Helena J. Chapman MD MPH PhD, Luisa A. Armas-Pérez MD MS, Michael Lauzardo MDMS, Edilberto R. González-Ochoa MD PhD
ABSTRACT
Global efforts to eliminate tuberculosis by 2050 continue to challenge health systems. In countries with low reported tuberculosis incidence, such as the USA (3.1/100,000 population) and Cuba (6.9/100,000), differences in classification by income level and health systems’ overall organizational structure are evident. However, the two countries’ low tuberculosis incidence, geographic proximity, robust research capacity and shared health priority for tuberculosis elimination provide fertile territory to strengthen collaboration for tuberculosis control in clinical, laboratory and community settings. Two tuberculosis symposia in Cuba—one at the Cuba Salud Convention in 2015 and the other at the International Forum on Hygiene and Epidemiology in 2016—were instrumental in stimulating dialogue on continued efforts towards eliminating tuberculosis by 2050. In this article, we describe tuberculosis burden in the USA and Cuba, critically analyze strengths and challenges experienced in areas of low tuberculosis incidence and provide recommendations for future institutional collaboration to support tuberculosis elimination and improved population health.
KEYWORDS Tuberculosis/epidemiology, Mycobacterium tuberculosis, prevention, communicable disease control, disease eradication, disease elimination, international cooperation, Cuba, USA
INTRODUCTION
Globally, tuberculosis (TB) is the main infectious cause of death, with an estimated 10.4 million new cases and 1.7 million deaths in 2016.[1] An estimated one third of the world’s population has asymptomatic Mycobacterium tuberculosis infection.[1] Over the past decade, although advances in diagnosis and treatment access, availability and effectiveness have improved TB patient outcomes, there have been no major strides towards global TB elimination. Continued emphasis on understanding the influence of political and social determinants of health on physical, psychosocial and individual health of TB patients will be crucial for TB elimination.
Three biological and social challenges in M. tuberculosis control persist and hinder TB elimination. First, both multidrug-resistant TB (MDR-TB), defined as M. tuberculosis strains that are resistant to isoniazid and rifampicin, and extensively drug-resistant TB, defined as MDR-TB resistant to any fluoroquinolone (e.g., levofloxacin, moxifloxacin) and at least one of three injectable second-line drugs (amikacin, capreomycin, kanamycin), have challenged successful treatment regimen delivery and outcomes. This human-made phenomenon is attributed to inadequate treatment by health care providers and lack of patient adherence to treatment regimens. An estimated 490,000 new MDR-TB cases were reported in 2016.[1]
Second, persons diagnosed with latent tuberculosis infection (LTBI) have an increased risk of developing active TB (TB reactivation), with a 5%–10% lifetime risk.[2] One third of the world’s population is thought to harbor LTBI; it is from this pool of infected persons that active TB cases emerge. Mathematical models of TB elimination all point to the need to address LTBI in order to have any prospect of eliminating TB this century.[3]
Third, nosocomial spread of TB is also a major driver of TB transmission, especially to persons with immune deficiencies (e.g., HIV/AIDS) or living in impoverished and overcrowded conditions (e.g., displaced populations or refugees, residents of correctional facilities or homeless shelters). Such persons frequently experience social stigma or exclusion, stress and anxiety, and demonstrate reduced health-seeking behaviors.[4] Moreover, health care workers, who have increased occupational risk of M. tuberculosis exposure, may be employed in health institutions with poor TB infection control practices.
Despite these general challenges, low-incidence countries, characterized by TB incidence of <100 cases per million population, have sustained TB control efforts.[5] Pragmatically speaking, obstacles to TB elimination in low-incidence countries are primarily: a) limited government support, such as inadequate health budgets; b) frequent periodic TB outbreaks in vulnerable groups (e.g., in correctional facilities, homeless shelters, health institutions); and c) need for early identification of susceptible individuals with LTBI and at risk of developing active TB.[5] Rapid responses are essential to address these challenges and act promptly to mitigate TB outbreaks and disease propagation in the community.
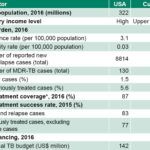
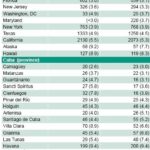
WHO reported 274,000 TB cases (27/100,000 population) in 2016 in the Americas Region.[1] Although the TB targets of the 2015 Millennium Development Goals were met, TB continues to be a major public health issue in Latin America and the Caribbean.[6] In 2016, two neighboring countries reported low TB incidence: USA (3.1/100,000 population) and Cuba (6.9/100,000 population).[7] Yet, although these two countries are in the TB pre-elimination stage (<10 TB cases per million population/year), further progress will be required to reach TB elimination (<1 TB case per million).[8] While the USA and Cuba differ in terms of total population and allocated budgets for their National TB Programs (NTP), their comparable levels of estimated TB incidence coupled with TB control as a shared national priority provide a framework for future scientific TB collaboration and partnerships. Table 1 presents estimated indicators of TB burden, treatment and NTP financing for both countries in 2016.[7,9] National surveillance programs have reported variation in TB incidence within each country. Table 2 displays TB incidence in 2015 and 2016 for US states and Cuban provinces reporting ≥3 cases per 100,000 population.[10,11]
IMPORTANCE The USA and Cuba—both characterized by low tuberculosis incidence, geographic proximity, robust research capacity and shared health priority for TB elimination—can strengthen institutional scientific collaboration to contribute to achieving tuberculosis control and elimination by 2050.
Table 1: Reported TB cases, treatment and national budgets, USA and Cuba, 2016
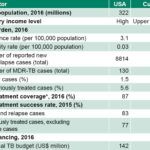
*new and relapse TB cases notified and treated, divided by estimated incident TB cases MDR: multidrug-resistant TB: tuberculosis / Sources: references 7,9
Continued discussions of global TB burden prompted the World Health Assembly to adopt the WHO End TB Strategy in 2014, and shift the dialogue from “stopping TB” to “ending the TB epidemic.”[5] This strategy emphasizes a holistic approach, adopting multisectoral interventions for community health and society, with three main pillars: 1) enhanced patient-centered prevention and treatment (e.g., early diagnosis and treatment of high-risk groups); 2) national policies and supportive systems (e.g., political commitment, community engagement and appropriate health policies); and 3) targeted research and scientific advances (e.g., discoveries to identify innovative strategies and approaches).[5]
Considering this holistic approach with its pillars, collaborative scientific teams are key to advancing the technical agenda and making progress towards TB elimination. In this report, we propose that the USA and Cuba—which have low TB incidence, geographic proximity, robust research capacities, and shared health priorities aimed at TB elimination—can strengthen scientific collaboration for TB control in clinical, laboratory and community settings. Considering TB control efforts in the USA and Cuba, we aim to critically analyze the strengths and challenges experienced in these two low-incidence countries and provide recommendations for future institutional collaboration that can contribute to TB elimination and improved population health.
Table 2: Tuberculosis incidence >3/100,000 populationa, USA and Cuba, 2015–2016
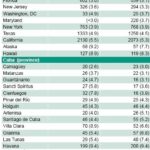
a>3/100,000 population selected as baseline because 2015 national TB incidence in the USA was 3/100,000 population
bnumber of reported cases (US National Tuberculosis Surveillance System) divided by midyear population estimates (US Census Bureau)
cnumber of reported cases (Cuban Ministry of Public Health National Medical Records and Health Statistics Division) divided by population estimates (Cuban Ministry of Public Health statistical yearbooks)
incidence: new and relapse cases in past year
TB: tuberculosis
Sources: references 1,10,11
PROPOSED COLLABORATION
Background This proposed bilateral collaboration in TB control originated from four scientific exchanges since 2014, all with Cuban government approval. In March 2014, participation in the American Public Health Association–Medical Education Cooperation with Cuba (APHA–MEDICC) delegation provided an immersion experience to gain insight into Cuba’s universal health coverage as it functions at the primary care level. Following this exchange, the Cuban Hygiene and Epidemiology Society’s Pulmonary Health Executive Board and the Pedro Kourí Tropical Medicine Institute (IPK), a PAHO/WHO collaborating center, successfully conducted two TB symposia at international conferences in Havana in 2015 and 2016: the International TB Symposium 2015 (Towards TB Elimination 2016–2050),[12] at Cuba Salud 2015 in April 2015, and the International Symposium on Pulmonary Health and TB Elimination (TB Elimination: Accelerating the Pace), held in conjunction with the International Forum on Hygiene and Epidemiology, in November 2016. Both symposia were instrumental in stimulating dialogue on continued efforts towards TB elimination by 2050.[12] Finally, in April 2017, Cuban health leaders and invited international researchers participated in the workshop, Epidemiologic and Operational Research on TB, at IPK.
These events provided opportunities for fruitful scientific and technical exchange among clinicians and health researchers at IPK and the University of Florida (UF), with two notable results: First, Helena Chapman, then a UF doctoral student, received a three-week cross-cultural training in clinical and epidemiologic aspects of TB, mentored by respected clinicians and researchers at IPK and other Cuban Ministry of Public Health (MINSAP) institutions. Second, a collaborative manuscript was published that described the outcomes of the International TB Symposium 2015.[12] Such academic exchanges are evidence of strong commitment to scientific discovery, research and practice en route to TB control and elimination.
The proposed collaboration can strengthen future scientific advances in TB prevention and control efforts, which would be beneficial locally, nationally and internationally, and serve as a model for other countries that aim to build scientific capacity, better understand the epidemiology of TB transmission and reach optimal indicators for population health related to TB control.
Participating Institutions UF, located in Gainesville, Florida, was founded in 1853 and has recently been ranked as one of the USA’s top ten public universities. The Division of Infectious Diseases and Global Medicine forms part of the UF Health Science Center, the largest health education center in the southeastern USA.[13] In addition to academic training and clinical responsibilities in medicine and patient care, scientific research collaborations among various disciplines are fundamental at the UF Health Science Center, UF Emerging Pathogens Institute, Southeastern National TB Center (SNTC), and UF One Health Center of Excellence. SNTC itself provides services to the southeastern USA, including Puerto Rico and the US Virgin Islands. Together, these academic centers provide broad research expertise and potential for collaboration in basic, clinical and social sciences related to spread of emerging infectious diseases that influence human, animal and environmental health in Florida communities.
Located in Havana, IPK was founded in 1937 and has become an internationally renowned scientific institution for undergraduate and graduate academic training, medical care, laboratory diagnostics and research.[14] As part of MINSAP, IPK’s main objectives are to provide optimal medical services to patients, conduct laboratory diagnostics of infectious pathogens, educate Cuban and international students in multiple scientific disciplines, and develop research initiatives on prevention and control of tropical and other infectious diseases. Collaborating departments include the National Tuberculosis, Leprosy and Mycobacteria Reference and Research Laboratory, IPK Hospital, Department of Epidemiology and the National Clinical Reference Center for AIDS Treatment.
Proposed activities Through this proposed collaboration, binational activities between UF and IPK clinicians and researchers in basic, clinical and social sciences related to TB control efforts can identify research gaps and develop innovative projects to strengthen the scientific knowledge base about M. tuberculosis. Notably, these internationally recognized institutions, with robust clinical and research capacities in infectious diseases, have geographic proximity that would facilitate such joint work over the long term. In order to maximize scientific rigor and communication throughout an established research timeline, several activities can facilitate open dialogue, rapport among researchers, task efficiency, adherence to deadlines and overall transparency.
We propose a US-Cuban collaboration to develop a long-range strategy for research into TB epidemiology as it relates to the geographic catchment area of each institution, an accounting of best practices that have emerged in each area, analyses of persistent problems and innovative proposals to address these challenges, and a publication agenda to share findings with the scientific and public health communities. Working methods would include conference calls, web-based seminars, academic exchanges, research collaborations and joint publications.
ANALYSIS
Strengths Since NTPs were founded in the USA and Cuba, efforts towards TB elimination have integrated essential components of TB control. Political commitment can be described in the context of government responsibility, accountability and rapid responses to TB epidemics.[15,16] The US Public Health Service’s NTP was established in 1944, eventually transitioning financial support from local and state governments to the federal level.[15] In Cuba, the national TB surveillance system was initiated in 1953.[16] Cuba’s NTP was established in 1959, and national policies and guidelines were implemented in 1963 and 1964, focusing on population-based health promotion and disease prevention for TB control.[16] Notably, neonatal BCG vaccination has been a routine preventive measure in Cuba,[17] but not in the USA.
All countries have encountered challenges in managing MDR-TB, diagnosing and treating LTBI, and identifying and preventing TB transmission in high-risk population groups. However, rapid and effective responses to these challenges by NTPs in the USA and Cuba have demonstrated successful identification of TB cases, reduction of TB incidence and mortality, and increased treatment success rates.[18,19] Over time, robust M. tuberculosis monitoring and surveillance systems; universal access to directly observed treatment, short-course; and contact followup have proven to be strengths for rapid outbreak control. Strict M. tuberculosis infection control practices and continued research and international collaboration to understand TB dynamics complement the structure and function of these two systems. Also, promotion of human rights and ethical treatment of TB patients has aimed to reduce social stigma and discrimination that may hinder access to TB service delivery or negatively influence health-seeking behaviors.
Challenges In addition to the global challenges, TB control in low-incidence countries such as the USA and Cuba presents unique hurdles to continuing to improve TB indicators. Sustained innovative programs and collaborations that target these challenges will facilitate TB elimination.
LTBI and risk of TB reactivation Prompt identification of population groups at high risk for TB infection or disease is essential for TB control. Certain groups have risk factors for M. tuberculosis exposure, such as those with occupational risks (e.g., health care workers), compromised immune systems (e.g., HIV/AIDS), comorbidities (e.g., diabetes) or toxic behaviors (e.g. tobacco use) that also lead to higher risk for TB infection or reactivation.[8]
Migration from high-burden to low-burden countries Low-incidence countries, which have less active TB transmission than high-incidence countries, have documented TB transmission based on immigration.[8] Migrants may have previous M. tuberculosis exposure from their country of origin; their latent infections can progress to active TB disease following a stressful relocation and settlement process, and further increase population risk of exposure.
Delayed identification and treatment of TB cases Delays in health care service delivery to diagnose TB can be attributed to health providers (e.g., medical error) or patients (e.g., reduced health care-seeking behavior due to stigma, mistrust of authorities or lack of service availability or access to health institutions).[18] It is thus essential to avoid missed opportunities to identify TB infection or disease in the general population.
Expertise in TB control Low TB incidence may result in fewer professionals having direct experience with TB, which may lead to gaps in health professions education and training, contributing to medical errors, lapses in infection control practices, or inadequate outbreak control and contact followup.[18] Existence of and adherence to administrative, environmental and respiratory protection controls in M. tuberculosis are crucial to reduce nosocomial TB transmission in health institutions.
Type of institution Although UF and IPK are both institutions that focus on scientific advances in clinical and research capacities, they have differing characteristics. UF is a public (state) academic institution of higher learning, forming part of Florida’s state university system, and includes SNTC’s state and regional scope. IPK is a public (national government) institution, under MINSAP, with academic functions as well as clinical responsibilities at municipal, provincial and national levels.
US embargo against Cuba In 1961, the US Congress passed legislation forbidding assistance to communist countries, including Cuba, and authorized the President to embargo all trade with Cuba. The embargo was formally declared on February 3, 1962 and has since limited direct interactions between the two countries, impeding trade and commerce, economic relations, and aid and development, and making scientific collaboration challenging.[20] Despite such restrictions, academic exchanges in clinical practice and research activities over the past decade have fostered an open scientific dialogue between US and Cuban scientists.
Next steps and recommendations Challenges in TB control encountered in low-incidence countries will continue, so collaborative efforts between the USA and Cuba need to take a holistic approach towards reducing TB burden, emphasizing the importance of understanding all determinants that influence physical and psychosocial health outcomes related to TB, is imperative for clinicians and researchers leading efforts towards TB elimination. Hence, targeted efforts to reduce risk of M. tuberculosis transmission can be multidisciplinary in nature in clinical and community settings. Passive and active surveillance of active TB cases can rapidly identify persons with TB infection or disease, reducing diagnostic delay, enabling timely preventive or curative therapy as needed, and increasing the proportion of cases successfully treated. Likewise, rapid identification of social or structural barriers in health care service delivery can improve understanding of TB dynamics and serve to strengthen established TB control policies. Next steps in TB control, incorporating scientific evidence to inform policy, include:
Renewal of political commitment to TB elimination It is essential to understand the structural determinants of TB control based on federal or national policies and directives that drive legal regulations and budget allocation. NTPs require administrative leadership and financial resources to maintain universal access to and availability of TB service delivery in all institutions and communities.
Implementation of new technologies to facilitate TB diagnostics and treatment Development of new technologies, whether in laboratory diagnostics or more effective treatment regimens, is key to prompt diagnosis and treatment of TB infection and disease.
Promotion of sustainable training and evaluation Continued training in basic, clinical and social sciences can advance scientific and social understanding of M. tuberculosis and transmission dynamics, yet can be difficult in the face of an epidemic with decreasing incidence rates. Highlighting barriers among health care workers or community members that may hinder components of TB service delivery can support formulation of more efficient designs or alternative approaches for holistic care.
Quality assurance of monitoring and evaluation in TB control Close examination of TB control through monitoring and evaluation procedures can identify poor quality or gaps in practice so that they can be modified. By identifying discrepancies in TB burden among states or provinces, preventive actions and prioritized medical attention can be concentrated on the geographic sites most in need.
Focus on LTBI Current TB control efforts and economic development have helped reduce active TB incidence, but to ultimately eliminate TB, a much greater focus on testing and effective treatment of LTBI is critical. Scaling up LTBI services will require operational and clinical research to inform new policies.
CONCLUSIONS
Countries with low TB incidence, such as the USA and Cuba, have made successful strides in the move to eliminate TB by 2050. Their collaboration can serve as a model for other countries that intend to reach population health targets for TB, improve understanding of TB epidemiology, and strengthen academic capacity-building and training of basic, clinical and social scientists. With close geographic proximity, research capacity and shared health priority for TB elimination, the two nations can collaborate and share clinical, laboratory and community health experiences to accelerate TB elimination throughout the Americas Region.
References

- World Health Organization. Global Tuberculosis Report 2017. WHO/HTM/TB/2017.23. Geneva: World Health Organization; 2017. 147 p.
- Chapman HJ, Lauzardo M. Advances in diagnosis and treatment of latent tuberculosis infection. J Am Board Fam Med. 2014 Sep–Oct;27(5):704−12.
- Hill AN, Becerra J, Castro KG. Modelling tuberculosis trends in the USA. Epidemiol Infect. 2012 Oct;140(10):1862−72.
- Figueroa-Muñoz JI, Ramon-Pardo P. Tuberculosis control in vulnerable groups. Bull World Health Organ. 2008 Sep;86(9):733−5.
- World Health Organization. Implementing the End TB Strategy: The essentials. WHO/HTM/TN/2015.31. Geneva: World Health Organization; 2015. 130 p.
- Rendon A, Fuentes Z, Torres-Duque CA, Granado MD, Victoria J, Duarte R, et al. Roadmap for tuberculosis elimination in Latin American and Caribbean countries: a strategic alliance. Eur Respir J. 2016 Nov;48(5):1282−7.
- World Health Organization. Tuberculosis country profiles, 2016 [Internet]. Geneva: World Health Organization; 2017 [cited 2018 Jan 26]. Available from: http://www.who.int/tb/country/data/profiles/en/
- World Health Organization. Towards tuberculosis elimination: An action framework for low-incidence countries. WHO/HTM/TB 2014.13. Geneva: World Health Organization; 2014. 67 p.
- The World Bank. World Bank Open Data [Internet]. Washington, D.C.: The World Bank; c2017 [cited 2018 Jan 26]. Available from: http://data.worldbank.org/
- Schmit KM, Wansaula Z, Pratt R, Price SF, Langer AJ. Tuberculosis – United States, 2016. MMWR Morb Mortal Wkly Rep. 2017 Mar;66(11):289−94.
- National Health Statistics and Medical Records Division (CU). Anuario Estadístico de Salud, 2016 [Internet]. Havana: Ministry of Public Health (CU); 2017. 206 p. Available from: http://files.sld.cu/dne/files/2017/05/Anuario_Estad%C3%ADstico_de_Salud_e_2016_edici%C3%B3n_2017.pdf. Spanish.
- Chapman HJ, Armas Pérez L. Innovative Tuberculosis Symposium held during Cuba Salud 2015. Tuberculosis (Edinb). 2016 Dec;101:41−3.
- University of Florida. Division of Infectious Diseases and Global Medicine [Internet]. 2017 [cited 2017 Nov 20]. Gainesville (US): University of Florida; c2018 [cited 2017 Nov 20; updated 2018 Mar 1]. Available from: http://id.medicine.ufl.edu/
- Pedro Kourí Tropical Medicine Institute [Internet]. Havana: Pedro Kourí Tropical Medicine Institute; c1999-2018 [cited 2017 Nov 20]. Available from: http://instituciones.sld.cu/ipk/informacion-del-ipk/. Spanish.
- Binkin NJ, Vernon AA, Simone PM, McCray E, Miller BI, Schieffelbein CW, et al. Tuberculosis prevention and control activities in the United States: an overview of the organization of tuberculosis services. Int J Tuberc Lung Dis. 1999 Aug;3(8):663−74.
- Beldarraín E. Impact of the 1970 reforms to Cuba’s national tuberculosis control program. MEDICC Rev. 2015 Jul;17(3):33−8.
- Galindo BM, Concepción D, Galindo MA, Pérez A, Saiz J. Vaccine-related adverse events in Cuban children, 1999–2008. MEDICC Rev. 2012 Jan;14(1):38–43.
- Taylor Z, Nolan CM, Blumberg HM; American Thoracic Society; Centers for Disease Control and Prevention; Infectious Diseases Society of America. Controlling tuberculosis in the United States. Recommendations from the American Thoracic Society, CDC, and the Infectious Diseases Society of America. MMWR Recomm Rep. 2005 Nov;54(RR-12):1−81.
- González E, Armas L, Llanes MJ. Progress towards tuberculosis elimination in Cuba. Int J Tuberc Lung Dis. 2007 Apr;11(4):405−11.
- Drain PK, Barry M. Fifty years of U.S. embargo: Cuba’s health outcomes and lessons. Science. 2010 Apr 30;328(5978):572–3.
THE AUTHORS
Helena J. Chapman (Corresponding author: Helena.Chapman@medicine.ufl.edu), physician specializing in public health, with a master’s degree in public health (epidemiology) and doctorate in public health (One Health). Division of Infectious Diseases and Global Medicine (DIDGM), College of Medicine, University of Florida (UF), Gainesville, Florida, USA.
Luisa A. Armas-Pérez, pulmonologist with a master’s degree in epidemiology. Associate researcher and associate professor, Department of Epidemiology, Pedro Kourí Tropical Medicine Institute (IPK), Havana, Cuba.
Michael Lauzardo, internist and pulmonologist with a master’s degree in epidemiology. Associate professor, DIDGM, UF College of Medicine, Gainesville, Florida, USA.
Edilberto R. González-Ochoa, physician epidemiologist with a doctorate in health sciences. Full professor and senior researcher, Department of Epidemiology, IPK, Havana, Cuba.
Submitted: October 27, 2017 Approved: March 07, 2018 Disclosures: None