INTRODUCTION
Chronic non-communicable diseases (NCD) have been called the pandemic of the 21st century and constitute a high priority for public health. It is vitally important to improve health systems’ capacity to respond, making better use of preventive potential by reducing prevalence of specific risk factors and conditions: tobacco and alcohol use, unhealthy diet, physical inactivity, obesity, diabetes, high serum cholesterol, hypertension, and physical and chemical factors in the environment;[1,2] hence growing interest in NCD risk factor surveillance.
Globally, NCDs and their risk factors are important and growing contributors to the burden of morbidity, mortality and disability, and to diminished quality of life for patients and their families. NCDs contribute to 60% of all deaths, and of these, 46% are in the population aged < 70 years (the most productive years), to the detriment of countries’ development potential; 80% of NCD deaths are in low- and middle-income countries.[3–5]
In the Americas, 62% (3.2 million) of the 5.2 million deaths reported in 2004 resulted from NCDs, mainly cardiovascular diseases, cancer, chronic respiratory diseases and diabetes. Given current demographic, social and economic changes, as well as epidemiological and nutritional shifts, NCD-attributable deaths are expected to increase in the coming years.[2,3,6] At the same time, a growing body of evidence indicates that NCDs are largely preventable, including assessment of effectiveness, cost, acceptability and feasibility of preventive interventions. Thus, it is estimated that improved diet, more physical activity and eliminating tobacco use could prevent 80% of heart disease and 90% of diabetes cases.[7–10]
In Cuba, NCDs are involved in 76% of all deaths and annual NCD-related mortality (642.2 per 100,000 population) is over ten times the combined rates for communicable diseases and maternal, perinatal and nutritional causes (58.7 per 100,000 population); NCDs add greatly to potential years of life lost and impact negatively on individual quality of life and on the Cuban economy.[11]
National policy statements and other documents have expressed awareness of the importance of NCD risk factors since 1981. A commitment to address them was ratified in the 1992 document Objectives, Principles and Directives for Cuban Public Health for the Year 2000, which pointed to the need for surveillance and research on the major risk factors associated with population lifestyles. Thus, the first National Survey on Risk Factors and Chronic Diseases was conducted in 1995 to identify prevalence and distribution of the main NCD risk factors in Cuba’s urban population aged ≥15 years. Its results provided a baseline that has facilitated trend detection and evaluation of interventions. In 1996 Cuba’s Ministry of Public Health (MINSAP, the Spanish acronym) established the National Chronic Non-Communicable Diseases Program, with a strong foundation in primary care, hospitals and provincial hygiene and epidemiology centers. The Program combines comprehensive health care actions and collaboration with other sectors.[12,13]
The Second National Survey on Risk Factors and Chronic Diseases (ENFRENT II, the Spanish acronym) was completed in late 2001. For the first time, it included a section on injuries and illnesses and another on health-related quality of life. In 2005–2006, health projections for 2015 were approved, which emphasized reaching a life expectancy at birth of 80 years. The interventions proposed to meet that goal have been affected in recent years by a series of natural disasters resulting in epidemics of communicable diseases (influenza, dengue and others), which affected the National Program’s sustainability.
In 2007, the need to reassess the NCD situation was recognized[14] and the decision taken to implement a different, decentralized surveillance strategy capable of identifying distribution and trends of major risk factors at the municipal level. This in turn would enable closer study, assessment and management of NCDs and their risk factors and identify new opportunities for intervention and future research at the local level. This would all, of course, have to be consistent with Cuba’s public health objectives and carried out in line with MINSAP’s policy of decentralization.[15,16]
This paper describes planning and implementation of NCD risk factor measurement as part of Cuba’s decentralized surveillance system in 12 municipalities during the years 2008–2010.
METHODS
A descriptive cross-sectional study was designed and implemented from 2008 through 2010. The study’s target population consisted of persons aged 15–74 years resident in urban and rural areas in 17 selected municipalities throughout Cuba. Municipalities were selected based on their economic, social or cultural influence on the life of the province, as well as three municipalities with previous NCD-related health intervention projects. The total population in these municipalities is 28.3% of the Cuban population of approximately 11.2 million.[11]
The framework was based on WHO/PAHO Stepwise Approach to Non-Communicable Disease Risk Factor Surveillance (STEPS), which can be adapted to specific economic, infrastructure and logistical conditions. Cuba implemented the instrument’s three steps: questionnaire (step 1), physical measurements (step 2), and biochemical measurements (step 3).[17] The study was led by the National Hygiene, Epidemiology and Microbiology Institute (INHEM, the Spanish acronym), in conjunction with MINSAP experts in health education and research, and with the National Statistics Bureau. A national coordinating team was formed with expertise in NCD control and population surveys. The process was replicated in each province to ensure appropriate oversight and implementation. This was not possible in every municipality because of reassignment of some personnel to other tasks, in Cuba and abroad.
Use of the STEPS questionnaire permitted comparison of resulting data with those from other countries and also within Cuba over time. The questionnaire was adapted to the Cuban context and expanded to include questions about quality of life. Serum creatinine was added to the biochemical measures to determine renal function.[17]
The instrument included:
- general information—address, health care catchment area;
- sociodemographic information—sex, age, education level completed (no formal schooling, primary school, middle school, trades school, middle-level technical training, high school and university), skin color, marital status, main employment, and wages earned in the previous year;
- behavioral measurements—tobacco and alcohol use; diet; physical activity at work, in commuting and leisure activities;
- personal history of diabetes, high total cholesterol and hypertension;
- family history of diabetes, high cholesterol, hypertension, ischemic or hemorrhagic stroke, heart attack and cancer;
- physical measurements—blood pressure and anthropometrics (weight, height, and waist and hip circumference);
- biochemical measurements—fasting blood glucose, triglycerides, total cholesterol and creatinine;
- health-related quality of life—EuroQol instrument using a visual analogue scale for self report of five aspects of health status (mobility, self care, usual activities, pain or discomfort, and anxiety or depression).[18]
Constraints Due to difficulties obtaining a reliable supply of reagents, biochemical measurements were not taken consistently in all municipalities. There were also challenges to determining wages earned by those surveyed, so that part of the analysis was postponed. Several natural disasters hit Cuba and spawned outbreaks of communicable diseases, preventing simultaneous collection of data in all municipalities. The present paper therefore includes only the 12 municipalities where data analysis was complete at the time of writing. These problems may also influence variation in municipal results, which will require local-level analysis.
IMPLEMENTATION
Study plan and implementation In all provinces, meetings were held to provide detailed explanations of the study and local use of its results to provincial (People’s Power president or vice president) and municipal governments. In each municipality, five working groups of health personnel (technicians, nurses, doctors and administrative staff) were constituted, with defined tasks:
- data collection (ten surveyors and two supervisors);
- physical measurements: anthropometrics and blood pressure (ten people, including two supervisors);
- biochemical measurements (three people);
- data management (data entry clerks, epidemiologists and biostatisticians); and
- logistics, including resources and survey organization.
The Provincial Hygiene, Epidemiology and Microbiology Centers (CPHEM, the Spanish acronym), municipal hygiene and epidemiology centers and units, and head nurses in the selected provinces, municipalities and polyclinics worked throughout the organizational phase.
Sample design In each municipality an independent sample was taken, although the design was common to all (except for the municipality of Cienfuegos, which participated in the international project CARMELA [Cardiovascular Risk Factor Multiple Evaluation in Latin America], whose sampling design and basic criteria have been published).[19]
The sample size required was calculated according to expert criteria (see acknowledgments for technical contributions) of approximately 200 individuals in each stratum (age group and sex). To ensure this sample size, allowing for attrition, 220 individuals per stratum were selected. The design, therefore, was equiprobabalistic within each group but not between groups.
Cluster sampling was performed in two stages, stratified by age and sex. Clusters consisted of family doctor-and-nurse practices in the municipality’s health areas; units of analysis were the individuals selected in each practice. There were 12 strata: 6 age groups (15–24; 25–34; 35–44; 45–54; 55–64; 65–74 years) for each sex.
In the first stage, family doctor-and-nurse practices were randomly selected from among all practices in each municipality through systematic sampling; in these practices, a census was conducted of all persons in the age groups of interest. The second stage involved a systematic selection of 220 individuals in each stratum, using fractions equal to 220/number of individuals in the stratum, for a final desired sample size of 2640 for each municipality (with the exception of Cienfuegos, noted above).
Since the sampling was complex (multistaged, stratified and non-equiprobabilistic), a weighting factor was required for data analysis. It consisted of the inverse of the probability of selecting an individual and was calculated by dividing, for each age and sex group, the 2008 population in the municipality by the total number of persons in the sample, so that estimates were representative of all persons in that age and sex group in the municipality.[20]
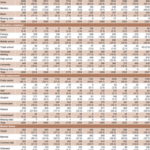
By the time this paper was being prepared, data processing and analysis had concluded in 12 municipalities, whose populations together comprise 20% of the country’s total population (Table 1).
Table 1: Sample characteristics by municipality (n = 2640*)

*Desired sample for Cienfuegos was 2400[20]
Before starting the survey proper, a pilot test was conducted in the 10 de Octubre Municipality in Havana Province (then called City of Havana Province, prior to provincial boundary changes in 2010), to estimate questionnaire completion time and assess comprehension and acceptability. Of the 100 people who were randomly selected, 94 agreed to participate and 6 declined, citing time limitations.
Participation in the survey proper involved a 50–60 minute formal interview, during which respondents were asked to go to the measurement center 48 hours later (or at an agreed-upon time) in a fasting state (written instructions provided). Measurement centers were usually family doctor-and-nurse offices, schools or other suitable buildings in the community, chosen to meet minimal conditions of privacy and comfort and for location as close as possible to the study area, that is, the catchment area of the family doctor-and-nurse office.
Family doctors and nurses facilitated recruitment and trained study personnel in each measurement center, took physical measurements per protocol, and drew blood samples for laboratory testing for glucose, creatinine, and total cholesterol and triglycerides.[21]
Ethics All persons selected were visited at home to obtain written consent to participate, following explanation of the purpose of the survey, importance and benefits of participation, absence of risk, data confidentiality and freedom to opt out without repercussions at any moment should they so desire.
Special care was taken to send participants’ test results via their family doctor and nurse; if any changes requiring medical attention were observed, participants were immediately referred for treatment and followup
Quality control A system of quality control was set in place from the beginning, including detailed protocols and standard procedures for questionnaire administration and anthropometric and laboratory measurements. Three-day sessions were held in 14 provinces to train personnel designated for each of the three functions. A rigorous accreditation step was also set up for quality assurance.
The national coordinating group visited provinces to verify quality on the ground through direct observation of protocol adherence. In two municipalities, the process was interrupted because of organizational problems and reinitiated later when organization met required standards.
Laboratory results were monitored weekly by a national reference laboratory in Havana (at Carlos J. Finlay Biological Products Company). Some 438 health technicians were involved in analyzing samples, which helped increase their scientific–technical preparation in NCD risk factors.
Data management and statistical analysis Data entry used EpiData Version 3.1 software. In each municipality, a supervisor reviewed and then coded data collected daily. At the end of each work day, provincial coordinating team supervisors sent the database by email to biostatisticians in the INHEM national coordinating team, where they again reviewed and corrected the minimum, average and maximum values of each variable. A central database was consolidated for each municipality with an automated validation system for each variable in the questionnaire.
Data were analyzed in each municipality. Means were calculated for continuous variables and percentages for qualitative ones, with 95% confidence intervals, using methods recommended for complex sample analysis, including standard error adjustments.[20]
The population’s sociodemographic characteristics are presented in Table 2. This were consistent with 2002 census data.[22]
LESSONS LEARNED
The planning and implementation processes described here were unprecedented in Cuba and enabled decentralization of NCD risk factor surveillance and prompt use of information generated for decisionmaking in municipalities and provinces. From the research team’s perspective, this is the most important result obtained.
Table 2: Sociodemographic distribution of sample*
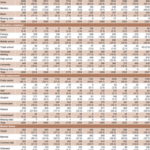
*Percentages were calculated based on net totals (without missing data)
AGU: Aguada CAM: Camagüey CAV: Ciego de Ávila CFG: Cienfuegos HOL: Holguín MOR: Morón MTZ: Matanzas PDR: Pinar del Río SAB: San Antonio de los Baños SCL: Santa Clara STG: Santiago de Cuba YAG: Yaguajay
From the outset, participation of local government authorities was decisive in the process and for establishing accountability for progress in measurements, to ensure timely corrections if necessary.
The survey’s success depended in part on discussion and analysis of data with senior provincial public health authorities and representatives of provincial and municipal governments, as well as members of the National–Provincial Coordinating Group. The results of these discussions informed design of a concrete intersectoral action plan with emphasis on a communications strategy. Participating sectors and institutes included those in education, food and nutrition, sports and recreation, culture, higher education, and the media.
This experience demonstrates the usefulness and feasibility of intersectoral work in implementing NCD risk factor surveillance, as has been found in other countries.[23–25]