David, Daniel, and Diego were born at 32 weeks via caesarean section in Cuba’s eastern province of Granma—they weighed between 1520 and 1780 grams each. Their mother, Dayanis Díaz, wasn’t producing enough milk for her triplets and just 24 hours after birth, they were being fed with pasteurized milk from the hospital’s breast milk bank. For a month, the three Ds were nourished with this donated milk until Dayanis started lactating sufficiently, at which point her own milk supplemented that from the milk bank. Shortly thereafter, the triplets were discharged, weighing in at 2500 grams. “Every day I give thanks for the patience, understanding and support of the milk bank team,” says Dayanis.
In Santiago de Cuba, Jorge Rodríguez was born prematurely, with low birth weight, and was in critical condition for the first several days. Tragically, his mother died giving birth and his neonatology team began nourishing him with milk from the local milk bank. After three months, he was healthy enough to go home “thanks to the breast milk bank and the voluntary spirit of the donors. We are very grateful,” says Jorge’s father.
Arlet Tito gave birth to twins at the tender age of 14. One of the babies died and the other, weighing just 900 grams, suffered from prenatal asphyxia. Traumatized, Arlet wouldn’t nurse her surviving son, who began receiving donated milk from the breast milk bank in her province of Guantánamo. As her son gained weight, the bank’s specialized breastfeeding support team began talking with Arlet about the benefits and importance of nursing. The message hit home, and she eventually became one of the banks most prolific donors—depositing up to seven liters a month—as well as a health promoter, giving talks about the benefits of breastfeeding to expectant mothers in the maternity wards of Guantánamo’s Agostinho Neto Provincial Clinical-Surgical Teaching Hospital.
The three D’s, Jorge, Arlet and her son and many other mothers and children like them, are beneficiaries of Cuba’s Human Breast Milk Bank program, administered by the country’s Ministry of Public Health (MINSAP, the Spanish acronym) with financial support from UNICEF and other international organizations, and technical and training support from Brazil’s Oswaldo Cruz Foundation (FIOCRUZ). Part of the multi-year, intersectoral program entitled Support for the Fight Against Anemia in Vulnerable Groups, the milk banks are one of the pillars of the strategy to combat anemia, but also to raise awareness and promote breastfeeding among new mothers.
The Problem: Anemia
Iron-deficiency anemia is considered a national health priority in Cuba—especially among the most vulnerable, including pregnant women, newborns, and children under five years old. National studies show that 25-35% of women of reproductive age[1] and 28% of pregnant women in their third trimester have iron-deficiency anemia,[2] while 37.5% of children aged 6–35 months suffer from anemia.[3] A diet low in iron has been identified as the primary cause, prompting design and implementation of several national programs.
As early as 1987, public health authorities in Cuba had developed policies to reduce the prevalence of anemia, particularly in the most vulnerable populations and regions, such as the country’s five eastern provinces: Las Tunas, Holguín, Granma, Santiago de Cuba and Guantánamo. In 2008, these policies were converted into a national, multisectoral strategy that included distribution of iron-fortified foods and supplements, beefed-up nutritional guidelines and education, diversification of iron-rich food production and greater iron-deficiency surveillance. Under this program, known as the Comprehensive Plan for the Prevention and Control of Iron-Deficiency Anemia in Cuba, the highest-risk groups were prioritized and anemia prevention, rather than control, became the cornerstone.[4]
UNICEF, joined by other UN agencies, including WHO/PAHO and the UN Development Programme (UNDP) has supported Cuba’s national strategy to prevent anemia through the subprogram Support for the Fight against Anemia in Vulnerable Groups. This effort focuses on Cuba’s five eastern provinces and Pinar del Río in the west, where drought, hurricanes, food insecurity, and other determinants conspire to make these areas more vulnerable. Indeed, the prevalence of anemia in infants between 6 and 11 months in the eastern region is classified as severe, according to WHO guidelines,[5] which consider breast milk “the first line of defense against infection and the only food capable of satisfying all the nutritional and immunological needs of newborns, through six months.”[6]
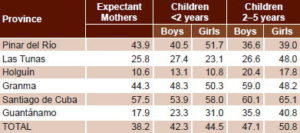
Anemia Prevalence (%) among Expectant Mothers & Children in Six Cuban Provinces, 2010
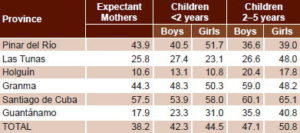
Source: Nutrition and Food Hygiene Institute, MINSAP
The Strategy: Breastfeeding & Human Breast Milk Banks
Containing all the hormones, micronutrients, growth factor, proteins, enzymes, nucleotides and other properties necessary for proper growth and development, human breast milk is recognized as the most complete food for the earliest stages of life. The iron in breast milk is also more easily absorbed by infants than that found in cow’s or other milk formulas. For optimum growth and neurodevelopment, international guidelines recommend exclusive breastfeeding from birth through six months, and supplemented by other foods through 24 months. Major causes of anemia in children younger than 24 months, meanwhile, include premature birth, low birth weight, lack of the quantity and quality of micronutrients needed for healthy growth, and recurring infections. For these reasons, and because nursing is a practical, cost-effective approach in resource-scarce settings like those on the island, public health authorities developed two related initiatives: the National Breastfeeding Program and human breast milk banks. These are administered by MINSAP and fall under the umbrella of the country’s National Maternal-Child Health Program (PAMI, the Spanish acronym).
“The two work together to promote the health and social benefits provided by nursing, to help us achieve the goal of exclusive breastfeeding for the first six months, and to have a positive impact on these infants’ health,” says Dr Pablo Carlos Roque, National Coordinator of the two programs. Specifically, these initiatives aim to:
- Increase the percentage of women breastfeeding exclusively for the first six months of their child’s life up to two years with supplemental food;
- Reduce morbidity and mortality among very low birth weight babies;
- Increase neonatal survival rates;
- Maintain the country’s low infant mortality rate; and
- Reduce under-five mortality.
To achieve these goals, policies were coordinated across complementary programs and intersectoral cooperation promoted; new nutritional guidelines were formulated for the first two years of life; research was encouraged into causes and effects of neonatal, infant, and under-five mortality and the impact breastfeeding has on these indicators; and technology and knowledge were shared concerning breast milk banks and lactation in general. According to Dr Gabino Ernesto Arman, head of PAMI in Pinar del Río Province, “we are working hard to raise awareness about breastfeeding, so that Cuban mothers nurse to 24 months. It’s a challenge because after 6 months, when their babies are growing and developing well, they tend to stop breastfeeding.” The need was urgent: results of a 2010–2011 study found that only 49% of Cuban mothers breastfed exclusively through 6 months, with that figure falling to 17% at 20–23 months.[7]
Fortunately, Cuba already had many efforts in place to support these goals, including the nationwide skin-to-skin or ‘kangaroo care’ program, launched at Pinar del Río’s Abel Santamaría Cuadrado Provincial Clinical-Surgical Hospital in 1994. This was complemented by UNICEF accreditation of 57 Cuban hospitals as ‘Mother-and-Baby Friendly’, meaning that a high percentage of mothers are nursing upon discharge.
The scientific evidence about the benefits of breast milk, especially for high-risk newborns, is irrefutable. But what can be done when a mother can’t (or won’t) nurse? The answer came in 2004 when a team of Brazilian doctors visited Cuba to present on human breast milk banks at the International Pediatric Congress. Findings from Brazil—the global leader in breast milk banks, with a network of 256 across the country—showed that these depositories are an economically sustainable and highly effective strategy for reducing neonatal mortality and morbidity related to infection, anemia and very low birth weight.[8]
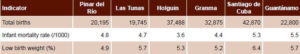
Selected Indicators for Six Provinces with Human Milk Banks, Cuba 2010–2012
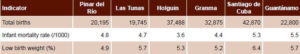
Sources: PAMI, MINSAP
Energized by the Brazilian experience, Cuban specialists piloted a human breast milk bank in Havana’s 10 de Octubre municipality in 2005. “It was a small, modestly financed project, but counted on trained and highly dedicated staff. Its results showed us how effective the approach could be,” says Dr Roque. That same year, Cuba signed the Brasilia Declaration issued at the Second International Congress on Human Milk Banks, which committed signatories to promote, protect and support breastfeeding, while recognizing breastfeeding as a key strategy for achieving several of the UN’s Millennium Development Goals and reducing neonatal mortality. From these initial steps, Cuba became wholly dedicated to setting up breast milk banks on a national scale.
In 2006, 30 Cuban specialists—the majority neonatologists—received technical training in breast milk collection, processing and distribution from the Brazilians. In 2007, Cuba and Brazil/FIOCRUZ signed a bilateral agreement, Technical Support for the Implementation of Breast Milk Banks in Cuba, and the island nation joined the Iberoamerican Network of Breast Milk Banks. In 2010, UNICEF provided three years of funding to train personnel, equip, and launch a small network of breast milk banks in Cuba. Complementary funds were provided by the Spanish government’s Fund for Reaching the Millennium Development Goals.
From Breast to Baby: How the Banks Work
Since the program was designed to prioritize the most vulnerable, the first six breast milk banks established under these agreements were set up in Mother-and-Baby Friendly Hospitals in Pinar del Río, Holguín, Granma, Santiago de Cuba, Guantánamo, and Granma provinces between 2011 and 2012. The highest-risk patients were first in line for the donated milk. These include babies born at 34 weeks or earlier; those with very low birth weight (less than 1500 grams); infants who have undergone digestive tract surgery; babies born with asphyxia; and those in neonatal intensive care units for other reasons.
Educational activities related to breastfeeding—incorporating role-playing, question-and-answer sessions, and demonstrations—begin with expectant mothers during regular visits to their family doctors and obstetricians, and at maternity homes (specialized centers for high-risk pregnancies; see MEDICC Review, July 2011). These activities continue on maternity wards to promote breastfeeding exclusively through six months. In the half a dozen hospitals with breast milk banks, these efforts are also designed to motivate new mothers to become donors.
“Donating milk is voluntary, and while some health professionals were skeptical that we’d be able to find donors, Cubans have a lot of solidarity and we believed it would be hard for a Cuban woman—for any woman, actually—to say no when we explained that their milk could help save the life of a newborn child,” says Dr Roque. Angie Fernández, a 31-year-old donor in Pinar del Río is case in point. When her son Tiago José was born in mid-2013, she was determined to breastfeed him exclusively for six months; she also was eager to become a donor when she learned about the properties of breast milk and how hers could help heal a sick child. “I was really motivated to become a donor when my doctor told me about the milk bank. So I donated for six months until my milk ran out. Then I decided to become a promoter, to help convince other women to donate their expressed milk to the banks,” she told MEDICC Review during a session at the local maternity home.
Each prospective donor begins with a thorough clinical exam, including a series of blood tests (repeated every three months), complemented by an in-depth interview with one of the breast milk bank specialists, to assess her eligibility. Consent forms are signed and then her preparation begins (hand- and breast-washing with soap and water, covering her hair, wearing a surgical mask). Her teachers demonstrate manual extraction techniques and explain the process for assuring the sterilization of jars and an unbroken cold chain. A specially-trained health professional from the local breast milk bank visits the donor’s home to assess cleanliness, as well as to perform check-ups on both mother and baby to see that they are both healthy and well nourished; only mothers of those infants developing according to the country’s child growth and development standards are permitted to donate. These at-home visits are repeated whenever warranted, for instance if a mother’s donations are contaminated upon reception at the bank.
In Cuba, unlike in many other countries, donors are not paid or otherwise compensated for their milk, since the Brazilian experience showed that women with economic needs would sell their milk before providing it to their own child. The voluntary model works in Cuba for a variety of reasons, according to the banks’ professionals, including the individualized, at-home care and attention provided by breast milk bank professionals to nursing mothers.

Angie Fernández, encouraging expectant mothers to donate their milk at a Pinar del Río maternity home. /E. Añé
The expressed milk is kept in the donor’s freezer until collected by the bank’s team, equipped with coolers for this purpose and transported to the hospital, where the unprocessed milk is deposited in special deep freezers. Within 7–15 days, these donations undergo multi-step quality control, pasteurization using the Holder method,[9] classification (there are over a dozen types of breast milk, each with different properties), and a last microbiological analysis to assess whether the milk is certified for distribution. The banks operate 8–12 hours a day (the Guantánamo bank is 24 hours) and the milk is processed once or twice a week, depending on volume of donations, demand and the most rational use of resources for each hospital. All breast milk banks in Cuba are located next to the hospital’s neonatology wards and are designed for a seamless flow between intake, processing, storage and distribution of donated milk.[10]

Milk donations frozen in Pinar del Río’s breast milk bank. / E. Añé
Each step follows strict international and domestic biosecurity standards, monitored by the hospital’s maternal-child health and nursing departments, plus the Hygiene and Epidemiological Departments of the individual hospitals and their provincial-level counterparts. Furthermore, MINSAP’s Department of Environmental Health visits and inspects each bank periodically. All equipment, including thermometers, timers and microbiological control instruments, are tested and calibrated by national metrological authorities.
“Once our bank was up and running and we started seeing positive results, word got out and the demand for donated milk skyrocketed,” says Dr Liliana Rivera, a neonatologist and director of the Gotita de Vida human breast milk bank at Pinar del Río’s Abel Santamaría Cuadrado Provincial Clinical-Surgical Hospital. “So we went into the community and began actively recruiting donors.” Between July and September, 2011, the Gotita de Vida bank collected 9.7 liters of milk from 47 donors; between January and March, 2013, the bank had collected 140.2 liters from 424 donors.[6] “If we received 20 liters of donated milk a week, that would be ideal,” says Rivera, “but we’re getting about half that on average. There’s still a lot of work to do.”
Results, Challenges & Lessons Learned
Although the program is just a few years old and the impact has yet to be fully evaluated, initial results are positive. Very low birthweight babies receiving donated milk are gaining 50 grams per day, which means not only stronger babies, but also shorter stays in intensive care, with fewer infections and a decrease in use of antibiotics. This is important in a resource-scarce setting like Cuba, since it translates into lower costs related to hospital stays, and less procurement and administration of medicines, supplemental nutrients and milk substitutes.
Human Breast Milk Bank Collection & Processing Results in Six Cuban Provinces, 2011–2012

Source: Maternal–Child Health Program, Human Breast Milk Bank program, MINSAP
Infant mortality has dropped in four of the six provinces with breast milk banks, and nursing by new mothers has increased in all of them. Furthermore, breast milk bank specialists and promoters (i.e. current and former donors), have held over 3,000 educational workshops and talks, conferences about breastfeeding and directly counseled more than 8,300 new mothers who have experienced trouble nursing. Over the course of the program, only 2% of raw milk and 1.8% of the processed milk collected has been discarded due to contamination or poor quality.[6]
Importantly, this program has also shown how different ministries, Cuban families and communities can work together in an intersectoral way to improve population health. Close coordination is required among several entities to ensure proper collection, maintain the cold chain, perform the necessary tests and assure quality control. This includes the banks and hospitals themselves, transportation, sports, nutrition and hygiene institutes, ETECSA (the telecommunications company), and metrological authorities, among others.
Challenges remain. Dr Rivera notes: “As I said, we still have a lot of work to do—especially if we expect to reach the goal of having a breast milk bank in every Cuban province.” One challenge looming large is how to increase supply to meet demand, compounded by the perennial lack of financial and material resources on the island. Expressed milk, for instance, is stored by the donor in wide-mouthed glass jars with plastic tops—simple items that are, nevertheless, uncommon in Cuba. Until now, these have been imported, an expensive and slow proposition. While there are enough jars for the six banks at current donation levels, expanding the program will require domestic production of these jars.
Program designers also explain that until all the material and human resources are in place, they cannot promote the program as aggressively as they would like. In 2014, these resources have been procured to open one more bank—in Camagüey Province—where health authorities are preparing to roll out a media campaign about the breast milk bank program, anticipating it will motivate new donors. This will require coordination between different sectors participating in the program, training of more staff, and meticulous control of resources.
Research and analysis of the breast milk banks’ impact is also needed to provide evidence of their effectiveness. This is important to allow comparisons between those provinces with a bank and those without, and if results are positive, to attract more funding as well.
Other areas where experience shows room for improvement include the testing, installation and maintenance of the banks’ equipment; providing for fluctuations in staff who may be absent due to sickness or travel; streamlining bureaucratic processes for ensuring transportation for donation collection; and freeing up health professionals from other duties so they can dedicate more of their time to the breast milk bank.
Final Considerations
Breast milk has proven a cost-effective and efficient method for providing all the nutritional and immunological properties a baby needs. Indeed, it has no substitute—nothing has higher quality, consistency, temperature, composition and nutritional balance than breast milk.
When a mother cannot nurse her baby, the milk from another lactating woman is the next best thing and has shown to contribute to healthy growth and development of at-risk infants. Human milk banks are especially effective in resource-scarce settings with coordinated, continuous support from local and national governments, international organizations, the surrounding community and individual donors.
References

- Pérez R. The public health sector and nutrition in Cuba. MEDICC Rev. 2009 Fall;11(4):6-8.
- Proyecciones de la Salud Pública en Cuba para el 2015. Havana: Ministry of Public Health (CU); 2006. p 25.
- United Nations Children’s Fund; Nutrition and Food Hygiene Institute (CU). Intervenciones para la prevención de la anemia por deficiencia de hierro en infantes menores de tres años. Puré de frutas fortificados. Experiencia cubana. Havana: Food Industry Research Institute (CU); 2011. Cuba.
- This comprehensive program evolved from the National Plan for the Prevention and Control of Iron Deficiency and Anemia in the Cuban Population, established in 1997. Ministry of Public Health (CU). Plan integral para la prevención y el control de la anemia por deficiencia de hierro en Cuba. Havana: Ministry of Public Health (CU); 2008. Spanish.
- UNICEF-WHO. Iron deficiency anemia. Assessment, prevention and control. A guide for program managers [Internet]. Geneva: WHO; 2001 [cited 19 January 2014]. Available from: www.who.int/nutrition/publications/en/ida_assessment_prevention_control.pdf
- Ministry of Public Health (CU). Bancos de leche humana en Cuba. MINSAP-UNICEF-CUBA(CU); 2013.
- Ministry of Public Health (CU). Encuesta de indicadores múltiples por conglomerados (2010/11). Havana: National Health Statistics and Medical Records Division (CU); UNICEF; 2012. Spanish.
- Coutsoudis I, Adhikari M. Nair N, Coutsoudis A. Feasibility and safety of setting up a donor breastmilk bank in a neonatal prem unit in a resource limited setting: An observational, longitudinal cohort study. BMC Public Health. 2011 May 20;11:356.
- Landers S, Updegrove K. Bacterial screening of donor human milk before and after Holder pasteurization. Breastfeed Medicine. 2010 Jun;5(3):117–21.
- The exception is in Granma, where the bank is located 1.5 miles from the hospital, since appropriate space was unavailable in the hospital itself.