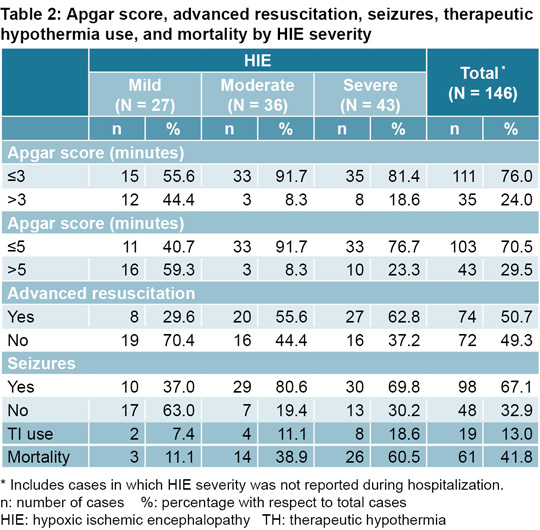
with a score ≤5 at 5 minutes were reported. Of the 146 newborns who presented with HIE, 111 (76%) had an Apgar score of ≤3 at 1 minute of life and 103 (70.5%) ≤5 at 5 mintes of life. Low Apgar scores were much more common in the moderate and severe forms of HIE (Table 2).
Seizures Of the 146 newborns with HIE, 98 (67.1%) experienced seizures. Seizures were also much more common in moderate and severe forms of HIE (Table 2).
Resuscitation according to HIE severity Advanced resuscitation was necessary in 74 newborns with HIE (51%) (Table 2). The likelihood of advanced resuscitation obviously increased with HIE severity. Of the 20 newborns with moderate HIE who received advanced CPR, 9 (45%) required cardiac massage and 4 (20%) required vasoactive medication. Of the neonates with severe HIE, 27 (63%) required advanced CPR, of which 22 (81%) required cardiac massage and 11 (41%) required medication. Only 11% of newborns were resuscitated with 21% FiO2 and 40% were resuscitated with 100% oxygen. FiO2 data was not reported for the remaining 49%.
Therapeutic hypothermia Only 19 of the 146 newborns with HIE (13%) were treated with TH (mild HIE: 2, moderate HIE: 4, severe HIE: 8, with unknown severity: 5) (Table 2). Of those treated with TH, 75% received body cooling and 25% received selective brain cooling. It is obvious that, regardless of the severity of HIE, TH use is infrequent.
Mortality Among the 2876 newborns, mortality reported was 11% (310 newborns) while mortality in the 146 newborns with HIE was 42% (61/146), which is positively correlated with HIE severity. Of the 61 newborns with HIE who died, 37 cases (60.7%) were directly attributable to HIE, regardless of severity. In the remaining 24 (39.3%), death was attributed to sepsis, meningitis, respiratory failure, hypoxemia, kernicterus and other causes.
DISCUSSION
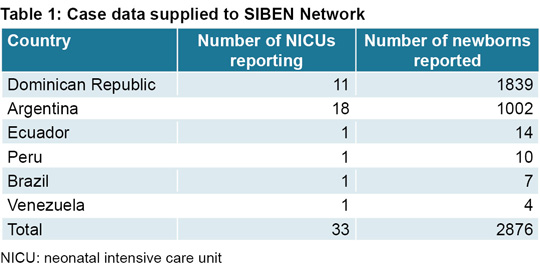
HIE is a neonatal condition that results in high mortality and severe neurological sequelae.[1–3] In this study, HIE prevalence in newborns at ≥36 weeks GA admitted to SIBEN Network centers was 5.1% with a mortality rate of 42%, almost four times that of non-HIE newborns at the same GA reported to the Network. Although HIE severity was not reported for all newborns, in 54% of reported cases it was either moderate or severe. These data do not represent all of Latin America nor the reality of each country, as our sample corresponds to voluntary reporting made by only some of the neonatal units within the region. However, even with the aforementioned limitations of our sample, these data reflect a situation demanding urgent action.
TH has proven benefits for newborns with HIE,[10,15,17–23], among which the reduction in mortality or neurodevelopmental alterations at 18 months stands out with a relative risk (RR) of 0.75, 95% CI (0.68–0.83).[17] TH has few side effects and its implementation is relatively simple. However, TH was only used in a small number of newborns with HIE in this sample, and it remains unavailable in many centers throughout the region. In the SIBEN Network during the study period, 87% of neonates who presented with HIE did not receive TH, and of the 79 reported with moderate or severe HIE, only 12 (15%) had access to TH. It is highly probable that the mortality rate in these newborns would have been lower if TH had been available and applied. Even though we do not know the neurological evolution of these newborns after discharge, evidence shows that TH leads to reduced rates of major disability associated with HIE and therefore better long-term neurological outcomes.[17]
As is the case with other health indicators, no Latin American countries present national data on prevalence and clinical evolution of newborns with HIE, with the exception of Cuba, where HIE frequency in 2017 and 2018 was comparable to rates in high-income countries. HIE mortality rates in Cuba of 12% and 17% (for 2017 and 2018, respectively) cannot be stratified by HIE severity since, as of this writing, the Cuban national registry has not yet recorded this data for later analysis. Unlike Latin America, other regions have working groups that track information related to HIE incidence, its severity, conditions available for comprehensive care and the TH implementation.[24,25] In a cross-sectional study conducted in 57 Spanish hospitals, 95% of those surveyed used servo-controlled total body cooling and had established protocols specific to HIE patient care.[26]
This study does not include an analysis of the use of oxygen in advanced resuscitation procedures. The universal recommendation is to use ambient air (21% FiO2). However, this was the case in only 11% of newborns resuscitated in this sample. Some 40% were resuscitated with 100% oxygen, despite ample evidence advising against this practice and the damage the hypoxia-reperfusion-hyperoxia cycle can have on the brain.[27–31]
Any process aimed at improving quality of care for newborns with HIE must be based on reliable information. This is the first study involving Latin American countries that provides data on this important problem. Comprehensive care of newborns affected by HIE is multi-faceted and must include the availability of adequate resuscitation with trained personnel in the delivery room, avoiding inappropriate use of oxygen; rapid clinical diagnoses; the ability to assess HIE severity, and use of previously validated care protocols. Timely care for families is essential, as is TH provision in the NICU or potential for patient referral to a center capable of providing TH within the first six hours of life. Finally, given the consequences HIE has for neurodevelopment and quality of life for both children and their families, specialized followup programs should be established to identify and treat neurodevelopmental issues in a timely manner, and offer support and guidance to families.[32]
CONCLUSIONS
Hypoxic ischemic encephalopathy is a neonatal condition responsible for high mortality rates and severe neurological sequelae. HIE prevalence in this study was 5.1%, with an overall mortality rate of 42%. Despite the fact that HIE was graded as either moderate or severe in 54% of cases, therapeutic hypothermia was not performed on 87% of neonates presenting with HIE. This is the first study published containing multicenter data on HIE in Latin America, and it demonstrates an urgent need for the implementation of programs to improve the quality of care available for newborns with neonatal encephalopathy.
ACKNOWLEDGMENTS
We are grateful to the following specialists for collecting and reporting data to the SIBEN Network: Maria Rosa Frias, Diego Depietro, Ignacio Sosa, Belen Falco, Maiara Celiz, Segundo Jaime Sánchez, Anabell Pereira, María Elisa Villoldo, Carolina Pinto, Cristiane Ribeiro, María Rosa Gonzalez, Amantina Peña, Sujey Vargas, Candelaria Nuñez, Maria Victoria Vulcano, Arielina Felix, Maritza Ramos Medina, Nadia Rosario, Taína Malena, Mónica Menzio, Veronica Favareto, Ana Medina, Odris Tejera and Joselyn Acosta.