INTRODUCTION
As yet, there is no vaccine against HIV. The epidemic has orphaned millions of children. In many cases, family members have to raise children left behind or whose parents are afflicted with HIV.
According to UNAIDS, in 2009, 33.4 million people were living with HIV around the world; 2.1 million of them were children aged <15 years. Over 90% of these children acquired the infection by mother-to-child transmission, reaching nearly 100% in developing countries.[1]
In Cuba, the Ministry of Public Health reports that from 1986 to December 31, 2009, 420 children of seropositive mothers had been identified: 295 were healthy, 89 were undergoing testing, 36 had been diagnosed as seropositive and 34 had developed AIDS.[2] These data place Cuba among the countries with low rates of HIV-infected children.
An HIV diagnosis, like that of any another chronic illness, alters family dynamics. Although the whole family is affected by the illness, in most cases only one person assumes the sick person’s care. This is usually a family member who must adapt to the stresses of caregiver demands.[3,4] Many families have experience in caring for a chronically ill member, in which the primary caregiver is usually healthy. Nonetheless, HIV/AIDS presents a new challenge for family dynamics because when the infection is by mother-to-child transmission, the mother also is infected, requiring a different approach to the process of care.
The primary caregiver attends to the sick person’s physical and emotional needs, and is usually the husband, wife, son, daughter, other close relative or friend.[4] Researchers on caregivers of the chronically ill have approached assessment from different points of view. Some studies present the negative impact on mental health, generally known as caregiver burden and caregiver stress.[5] Others explore coping mechanisms in positive terms relating to the caregiver’s self-esteem or satisfaction.[6] Other studies, however, offer a broader assessment concerning health, mental health and quality of life.[7]
According to WHO, mental health is defined as “a state of well-being in which every individual realizes his or her own potential, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to her or his community.”[8] Héctor Sierra, a Mexican psychologist and expert in the mental health field, confirms that loss of mental health is “not only a consequence of biological fatalism or the result of an unfortunate personal history, but [can also be] the result of concrete experiences lived in the here and now within our social environments.”[9]
Children and adolescents with HIV/AIDS require care appropriate to their physical, psychological and social development. Their caregivers should be responsible people who maintain adequate physical and mental health. Medical attention for children with HIV/AIDS and their families has tended to focus on physical care. Our study stems from the premise that a more comprehensive approach to the health–illness continuum is needed that takes into account mental health, key to an individual’s balance and social adjustment.
The study’s objective was to describe general mental health characteristics of primary caregivers of Cuban children and adolescents from across the country who were diagnosed with HIV/AIDS at the Pedro Kourí Tropical Medicine Institute (IPK).
METHODS
Participants A descriptive study was carried out of primary caregivers of children and adolescents with HIV diagnosed at the IPK pediatric HIV clinic through 2009. Eligible participants were caregivers of children who were alive at the time of the study, receiving followup at the pediatric HIV clinic and whose infection was due to vertical transmission, blood transfusion and/or hemoderivatives. As a result, 26 caregivers of children attending the clinic from November 2009 through March 2010 were invited to participate.
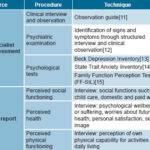
Procedures This study examined current mental health status using self-report, mental health specialists’ assessment and specific psychological tests (Table 1). Assessment of each caregiver was carried out in a quiet and private setting in a single session lasting approximately two hours. Results were integrated to determine presence of mental disorders, using as a guide the Tenth International Classification of Diseases (ICD-10).[10]
Psychological assessment Clinical interview and observation. A diagnostic-investigative clinical interview was conducted, covering sociodemographic data (age, sex, educational level, employment and HIV serostatus) and individual behavior and relationships (family, personal, sexual-marital, school and workplace), in order to understand both strengths and potential pathologies. We used the guide proposed by Alvarez to systematically observe aspects such as facial expression, posture, behavior, speech, appearance and attitudes towards the conversation and interviewer.[11]
Psychiatric examination. This included a general description of the caregiver and an examination of ability to integrate information and of relational, intellectual, cognitive, emotional and behavioral functions.[12]
Psychological tests. The Beck Depression Inventory (BDI) was used to identify depression. The BDI consists of 21 items for assessing intensity of depression, each scored in a four-point scale. Depression is demonstrated in established degrees: mild, moderate and severe. We took into account the degrees as well as the 21 dimensions (found in the referenced document).[13]
Table1: Psychological assessment procedures and techniques
The State Trait Anxiety Inventory (STAI) begins with theoretical consideration of anxiety in two forms of expression, as a state and as a trait. As a state, it can be thought of as a transitory or situational emotion that varies in intensity and fluctuates with time. As a trait, it refers to relatively stable individual variations (personality characteristics) in terms of the propensity for anxiety, or tendency to perceive a broad series of situations or stimuli as dangerous or threatening, and the tendency to react to such “threats” with anxiety.[14]
The Family Function Perception Test (FF-SIL, the Spanish acronym) was used to evaluate systemic relational dynamics among family members, using one member’s perceptions as a starting point. This test classifies families in four categories with respect to their degree of function: functional, moderately functional, dysfunctional, and highly dysfunctional.[15]
Analysis A descriptive analysis was made of caregivers’ sociodemographic variables and HIV status. Triangulation of information was incorporated for individual analysis, validating the qualitative information obtained from the techniques and tests administered. First, we assessed the caregivers’ performance on each of the tests. Second, we integrated this information with the goal of determining presence of mental disorders.
Ethical considerations Written informed consent was obtained from all participants, following an explanation of study objectives and assurance of psychological care if needed. The IPK ethics committee approved the study.
RESULTS
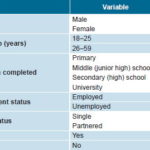
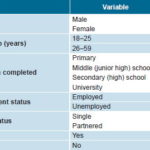
Of the 26 caregivers invited, 13 participated in the study. Of these, ten were HIV positive. Twelve participants were women; six were single; seven had completed secondary (high) school; and nine were aged 26–59 years (Table 2).
Clinical interview and observations The group was generally cooperative and participated satisfactorily in the study. Noteworthy among observations were worried and serious facial expressions in nine participants. Seven caregivers paused frequently when answering questions about HIV, specifically with reference to their children, and exhibited tense posture and some untidiness of physical appearance.
The majority of caregivers demonstrated adequate social adjustment. Nevertherless, nine caregivers indicated conflicts and communication problems, especially in parent-child relationships. Eight participants reported experiencing parental divorce and excessive parental demands during their childhoods, as well as inadequate guidance received from their parents. Nine caregivers had poor academic performance, with low grades and failed years. Eight participants reported poor school adjustment and six said they had no plans for further education.
Eight were unemployed, and six had begun to work only between ages 28 and 31 years because they thought they did not need to work. Eleven had no plans for career advancement. When asked about sexual and marital matters, ten participants reported having had little information at the time of sexual initiation; eight reported dissatisfaction with their relationships and only five thought their relationships might improve in the future. Family conflicts were reported by eight caregivers. Seven of the ten HIV-positive caregivers reported conflicts related to the infection itself, such as feelings of stigmatization or discrimination.
Table 2: Sociodemographic characteristics of caregivers of HIV-positive children
Psychiatric examination None of the caregivers fulfilled criteria for a psychiatric disorder, although in the affective sphere three subjects reported symptoms of anxiety and depression, two of them following their children’s diagnosis of HIV infection. Other symptoms were short-term memory loss, diminished intellectual capacities, low libido and sleep-onset insomnia.
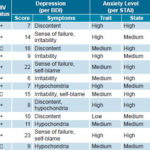
Psychological tests Five caregivers presented with depression according to BDI, three mild and two moderate. Six caregivers reported symptoms in the dimensions of failure, self-blame and irritability; another seven reported the same symptoms and also discontent and hypochondria (Table 3).
Table 3: Results of psychological tests on caregivers of children with HIV/AIDS in Cuba
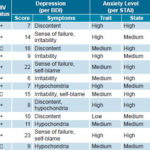
BDI: Beck Depression Inventory (0–13 minimal; >29 severe) STAI: State Trait Anxiety Inventory FF-SIL: Family Function Perception Test
Twelve members of the group had high or moderate levels of anxiety (six of each) as a trait according to STAI. All had high or moderate levels of anxiety (six and seven respectively) as a state.
Twelve caregivers perceived their families as functional and one moderately functional.
DISCUSSION
It is noteworthy that of 26 caregivers invited to participate in the study, seven refused and another six agreed but did not appear for sessions. Although specific reasons were not given, experience allows us to hypothesize on some of these.
Caregivers who refused may have had personal or relationship issues they did not feel comfortable sharing or exploring in depth. Those who accepted in principle but did not attend also missed appointments they had scheduled with their children’s pediatricians the same day. These caregivers were from different provinces throughout Cuba, and even though the study took advantage of these scheduled medical appointments to avoid an extra trip to Havana, their absence serves as a lesson. In future, we might extend the study period or have the research team travel closer to where caregivers live.
The sociodemographic characteristics of the group studied revealed some patterns. The majority of caregivers were female, consistent with other reports in the literature,[3,16] and also confirming the role assigned to women in our society as protectors and overseers of family health. Problems with partner relationships and employment were also highlighted. The fact that a substantial proportion of the group was single and unemployed suggests the possibility of a direct association between women caregivers, single status and unemployment.[17,18]
Research by Worthington and Krentz[19] showed that the strongest predictor of quality of life related to health of adults living with HIV is employment status. In other words, a protective factor for the mental health of HIV-positive persons may be not only employment, but the social connections a job provides. This finding is highly relevant to our study group, ten of whom were HIV positive.
It is understandable that a stable partner relationship is also difficult to achieve, among other things because of constant concerns for the health of the child in their care and for their own health, and because of exclusionary attitudes still exhibited by some people towards persons living with HIV. There is also the challenge of how to tell a partner about HIV status in the face of possible rejection and termination of the relationship.
According to studies by Scherma[20] and Kwan[21], the work of providing continuous care often results in weakness, fatigue, a sense of failure, a loss of self awareness, insomnia, somatic symptoms, priority-setting difficulties, depression, social isolation, increased self-medication, irritability, lack of organization, and poor concentration and productivity. Several published studies[22–24] are consistent with ours in finding high anxiety levels in persons with HIV. The combination of HIV-positive status and the burden of caregiving may make these symptoms weigh even more heavily. This could be because, among other reasons, illness in itself produces a degree of anxiety, more so in the case of HIV, which still connotes certain death in the public’s mind.[19]
Anxiety was objectively assessed and found present in caregivers’ life dynamics. Note that nine participants identified family problems as the source of their anxiety. The family is the caregiver’s main support; but if this support fails or leads to dissatisfaction, it can reduce the caregiver’s level of functioning and chances for balanced mental health, leading to increasing and persistent anxiety.
It is important to note that the family function test did not provide sufficient information about actual status of family relationships, although we did find clues in the clinical interviews. Given the above, we suggest that future research on caregivers of children with HIV/AIDS should utilize more qualitative methodologies to study family dynamics, favoring techniques involving family member interaction and observation. This could lead to a better understanding of such problems and encourage comprehensive and in-depth interventions.
It is noteworthy that many of the symptoms found in this study stem from the constant tensions and expectations entailed in the caregivers’ day-to-day struggles to protect the health of the children under their care, and in the case of those infected with HIV, to care for themselves.
This study described the mental health status of primary caregivers of children with HIV/AIDS from various provinces in Cuba, paving the way for more comprehensive assessment of a little-studied group. This type of study can assist health care providers in encouraging positive family-caregiver-child interactions that enable and promote adequate health in each family member. The findings will help us as a mental health team improve our attention to these caregivers and children by addressing their main needs in a more objective way and understanding the nature of their most important problems. In this way, we can help develop their response capacities and coping mechanisms, supporting improved mental health, a necessary condition for effectively performing their work as caregivers—which is so important and frequently undervalued in society. Our study provides a first approach to a comprehensive assessment strategy; it should be supported by future studies with more participants.
CONCLUSIONS
Caregivers described complex intra- and interpersonal life dynamics, influenced by their HIV infection, suggesting, the need to integrate clinical and mental health approaches for more comprehensive and effective services for this group. In planning services for caregivers of persons living with HIV, the health system should emphasize a broader vision of health, including attention to family function. Educational strategies involving exchanges among families and treatment teams, where positive coping mechanisms, psychological support and improvement of family dynamics are promoted, could contribute to improved quality of life for both patients and their families. Future research in this area should favor qualitative approaches that can provide a deeper understanding of caregivers’ life dynamics and favor a more comprehensive approach to their mental health.
ACKNOWLEDGMENT
The authors dedicate this article to the memory of Elvis Guerrero Lobaina MS, a psychologist who worked closely with our group on the study. He died in 2010, leaving his wisdom to new generations of Cuban psychologists.