INTRODUCTION
AIDS is a leading cause of death in the Caribbean, where HIV prevalence is high.[1] However, Cuba maintains a prevalence of 0.1% in the population aged 15 to 49 years,[2] considered very low, even though incidence has increased in recent years.[1] From 1986 through 2009, 12,217 persons were diagnosed with HIV infection; 4938 (40.4%) developed AIDS; and 2127 (17.4%) died from AIDS. The epidemic has affected mainly men (81% of total); and men who have sex with men (MSM) account for 72% of all HIV diagnoses.[2]
From 1986 through 1993, HIV-positive Cubans were admitted and treated exclusively at 14 sanatoria established in various provinces,[3,4] a strategy that provoked considerable controversy.[5–8] Opportunistic infections and other HIV-associated conditions were treated at the Pedro Kourí Tropical Medicine Institute (IPK, its Spanish acronym). At the end of 1993, an ambulatory program was established,[3] and since 2006, major effort has gone into strengthening comprehensive decentralized care for HIV/AIDS patients at the primary health care level.[2]
In 1987, zidovudine (AZT) was recommended as monotherapy for all persons with AIDS in Cuba. In 1996, the Ministry of Public Health (MINSAP, its Spanish acronym) acquired antiretroviral drugs (ARVs) for all children with AIDS and their mothers (zidovudine, lamivudine, and indinavir). Since 1997, HIV-positive pregnant women receive AZT to prevent mother-to-child transmission. In 1998, international donations of zidovudine, lamivudine, didanosine, zalcitabine, stavudine, saquinavir, ritonavir, and indinavir enabled a group of persons with AIDS to begin receiving these ARVs. In mid-2001, several domestically-produced ARVs were introduced (zidovudine, lamivudine, stavudine, didanosine, and indinavir, followed a few months later by nevirapine), which were first prescribed for people diagnosed with AIDS or who were critically ill. In 2002, the treatment group was enlarged, and since 2003, there has been 100% coverage for all who require it, as defined by: CD4 cell count <350 cells/mm3, viral load >55,000 copies/mL, and presence of an opportunistic infection.[3] Later, drug combinations were expanded with support from the Global Fund to Fight AIDS, Tuberculosis, and Malaria.[4] At the end of 2009, 5034 persons with HIV/AIDS were receiving ARVs.[2] Several studies have shown that this use of antiretroviral therapy (ART) in Cuba has increased survival time and reduced opportunistic infections and AIDS deaths.[2,3,9,10]
Congenital esotropia may be accompanied by amblyopia (reduction in uni- or bilateral best corrected visual acuity not attributable to structural abnormality of the eye or posterior visual pathway), thus establishing the sensory nature of the impairment.[14] Ocular misalignment is in fact the main cause of amblyopia. Constant esotropic deviations, rather than alternating ones, are the fundamental cause of strabismic amblyopia.[15] Amblyopia is classified according to best corrected visual acuity (VA): mild (0.9–0.6), moderate (0.5–0.3) and severe (0.2–0.05).[15] Some authors do not explicitly define mild amblyopia and others ignore it, referring only to moderate and severe amblyopia.[15]
ART adherence is a key factor in disease course in persons with HIV/AIDS.[9–11] Adherence of ≥95.0% can achieve suppression of viral load to undetectable levels, improve immune system function,[9,12,13] and reduce AIDS-related morbidity and mortality.[14] In contrast, nonadherence can lead to treatment failure, development of ARV-resistant viral strains,[15] progression to AIDS[16] and death.[17] Factors related to patient characteristics, social environment, treatment type, the disease itself, and the health care team can influence degree of treatment compliance.[11,18–21]
In Cuba, clinicians have customarily explored treatment adherence through general patient interviews and monitoring of CD4 lymphocytes and viral load. However, some authors consider this method imprecise.[22,23] Although ART outcomes—fewer opportunistic infections, longer survival time, and fewer deaths—could lead to a conclusion of optimal adherence in Cuba,[3] no national study has been carried out to measure adherence.
The objective of this study is to determine high adherence and its predictive factors among Cuban HIV-positive individuals receiving ART.
METHODS
A cross-sectional study was done of 1986 HIV-positive individuals receiving ART in 2006. A stratified random sample was used, based on province of origin, sex, and treatment setting (outpatient care or sanatorium). The number of participants in each stratum was selected with probability proportional to its size. Participants in each stratum were selected by simple random sampling from the national list in SIDATRAT, a computer program designed by IPK for monitoring ART.
A minimum sample size of 694 individuals was determined using Epi Info 6.04 (expected prevalence of high adherence: 50%, given that there were no prior studies on ART adherence in Cuba; margin of error: 3%; confidence level: 95%). Sample size was increased by 25% to 867, to allow for refusals to participate and people who were sick, hospitalized, convalescing, away from their province, or deceased. General patient data were obtained from SIDATRAT.
Recruitment was limited to participants aged >15 years and who had been receiving ART for at least six months. The ethics committee at IPK, where all these patients were regularly seen, approved the study protocol. Informed consent was obtained from all participants.
Those selected were given a self-administered, anonymous, structured questionnaire. Respondents with a low educational level were assisted by trained personnel.
The questionnaire was developed based on a review of medical literature reporting relevant survey tools,[9,11,24–31] results of focus groups with patients and professionals, and interviews with AIDS experts. Questionnaire development included a pilot study with persons with HIV/AIDS who attended the IPK outpatient clinic; pilot results were analyzed by AIDS experts. Responses used a 5-point Likert scale, with a Cronbach’s alpha of 0.93, indicating high internal consistency. The questionnaire took approximately 15 minutes to complete. Interobserver reliability and concurrent validity were considered acceptable.
Questionnaire items were grouped by: 1) memory—ability to remember to take medications on schedule; 2) quality of communication with the physician at the specialized HIV/AIDS clinic; 3) quality of communication with family doctor; 4) support from and quality of communication with family; 5) support from and quality of communication with friends and classmates or co-workers; 6) self-efficacy—feeling capable of complying with treatment requirements; 7) commitment to complying with prescribed treatment; 8) agreement with positive opinions among persons with HIV/AIDS in Cuba regarding treatment effectiveness, trust in physicians, and confidence in the health system; 9) treatment compliance on each of the three days and in the week preceding questionnaire administration; and 10) compliance with nutritional requirements on each of the three days and in the week preceding questionnaire administration.
Each patient was asked for information on: 1) sociodemographic characteristics (age, sex, educational level, province of residence); 2) HIV (year of diagnosis, care setting—outpatient or sanatorium); and 3) treatment (years of ART, changes in drug combinations, names of drugs in current combination, number of doses daily, and number of tablets daily).
Adherence based on self-reporting of number of doses taken on each of the three days and in the week prior to questionnaire administration[25,29,32–35] was recoded into five categories:
- perfect adherence (100%),
- good adherence (95.0–99.9%),
- moderate adherence (80.0–94.9%),
- poor adherence (1.0–79.9%), and
- treatment drop-out (<1.0%).[35,36]
A participant was considered highly adherent if reported adherence was good or perfect (≥95.0%).[36]
Data analysis was done using SPSS 11.5 software. Contingency tables were constructed and data described using absolute and relative frequencies. The chi-square test of independence was used to assess possible associations between patient classification as adherent or nonadherent and other study variables. The reasons most frequently mentioned by individuals whose adherence was poor or who dropped out of treatment were listed.
After using the Spearman correlation coefficient to test for multicollinearity (among sociodemographic variables, and variables regarding HIV and treatment; memory; relationship with specialist clinical physician; support of family, friends, classmates and coworkers; self-efficacy; commitment to treatment; and agreement with positive opinions among persons with HIV/AIDS about confidence in treatment), logistic regression models were constructed to simultaneously evaluate above factors associated with high adherence.
To gain efficiency and clarity in the interpretation of results, continuous variables—relationship with specialist, with family, with friends, self-efficiency, commitment, agreement with circulating opinions, and memory—were transformed into dichotomous variables, using the median as the cutoff point.[37] Values above the median were considered adequate or functional, using the nonfunctional values as reference for analysis. Categorical values were converted into dummy values, taking the first value as the reference category. The Hosmer-Lemeshow test was used to analyze model fit[38] and the model constant adjusted.
RESULTS
The response rate was 97.7% (847/867). Most interviewees (97.8%) self-administered the questionnaire; a small group (2.2%) with low educational level received assistance from trained personnel.
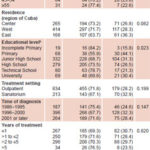
Mean respondent age was 35.8 years, and 77.6% were men. Distribution by region of residence was as follows: 19.8% from the Eastern region (provinces of Granma, Guantánamo, Holguín, Las Tunas, and Santiago de Cuba); 31.3% from the Central region (provinces of Camagüey, Ciego de Avila, Cienfuegos, Sancti Spíritus, and Villa Clara); and 48.9% from the Western region (provinces of Havana, Havana City, Matanzas and Pinar del Río). With regard to educational level, 8.1% had completed university studies, 9.4% technical level studies, 32.9% high school, 39.2% junior high school, and 8.0% primary school, while 2.2% had not completed primary education. Of the total, 25.1% were inpatients in a sanatorium, and 74.9% in ambulatory care.
Diagnosis occurred from 1986 through 1995 in 22.1% of respondents, from 1996 through 2000 in 46.7%, and in 2001 or later in 31.2%. Mean length of time on ART was 2.3 years. ART regimen had changed for 42.6% of respondents. Mean number of tablets taken daily was 12.8; 43.3% took medication twice a day; 16.0%, three times a day; and 40.7%, four or more times a day.
Perfect adherence was reported by 62.6% of respondents; good by 8.0%; moderate by 14.1%; poor by 13.3%; and 2.0% had dropped out of treatment. Thus, 70.6% of study participants were considered highly adherent. Bivariate analysis did not find significant differences between highly adherent and less adherent respondents with regard to sex, region of residence, treatment setting (sanatorium or outpatient), time of diagnosis, or years in treatment. Adherence decreased as number of tablets (p = 0.046) and doses per day (p = 0.050) increased (Table 1).
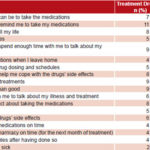
The five most frequent reasons mentioned by respondents whose adherence was poor or who dropped out of treatment were: the attending physician did not understand how hard it can be to take the medication; friends and co-workers did not remind them to take it; they didn’t feel they could take it life-long; the treatment interrupted daily activities; and friends, classmates and co-workers did not spend enough time with them to talk about the illness and treatment (Table 2).
Using the Spearman rank correlation coefficient, multicollinearity was found between the number of tablets daily and the number of doses daily (Spearman coefficient 0.823, p<0.001), so number of doses was dropped from the model. The Hosmer-Lemeshow goodness-of-fit test for the logistic regression model showed that it can be considered acceptable with no evidence of an important difference between predicted and observed results (χ2 = 7.053, gl = 8, p = 0.531).
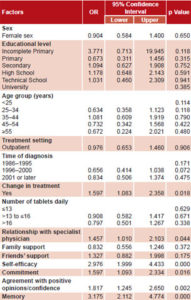
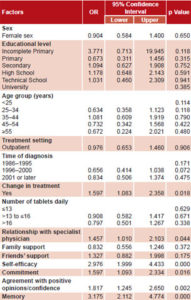
Change in treatment increased the probability of high adherence 1.6 times and supportive communication with a specialist physician 1.5 times. Good memory, self-efficacy, commitment, and agreement with positive opinions on confidence in doctors and health system increased probability of high adherence 3.2, 3.0, 1.6 and 1.8 times, respectively (Table 3).
DISCUSSION
As in other countries, in Cuba the use of ART in HIV-positive individuals has led to a decrease in opportunistic diseases and deaths from AIDS.[3,8] This achievement requires a high degree of adherence to treatment. A limitation of this study is that it is cross-sectional; therefore, the temporal relationship among variables studied is unknown and associations observed cannot be interpreted as causal.
Furthermore, the number of years of treatment studied is small, since ART has been guaranteed for all persons needing it since 2003, and our study was carried out in 2006. However, the research allows us to hypothesize about factors that may be associated with adherence.
Table 1: Characteristics of study participants and high adherence to antiretroviral therapy (n=847 except as noted)
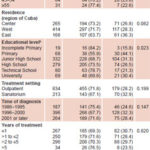
ap <0.001 bp <0.05 c Data unavailable for 11 patients
According to several authors, determining adherence through patient self-report is useful,[9,37,39,40] reliable,[41] and correlates well with virologic response.[36] Others are more cautious about reliability, noting that good adherence is socially acceptable and respondents may tend to exaggerate compliance.[32,36] In this study, 70.6% of patients were highly adherent. Overestimate for the reasons above cannot be ruled out.
Table 2: Participant self-reported reasons for poor adherence (n=113) or treatment drop-out (n=17)
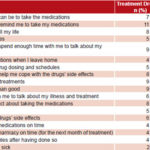
Table 3: Logistic regression model for sociodemographic variables and factors associated with ART adherence of ≥95% (n=847)
Adherence measurement methods vary widely, and thus produce results difficult to compare. For example, percent of “adherent persons” has been reported in Brazil as 63.1%[42] and 56.9%;[43] in Italy 57%;[44] in France 29.1%[45] and 55–60%;[46] in South Africa 93.6%;[47] in Botswana 54%;[48] in Uganda 89%[49] and 85%;[50] in Thailand 69%;[37] and in the United States 50%.[13]
New treatment regimes, available primarily in developed countries, with fewer numbers of tablets and doses daily, have contributed to increased adherence where these are available, although these studies such as those above indicate that adherence remains a problem even in some of those countries.
In our study, no association was found between adherence and sex, which coincides with some investigations,[24,37,43,51] but not others.[18,20,42] Lack of significant differences in adherence among regions in Cuba may be explained by existence of a national HIV/AIDS program with a unified approach. However, possible differences at the provincial and municipal levels should be explored to optimize intervention effectiveness in improving treatment adherence. We did not observe a significant difference between adherence in outpatient and sanatorium settings, suggesting the need for further research on this, particularly on the subjective factors concerning relationships with family, friends and the medical team.[18]
Our findings differ from some studies showing adherence increasing with age[52] and higher educational level.[24,43] While these did appear to have an influence in bivariate analysis, the association disappeared with multivariate analysis. Nevertheless, it would be prudent to tailor support to the age and educational levels of persons with HIV.
Some studies have associated non-adherence to change in treatment.[41] In contrast, our study found persons who have changed treatment to be more adherent. This might be related to the limitation of a cross-sectional study, although it is also possible that the change in treatment was because the individuals were in worse health and so felt the severity of the disease more strongly.[53] It could also be that the treatment change was to an easier-to-use regime with fewer tablets. While we did not find an effect of number of tablets in the multivariate analysis, several authors have reported that adherence decreases with an increase in the number of tablets and the number of daily doses.[24,43,54]
Adherence is clearly a challenge for both health professionals and the HIV/AIDS community. Although the number who dropped out of treatment (17 individuals in the sample) seems very low, it means there are dozens of HIV-positive people who could be at risk of becoming ill or dying. Persons who dropped out of treatment or had poor adherence most frequently referred to communications problems with the attending physician and lack of support from family and friends as reasons for their nonadherence. Also mentioned were lack of self-efficacy, disruption of daily activities, forgetfulness, and influence of negative opinions toward antiretroviral therapy,[39,40,53,55,56] all of which therefore should be taken into account in planning personalized interventions, specialized counseling, and training programs for health promoters.
In Cuba, individuals with HIV/AIDS more frequently voice opinions on negative aspects of therapy, such as adverse reactions, lipodystrophy, inconvenience, and number of tablets, than on positive results of therapy, such as increased survival time and well-being, and decrease in opportunistic infections.[2,3,8] This leads to the importance of continuing to publicize positive results of ART within the HIV/AIDS community.
The positive association between high adherence and goof communication with the specialist physician is an important aspect to keep in mind—though we should clarify that at the time of this study, family physicians did not yet play an important role in follow-up of persons on ART. A qualitative study of adherence in Brazil found that health professionals caring for persons with HIV/AIDS are often overworked and have little time to talk with patients about their needs and problems related to therapy and adherence.[53]
MINSAP’s National HIV/AIDS Program has provided training for physicians working with HIV-positive persons,[2] efforts which should continue and be expanded. There still may be untapped potential in improving the doctor-patient relationship in Cuba, such as training health workers in more effective techniques to assist in non-judgmental discussions with patients about adherence and adverse reactions.
The study’s multivariate analysis found no association between adherence and support from family, friends, and classmates/coworkers. This is perhaps surprising, since social networks have been shown to play an important role in general in the lives of people with HIV/AIDS.[21,37] Observations from clinical practice suggest social support can influence memory and self-efficacy, elements which have shown to improve adherence in some settings. Longitudinal research on social networks and adherence in Cuba is needed to clarify the relationship of social networks to adherence.
Our results indicate that more effective mechanisms are also required to help patients remember their medication schedule.[56]
Two highly significant factors in achieving adherence of ≥95% are self-efficacy and commitment to treatment,[57] pointing to importance of programs that aim to increase self-esteem in persons with HIV/AIDS; help them feel capable of following their prescribed ART regimen and integrating it into their daily routine; learn more about ART therapy; and build motivation to remember and take the ARV medications in any setting.
CONCLUSIONS
This study examined the complex, multidimensional nature of adherence to retroviral treatment. While ARV adherence in Cuba is good, achieving perfect adherence remains a challenge. Facilitating a close doctor-patient relationship, motivating persons with HIV/AIDS, increasing their self-efficacy and commitment to treatment, publicizing positive ART outcomes, and assisting them to remember medication schedules are crucial tools for reaching this objective. We need more studies, particularly longitudinal ones, on factors affecting ARV adherence to improve medical care and quality of life of persons with HIV/AIDS in Cuba.
ACKNOWLEDGMENTS
The authors are grateful for the cooperation of study participants, members of GPSIDA, the Comprehensive Care Centers for Persons with HIV/AIDS, and public health authorities from throughout Cuba who dedicated their time and efforts to the interview process. This study is part of a project on HAART adherence, nutrition, and physical exercise in persons with HIV/AIDS, being conducted by researchers from the departments of Biostatistics and Informatics, Medical Care, and Epidemiology of the Pedro Kourí Tropical Medicine Institute, with funding from MINSAP and HIVOS, a Dutch nongovernmental organization.