Dra. Rosaralis Santiesteban
MEDICC Review: Where did the epidemic start? How did the first cases present?
Rosaralis Santiesteban: The first cases appeared toward the end of 1991 in Pinar del Río Province in western Cuba: a bilateral optic neuropathy sometimes accompanied by peripheral sensory neuropathy and, in a minority of cases, myeloneuropathies. At first it was called optic neuritis, then epidemic optic neuropathy; then as peripheral nervous effects became apparent in some patients, a more general term was applied: Cuban Epidemic Neuropathy (CEN). By 1993, the epidemic had spread to all provinces, with some 50,000 cases, including optic, peripheral and mixed forms.
From the beginning, there was a great deal of discussion and investigation concerning its etiology. In 1992, a multidisciplinary commission established to study the epidemic hypothesized that the cause was toxic, nutritional, or both, without ruling out a contributing viral factor. The fact that Cuba’s health system is universally accessible and population health indicators were excellent at the time—while poorer countries with less robust health systems did not report cases—at first worked against the nutritional hypothesis. That remained a question for quite some time and led to several lines of new research into the nutritional status of the affected population.
MEDICC Review: What was finally concluded about the epidemic’s cause?
Rosaralis Santiesteban: The best-supported causal hypothesis is that a decline in nutritional status compromised the normal detoxification mechanisms that protect against toxins like cyanide.
Our epidemiological studies related smoking with the optical and mixed forms—but not peripheral neuropathies—with a dose-response effect. It is well known that other substances detoxified by the same pathways can produce lesions in neural tissue requiring the most energy to function, such as the optic and acoustic nerves and long neural pathways. It’s possible that giardiasis created chronic malabsorption, aggravated by diarrhea, which could have precipitated the appearance of symptoms, as was observed in studies in Cienfuegos province.
Although one can’t completely discard the possibility of a viral factor, it doesn’t really fit the clinical picture. Nor do the epidemiologic and laboratory studies bear out the idea of an infectious or biological agent. And what’s more, the response of patients to vitamin supplements reinforced the hypothesis that the disease was due to a nutritional deficit, exacerbated by toxic substances like alcohol and tobacco.
MEDICC Review: Why is it that we don’t see many similar epidemics in developing countries where malnutrition is prevalent? Why did it appear in Cuba, which in many ways was better off?
Rosaralis Santiesteban: Historically, epidemic forms of optic and peripheral neuropathies and myeloneuropathies in different parts of the world have nearly always been associated with wars, famine and environmental catastrophes. None of their causes has been determined definitively, but in almost all cases a nutritional deficit predominated. Yet, in some of the same African countries where we see malnutrition leading to blindness from cataracts and corneal perforations, even death, we don’t tend to see these neuropathies. It may be that their effects are such that most people can keep going about their daily lives. Or, in countries where the poor have little or no access to medical attention, the health care system may not even detect the cases.
However, perhaps the most reasonable general explanation is that the basic dietary starting point is different, with lower general caloric, protein and micronutrient consumption. Whereas in Cuba’s case, the culprit appears to be the very abruptness of onset of the nutritional deficit. Before the epidemic, Cuba’s health indicators were quite good: for example, Cuba’s 1992 infant mortality placed it among the 25 countries with the lowest rates. The health system was built upon strong primary care, which reached into rural and urban communities alike with services free to patients. Education was free, even through university, and the population was highly educated. Sports and other areas indicative of quality of life were also well developed. So then, it seemed incredible to see an epidemic related to nutritional deficiency.
But you have to recall that the fall of the Soviet Union and the dissolution of the socialist bloc in 1989 had removed Cuba’s main buffer against the devastating effects of the US economic blockade. This threw Cuba into a prolonged economic crisis known as the “special period,” lasting through most of the 1990s. The first 5 years were the hardest, and meant drastic changes in lifestyle for the vast majority of Cubans because of the lack of food and fuel for transportation. Daily per capita calorie intake fell from 2899 kcal in 1988 to 1863 kcal in 1993. This caloric deficit was compounded by increased physical activity, principally walking and cycling. We imported more than 700,000 bicycles in 1990, which were sold cheaply so people could ride to work or school. As a result of all this, an astounding 27% of adults lost more than 10% of their body weight.
The source of caloric intake was also problematic, because of an inappropriate composition of protein, fat and carbohydrates. The distribution of basic foodstuffs was regulated in Cuba and prices were subsidized, but a lot of what people ate was low in vitamins. It is significant that we haven’t seen this sort of epidemic generally in other Latin American countries where corn has remained the dietary staple of the poor for millennia. Corn has practically all the essential aminoacids, apart from tryptophan, and in some places, for example in rural Ecuador, people add wild berries to their drinking water, thus getting the benefit of their vitamins and antioxidants.
Corn and root vegetables were also the basis of the Cuban diet until the middle of the 19th century, when Chinese immigrants introduced rice as a crop. Rice soon replaced other crops like corn and root vegetables, leaving the country with a diet that “consumes” vitamins rather than providing them as it metabolizes. Then you add the fact that Cuba has long been a producer of sugar, rum and honey, all of which deplete vitamins and have toxic effects if not combined with adequate intake of other nutrients. As you know, we need the B vitamins to assimilate carbohydrates, especially vitamin B1, which isn’t stored very long in the body.
Even more now, the Cuban diet is based on rice and beans. Beans have some vegetable protein, but they’re cyanogenic, as is cabbage, also commonly consumed during the period of the epidemic. And of course the toxic effects of tobacco smoke, which produces cyanide and other toxins, would have exacerbated the effects of the sudden decline in food intake and increase in physical activity, bringing about the epidemic we saw. A social phenomenon that complicated the situation was easy access to tobacco and badly-distilled home-brewed alcohol. Foods containing fat and protein were scarce and expensive on the black market, as were vegetables (which, in any case, Cubans didn’t habitually consume in large amounts), while it remained easy for people to get tobacco and alcohol.
MEDICC Review: Who was most prone to the neuropathy?
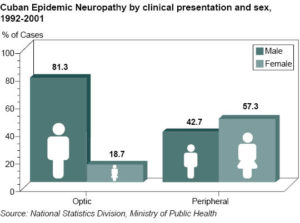
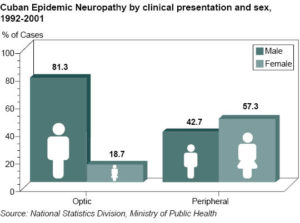
Rosaralis Santiesteban: Those most affected were people with the highest nutritional demands: smokers and drinkers, people with intense physical activity and those with greater body mass. For the optic form, men were more at risk than women on all counts: the Nutrition and Food Hygiene Institute found that at the time of the epidemic, men smoked at almost twice the rate of women, alcoholism was more than twice as prevalent among men and they also had significantly greater physical activity. When you add the fact that men in general have more body mass, it’s not surprising that men predominated among victims of the optic form of CEN, for which these risk factors were much stronger. On the other hand, the peripheral form was less affected by toxins and more by nutritional deficit—specifically vitamin B1 deficiency—and women were more affected than men. Children and the elderly were relatively spared because they were given preference in food distribution, both by the government and traditionally by families within households.
MEDICC Review: The course and impact of the epidemic also differed somewhat across the country.
Rosaralis Santiesteban: Yes. Nationally, the disease affected 0.5% of the population. But some provinces were affected earlier, and some more than others. For example, as I mentioned, the first cases were found in Pinar del Río, a province with a strong tradition of producing high-quality tobacco, but which has sulphur-deficient soil. At first the epidemic remained localized in that area, with mounting numbers of cases (358 in 1992). Then some cases appeared in Sancti Spíritus province, also in tobacco-growing areas, and in Havana.
Cuban Epidemic Neuropathy by clinical presentation and sex, 1992-2001
Chronology of Cuban Epidemic Neuropathy (CEN)

By the beginning of 1993, national incidence was rising at an alarming rate and there were now cases in every province, although not all were equally hard hit; Pinar del Río always had the highest incidence, reaching a cumulative prevalence of over 1300 per 100,000 in 1993. That year national incidence reached 462 per 100,000, but by June, within a few weeks of distribution of vitamin supplements to the entire population, the curve fell abruptly. This decline happened first in Pinar del Río, which was the first province to supplement the healthy population, well before the rest of the country.
By 1994, national incidence had dropped to 4.9 per 100,000; between 1995 and 1997 there was a small increase, due to a rise of cases in certain provinces after discontinuation of massive distribution of free multivitamins. When these small outbreaks happened, the supply of vitamins was increased and the rates fell again. There was then an uninterrupted decline in new cases until 2002, when the last cases were diagnosed.
By the end of the epidemic, Pinar del Río was still most affected, in terms of cumulative cases, followed by the provinces of Havana City, Matanzas, Cienfuegos, Sancti Spíritus, Camagüey, Holguín and Santiago de Cuba. The fact that these provinces are where tobacco cultivation and consumption are highest suggested one explanation for geographical differences in the epidemic’s impact.
MEDICC Review: Was tobacco the only factor determining why Pinar del Río was hit so much harder than Guantánamo province, for example?
Rosaralis Santiesteban: No, there were also some nutritional differences. Dr Carmen Porrata at the Nutrition and Food Hygiene Institute found that, while the whole country was affected by the abrupt decline in calorie intake starting in the early 1990s, Guantánamo started from a different baseline. The population there had historically adapted to a lower energy diet, so the change was not as extreme for them. And the composition of their diet involved different staples: for example, they depended more on vegetable oil than pork as a source of fat, and tended to eat more plantain and root vegetables and less rice for carbohydrates.
MEDICC Review: It’s remarkable that an epidemic on this scale was brought under control in such a relatively short time. What were the fundamentals of Cuba’s strategy for managing the epidemic?
Rosaralis Santiesteban: In short, there was a systemic, coordinated and truly multidisciplinary response, with a national approach that focused on early detection and treatment with vitamin supplements from the onset of symptoms, eventually expanding supplements to at-risk groups and then to the entire population. The clinical system was mobilized from the municipal level up, to enable monitoring and assessment of clinical results. And we invested a lot in training family doctors and internists, as well as ophthalmologists, in case identification and management. Intense scientific study was also a critical part of the response.
The epidemic affected such a large number of people that it became a major national issue, which is why, despite the economic crisis, the government allocated significant resources to provide free access to vitamins and antioxidants, for a campaign to discourage alcohol use and smoking, and for nutritional education and support for people at greatest risk.
That’s the short answer.
I can give you a bit more detail.
Beginning in May of 1992 the Ministry of Public Health carried out investigations in Pinar del Río to determine etiology, define and characterize the disease, and to establish appropriate treatment as well as eventual rehabilitation for those most severely affected. We then issued an alert to the entire health system, developed case definitions and diagnostic criteria and began to train ophthalmologists to diagnose it. There was a lot of subjectivity in the physical findings, even for the few neuro-ophthalmologists the country had then. The only really objective sign was pallor of the optic disc, which didn’t appear until some months after the first symptoms. Later, we would be able to observe a little edema and a loss of nerve fibers in the papillomacular bundle using red-free filters or halogen ophthalmoscopes that had not previously been available.
With the rush of new cases in 1993, the Ministry of Public Health issued a country-wide alert and advised prescription of vitamin supplements from onset of symptoms. We established new case definitions and norms for diagnosis and treatment, and stepped up vitamin production; vitamins were domestically produced from ingredients acquired abroad. During the first weeks of that year the exponential increase in incidence and the finding of enterovirus in some patients’ cerebrospinal fluid led to questioning of the toxic-nutritional hypothesis. In response, Civil Defence, the Academy of Sciences and the Ministry of Public Health established a multidisciplinary commission, the National Task Force, to broaden causal research and try to control the epidemic. The Group’s work was given top priority by the government and it reported daily to the highest authorities.
At that time, the case definition of the optic form was refined with description of hyperemia and optic disc pallor. Ophthalmologists were trained to deal with the avalanche of cases and to contribute to provincial and national research studies to assess the impact of new treatments complementing vitamin supplementation. The results of these studies led to the distribution of free multivitamins to the country’s entire 11 million people and a national campaign to discourage smoking and alcohol use. Over the next few years, there were a few small, local outbreaks that were readily controlled with vitamin therapy.
After the year 2000, there were only isolated new cases but the Ministry of Public Health decided to continue providing free vitamin supplements to the at-risk population. No new cases have been reported since 2002. Low-cost vitamin supplements are still available, and family doctors continue to promote their use.
MEDICC Review: What has become of the people who became ill during the epidemic?
Rosaralis Santiesteban: Patient assessment was carried out more frequently during the first year of follow-up, usually by ophthalmologists; later, annual checkups were carried out by family doctors. A number of surveys were taken in the years following the epidemic phase: the 1999 survey evaluated 94.6% of all cases diagnosed by then; using the WHO definitions of low vision, disabled and legally blind to assess disease sequelae in the optic form. The vast majority of sequelae observed in 1998 and 1999 were visual.
The 2002 survey excluded false positives to date, reducing the cumulative number of cases by more than 3500. Only about 10% of cases had sequelae: 2275 with vision problems and 2543 with peripheral nerve sequelae. By 2005, there were 4363 patients who still had some degree of impairment: 90.4% had low vision (some visual impairment but functional with or without corrective lenses), 8.6% were disabled with best corrected vision less than 0.3, and 1% legally blind with vision less than 0.1 in the better eye. Only 5 patients with the peripheral form remained handicapped and 38 with the optic form were legally blind. The highest numbers of severe optic sequelae were observed in the provinces of Havana City, Villa Clara, Sancti Spíritus and several eastern provinces where Leber’s Hereditary Optic Neuropathy (LHON)—a disease with a similar mitochondrial deficit and with severe visual sequelae—was also much more common. In western and central Cuba, we didn’t see peripheral sequelae to the extent that we did optical.
In 1998, the National Follow-up Program for neuropathy was launched to make sure that people who were left with sequelae got the help they needed. The Program involved a reorganization of the diagnostic and monitoring process at the municipal and provincial levels to facilitate evaluation and rehabilitation of patients with sequelae from both forms of the disease. We followed the WHO classification of health and functioning: impairment referring to the strict physiological effects, disability to functional effects of impairment, and handicap to the social impacts of these. Clinicians from family doctors to ophthalmologists had to be trained in the correct classification in order to develop appropriate rehabilitation plans and of course, physiatrists had to be involved. The Program, headed by Dr Carmen Serrano, continued to monitor cases until 2008.
MEDICC Review: You mentioned that this isn’t the first time Cuba has experienced this sort of epidemic.
Rosaralis Santiesteban: After careful study of the medical literature, I am convinced that such cases also appeared in other periods when hunger and malnutrition were rampant, specifically in the difficult years of Cuba’s two wars of independence in the 19th century.
I was able to review Cuban articles that appeared in the late 1800s and early 20th century—particularly the work of Cuban ophthalmologist, Dr Juan Santos Fernández, in which he mentioned a similar illness in Cuba at the end of the 19th century, described by his former student, Dr Domingo Madan. It was Dr Santos Fernández who first reported the temporal optic disc pallor I mentioned earlier—now considered pathognomonic of CEN and tobacco and alcohol-related amblyopia (TAA)—among patients with supposed TAA during the first war of independence, 1868–1878. The main clinical description was published by Dr Madan, in reference to an 1897 outbreak in Matanzas province during the last war of independence, when Spanish authorities confined the rural population to the cities and 300,000 civilians died of hunger. At the time, these conditions were treated as TAA, even though some patients denied using either substance or used them only rarely. Dr Madan eventually concluded that it was a toxic nutritional condition in non-alcoholics and spent the rest of his life trying to mitigate its causes. The disease was mentioned again by Dr Enrique López in 1900, who called it “blockade amblyopia” because it emerged during a period of severe hardship and even famine, exacerbated by the US blockade of Cuban ports in 1898.
Cuban Epidemic Neuropathy by clinical presentation and incidence, 1992–2002

*per 100,000 population Source: National Statistics Division, Ministry of Public Health
MEDICC Review: What was the role of international experts in the response to the epidemic?
Rosaralis Santiesteban: The epidemic’s scope, exponential growth and unknown causation attracted scientific collaboration from many countries. Faced with a possible infectious epidemic with rapidly rising incidence, we informed the international scientific community when the Vice-Minister of Public Health, Dr Jorge Antelo reported the epidemic to the 46th World Health Assembly in Geneva on May 4, 1993. The response was immediate, with the arrival of both material assistance and visiting experts. Dozens of scientists from abroad came to Cuba in 1993 to help: this was the most dramatic period of the epidemic, when we still hadn’t ruled out an infectious cause.
Visiting experts collaborated with Cuban scientists on several studies to clarify etiology, optimize diagnosis and investigate toxicity mechanisms. For example, Drs Alfredo Sadun and Janis Eels reproduced the disease in rats by putting them on a diet low in folic acid and giving them small quantities of methyl alcohol. Sadun also looked at the pathophysiological effects on the rats’ optic nerves and observed the same type of damage as in CEN and LHON. He reported his findings in 1995 and published several related articles, attracting particular attention since he elucidated the pathophysiology of these and other diseases of the optic nerve that had not yet been explained. Because of this work he received Lighthouse International’s Pisart Vision Award, awarded for major contributions to understanding diseases affecting vision.
Other neuro-ophthalmologists—such as Drs Thomas Hedges, Samuel Skolt, Gordon Plant, Geoffrey Arden and Janet Wolf—worked with us in several visits to Cuba and made important contributions. Among scientists in other disciplines who came was a Soviet group that brought a 19th century Cuban medical bibliography containing the material that started me on my journey in medical history, by providing the evidence that this same condition had arisen during our wars of independence.
This evidence was part of the information presented at the international workshop in July, 1994 to review completed and ongoing research into the epidemic. The final consensus was that the likely cause of the disease was metabolic and nutritional, without ruling out the possibility of a viral factor, hence the suggestion to keep pursuing that hypothesis. Drs Sadun, Hedges, Gustavo Román—who led the PAHO team in Cuba—and other scientists urged the US to remove the economic blockade.[3] Despite this, and despite the opposition of the vast majority of member states of the UN, the embargo continues, and has even been tightened.
MEDICC Review: What were the most important lessons learned from the epidemic?
Rosaralis Santiesteban: CEN is still referred to as the model of nutritional optic neuropathy and to explain neuropathies due to other causes also having a mitochondrial defect. The volume of research and clinical activity by both Cuban and international professionals was enormous, resulting in hundreds of publications covering the clinical picture, diagnosis, epidemiology, physiopathology, risk factors, biochemical mechanisms, prevention and treatment, and more. The detailed characterization of the disease is particularly notable: the disease affects several systems, functions and organs besides the eye—the peripheral nervous system, hearing, skin and mucosa. The optic nerve is the principal organ affected, particularly the parvocellular pathways and the papillomacular bundle; what had not been appreciated before this was that the outer layers of the retina are also involved.
Research into CEN reinforced the critical role of nutritional deficit in its etiology, aggravated by the presence of toxic substances like alcohol and tobacco. This of course has profound implications for primary prevention. Our research also contributed to important refinements in our understanding of other neuropathies, such as LHON and TAA.
Beyond the scientific lessons, we learned a lot about what is needed for an effective society-wide response to epidemics. Despite the economic crisis we were experiencing at the time, huge resources went into investigating and controlling CEN. PAHO Director Dr Carlyle Guerra de Macedo, said that he didn’t think there was another country that would have been able to carry out the sheer volume of research and clinical service that Cuba did when faced with this epidemic.[4]