Total quality management (TQM)
This performance evaluation process evolved towards the development of an overall quality policy, in which all aspects of the hospital process are analyzed. Emphasis was put not only on technical quality, but also on the perceived quality. Patient centeredness was (and is) continuously monitored by patient opinion polls. TQM-procedures were developed for optimizing vertical processes (e.g. how a hip fracture is received and treated, from entrance at the emergency door until leaving the hospital), for integrated processes (e.g. the functioning of the service of internal medicine), and for technical processes (e.g. evidence based use of antibiotics, adequate treatment of blood derivates, sterilization processes, etc.). Furthermore, an internal financial control system was set up to revise the financial efficiency of all hospital activities, comparing budget planning with service functioning and results.
This TQM also includes a global training program with in-service training, master’s courses, second specialization, PhD-programs, participation in university teaching, etc.
An overall quality plan is comprehensively monitored through quality circles. For example in surgery, besides the number of cases, emphasis is put on waiting time, intrahospital infections, patient satisfaction, etc. These circles exist for all aspects of the hospital care process: analysis of hospital mortality, the cesarean sections policy, peri-natal care, pharmaco-therapeutic safety, control and evaluation of the medical equipment, blood transfusion service, etc.
Through this quality management process the Cienfuegos hospital opted for the international ISO 9000 certification, which it has obtained for four hospital services: the intensive care unit, the neonatology intensive care unit, the centre for ophthalmologic surgery, and the office of user care.
4. Discussion
The Cienfuegos hospital management experience started in the very complex circumstances of incipient economic recovery of 1996. As financial resources would only slightly increase, the main challenge was to reach better results through efficiency gains.
A first step was to ensure a stable hospital management team that was decided to develop a process of developing technical quality and patient centeredness, taking the social commitment and technical mission of the hospital as a starting point.
The undertaken ‘step by step’ approach proved to be successful to ensure important quality improvements, even in a complex and resource limited situation. The first successes in strategic areas as elective surgery and the emergency services made further managerial initiatives receiving full support from staff and population.
The existence of an integrated public health system was a necessary condition. The main factor, for example, to explain the diminishing pressure on the emergency services is linked to the development of the first line. In 1987, Cienfuegos hospital attended some 250,000 emergency cases, while in 2003 that number had decreased to 70,000. This was only possible because of the development of Cuba’s family doctor program which – starting in 1985 – could cover 95% of the Cuban population in one decade.
The severe crisis did not stop this policy. To the contrary, the objective of ensuring the coverage of the whole Cuban population was accelerated [11]. At the same time, from 1996 onwards The Ministry of Health developed an overall policy to diminish unnecessary demand to hospital emergency services, through the setup of emergency services at the first line [39,40].
Also a campaign was launched to improve public conscience on the adequate use of emergency services, and on the importance of using family medicine as an entry point for non-urgent ailments. This focus on first line services has been essential to ensure sustainability of the overall health system in difficult times [41].
The shortening of the duration of hospital stays and the development of an ambitious ambulatory surgery program need an integrated system with an adequate coordination between the first line and the hospital. For this, the development of a ‘hospital at home’-program as part of the Cuban family medicine strategy, was pivotal [42,43].
More generally, timely interventions and follow-up at the first line are essential to ensure stable efficiency gains at the second line. The improved clinical efficiency strategy for AMI and stroke, for example, can only be effective if combined with a strategy to improve timely hospital admission for these ailments at the first care level.
This relation has been bidirectional. The experiences and results of the Cienfuegos hospital influenced the overall provincial health system management at the level of human resources management, quality development and efficiency gains.
Staff motivation, reinforced through collective decision making, was essential in this managerial process. To surmount the inertia of the profound crisis of the first half of the nineties, participatory methods were developed. Through a step by step approach the staff was convinced that even with very limited resources much can be done.
The disappearance of the waiting lists for surgery through the mobilizing the surgery department, triggered the clinicians to reorganize the emergency department. The results of the clinical management of AMI and stroke treatment played an important role in convincing hospital staff that overall clinical efficiency could drastically be improved.
The collective development of clinical guidelines resulted in a new managerial culture. Soon it became impossible to take whatever decision without direct involvement of the hospital staff. These collective procedures and the expectation that their implementation would ensure better hospital functioning boosted staff motivation.
This, in its turn, gave the necessary basis of mutual trust and confidence to develop the individual and collective evaluation system. References to global quality development through performance evaluation of medical services are scarce, but comparisons of overall hospital quality performance exist in the US, the UK and Spain [44–46].
For the Cuban public health system this type of evaluation of medical services is novel. In Cienfuegos it was widely accepted by evaluators and evaluates, as well by the trade unions and political organizations. The methodology allows the formulation of specific initiatives to continuously improve each department, according to its particular characteristics. This system of integrated and comprehensive evaluation has not been coupled to salary supplements.
5. Concluding Remarks
The experience of Cienfuegos confirms that a public hospital can be effective and efficient, even in circumstances of limited resources. At the same time it should be underlined that a hospital can only play its effective public health role when integrated in a well functioning public health system. The first line health services – and in the Cuban setting mainly the family doctors receiving technical backstopping from the policlinics – bear with the main health activities, from health promotion over prevention to cure and care, and develop a holistic and integrated approach to the patient and his/her family in their environment. In this context, a hospital can play its full role of second line facility in which patients with more severe ailments are been taken care of.
This experience might be a valuable reference for other initiatives to develop an evidence based decision making approach to improve public health management – at national, regional, local or institutional level – even in circumstances that have a less favorable national public health policy. It confirms that public health (care) models can be efficient – in function of ‘external efficiency’ of population health, not profits – if adequate managerial strategies are developed.
References

- UNDP. Human Development Report 2003. Millennium development goals: a compact among nations to end human poverty. UNDP. New York–Oxford: Oxford University Press; 2003.
- Navarro V. The worldwide class struggle. Monthly Review 2006;58(4). http://www.monthlyreview.org/0906navarro.php.
- Green D. Silent revolution. The rise and crisis of market economics in Latin America. New York: Monthly Review Press; 2003. ISBN:1-58367-091-2.
- De Vos P, De Ceukelaire W, Van der Stuyft P. Colombia and Cuba: contrasting models in Latin-American health sector reform. Tropical Medicine and International Health 2006;11:1604–12.
- World Bank. World development report 1993: investing in health. New York: World Bank; 1993.
- Iriart C, Merhy E, Waitzkin H. Managed care in Latin America: the new common sense in health policy reform. Social Science and Medicine 2001;52:1243–53.
- Hernandez M. Reforma sanitaria, equidad y derecho a la salud en Colombia. Cadernos de Saude Publica 2002;18:991–1001.
- Kuntz D. The politics of suffering: the impact of the U.S. embargo on the health of the Cuban people. International Journal of Health Services 1994;24(1):161–79.
- Cooper RS, Kennelly JF, Orduñez-García P. Health in Cuba. International Journal of Epidemiology 2006;35:817–24, doi:10.1093/ije/dyl175.
- Spiegel JM, Yassi A. Lessons from the margins of globalization: appreciating the Cuban health paradox. Journal of Public Health Policy 2004;25:85–110.
- De Vos P. Health report on Cuba. “No one left abandoned”: Cuba’s national health system since the 1959 revolution. International Journal of Health Services 2005;35:189–207.
- Franco M, Kennelly JF, Cooper RS, Orduñez-García P. La salud en Cuba y los Objetivos de Desarrollo del Milenio. Revista Panamericana de Salud Publica/Pan American Journal of Public Health 2007;21(4):239–350.
- Spiegel JM. Commentary: daring to learn from a good example and break the ‘Cuba taboo’. International Journal of Epidemiology 2006;35:825–6, doi:10.1093/ije/dyl144.
- De Vos P, De Ceukelaire W, Bonet M, Van der Stuyft P. Cuba’s international cooperation in health: an overview. International Journal of Health Services 2007;37:761–76.
- Hospital Universitario Dr. Gustavo Aldereguía Lima. Anuario Estadístico. Cienfuegos: Hospital Universitario Dr. Gustavo Aldereguía Lima; 2008. http://www.gal.sld.cu/.
- Davis JE. Ambulatory surgery: how far can we go? Medical Clinics of North America 1993;77(2):365–75.
- Cienfuegos Hospital. Annual report 2008. Cienfuegos: Cienfuegos Hospital; 2009.
- De Vos P, Murlá P, Rodriguez A, Bonet M, Más P, Van der Stuyft P. Shifting the demand for emergency care in Cuba’s health system. Social Science and Medicine 2005;60:609–16.
- Iraola MD, Ordúñez PO, Rojas O. Hay diferencias en la población que utiliza el servicio de urgencias hospitalario? Revista de Calidad Asistencial 2005;20(3):157–8.
- PAHO/OPS. Establecimiento de un sistema de atención a víctimas en masas. Washington, DC: OPS; 1996. p. 35–41.
- PAHO/OPS. Organización de los servicios de salud para situaciones de desastres. Washington DC: OPS; 1983. p. 37–73.
- Eastman AB. Blood in our streets. The status and evolution of trauma care systems. Archives of Surgery 1992;127:677–81.
- Hersche B, Wenker O. Principles of hospital disaster planning. Disaster Medicine 1998;1(2). http://www.ispub.com/ostia/index.php?xmlFilePath=journals/ijrdm/vol1n2/hosp.xml.
- Navarro-Machado VR, Rodriguez-Suarez G, Falcón-Hernández A, Orduñez-García PO, Iraola-Ferrar M. Atención de víctimas en masa. Propuesta de un sistema por tarjetas de funciones. Revista Cubana de Salud Pública 2001;27(1).
- Cooper RS, Ordúñez P, Iraola-Ferrer M, Bernal JL, Espinosa A. Cardiovascular disease and associated risk factors in Cuba: prospects for prevention and control. American Journal of Public Health 2006;96:94–101.
- Iraola MD, Valladares FJ, Álvarez FC, Nodal JR, Rodríguez B. Optimización del tratamiento médico en el infarto agudo de miocardio. Clínica Cardiovascular 2000;18:11–6.
- Iraola M, Ordúñez P, Alvarez F, Santos M, Valladares F, Rodríguez B, et al. Unidad de cuidados intensivos cardiológicos: impacto sobre la mortalidad por infarto agudo del miocardio. Mejora continua de la calidad. MOI 2002;2(4):23.
- Ordúñez-García P, Iraola-Ferrer M, La Rosa-Linares Y. Experience in Cuba shows optimizing thrombolysis may reduce death rates in poor countries. British Medical Journal 2005;330:1271–2.
- Álvarez Z, Iraola MD, Molina F, Barco V. Caracterización de la mortalidad en la unidad de cuidados intensivos. Año 1998. Revista de Cubana Medicina 2000;39:222–7.
- Iraola MD, Santana AA, Rodríguez B, Valladares FJ. Sobrevida en el infarto agudo del miocardio. Clínica Cardiovascular 2001;19(2):40–5.
- Falcón-Hernández A, Iraola-Ferrer MD, Valladares-Carvajal FJ, Ordúñez-García PO. Impacto de un nuevo servicio para la asistencia de enfermedades cardiovasculares agudas. Revista Cubana de Medicina Intensiva y Emergencias 2006;5(2):380–90.
- Ordúñez P, Bernal JL, Espinosa-Brito A, Silva LC, Cooper RS. Ethnicity, education and blood pressure in Cuba. American Journal of Epidemiology 2005;162:49–56.
- Orduñez-García PO, Iraola-Ferrer MD, Bembibre-Taboada R. Cuba: better care for stroke. British Medical Journal 2006;332:551, doi:10.1136/bmj.332.7540.551-a.
- Ishikawa K, Loftus JH. Introduction to quality control. 3rd ed. Tokyo: 3A Corporation; 1990.
- Feinstein AR. Clinical epidemiology. The arquitecture of clinical research. Philadelphia–Boston: WB Saunders Company; 1985.
- Sackett DL. Clinical epidemiology. What, who, and whither. Journal of Clinical Epidemiology 2002;55(12):1161–6.
- Alvarez-Li FC, Orduñez-García PO, Espinosa-Brito AD. Introducción de la evaluación del desempeño individual en un hospital cubano. Metodología y resultados. Revista de Calidad Asistencial 2006;21(2):101–9. http://www.doyma.es/.
- Espinosa-Brito AD, del Sol-Padrón LG, Álvarez-Li FC, Rocha-Hernández JF, Ordúñez-García PO. Introducción de la evaluación del grado de desarrollo de los servicios médicos en un hospital cubano. Metodología y resultados. Revista de Calidad Asistencial 2007;22(4):195–201. http://www.doyma.es.
- De Vos P, Murlá P, Rodriguez A, Bonet M, Más P, Van der Stuyft P. Shifting the demand for emergency care in Cuba’s health system. Social Science and Medicine 2005;60:609–16.
- De Vos P, Vanlerberghe V, Rodriguez A, García R, Bonet M, Van der Stuyft P. Uses of first line emergency services in Cuba. Health Policy 2008;85:94–104.
- Van der Stuyft P, De Vos P. La relación entre los niveles de atención constituye un determinante clave de la salud [electronic only]. Revista Cubana Salud Pública 2008;34(4):1–9. http://bvs.sld.cu/revistas/spu/vol34 4 08/spu14408.htm.
- Barroso Utra IM, García Fariñas A, Rodríguez Salvá A, De Vos P, Bonet Gorbea M, Van Der Stuyft P. El ingreso en el hogar y su costo directo en Cuba. Panamerican Journal of Public Health 2007;21:85–95.
- De Vos P, Barroso I, Rodríguez A, Bonet M, Van der Stuyft P. The functioning of the Cuban home hospitalization programme: a descriptive analysis. BMC Health Services Research 2007;7. http://www.biomedcentral.com/content/pdf/1472-6963-7-76.pdf.
- Solucient top hospitals. 100 top hospitals study results and information products; 2006. http://www.100tophospitals.com/reports/intro.asp.
- Neil DA, Clarke S, Oakley JG. Public reporting of individual surgeon performance information: United Kingdom developments and Australian issues. Medical Journal of Australia 2004;181:266–8.
- García-Eroles L, Illa C, Arias A, Casas M. Los Top 20 2000: objetivos, ventajas y limitaciones. Revista de Calidad Asistencial 2001;16:107–16.
- De Vos P, Dewitte H, Van der Stuyft P. Unhealthy European health policy. International Journal of Health Services 2004;34:255–69.
THE AUTHORS
Pol De Vos, Public Health Department, Institute of Tropical Medicine, Antwerpen, Belgium. Corresponding author at: Institute for Tropical Medicine, Department of Public Health, Nationalestraat 155, 2000 Antwerp, Belgium. Tel.: +32 3 247 62 85; fax: +32 3 247 62 58. E-mail address: pdevos@itg.be (P. De Vos).
Pedro Orduñez-García, General University Hospital Dr. Gusavo Aldereguia Lima, Cienfuegos, Cuba
Moisés Santos-Peña, General University Hospital Dr. Gusavo Aldereguia Lima, Cienfuegos, Cuba
Patrick Van der Stuyft, Public Health Department, Institute of Tropical Medicine, Antwerpen, Belgium