INTRODUCTION
In 2006, WHO estimated 7.2 million deaths—all preventable—from ischemic heart disease (IHD), with acute myocardial infarction (AMI) the major contributor.[1] Mortality rates and trends vary by country[2–9] and even within countries,[9–11] with differences attributed to both medical determinants (health system characteristics and coverage) and non-medical (risk factor distribution, genetics, environment and socioeconomic factors).[10] Risk of death from AMI increases with age and population aging has contributed to rising numbers of deaths in several countries.[12]
Despite efforts in developed countries, time lag between symptom onset and treatment for AMI continues to be a problem, treatment delay causing further deterioration in myocardial function and more disability and death.[6,8] AMI can be fatal or incapacitate the patient for life, both physically and psychologically. It often occurs in the prime of life and so has serious financial implications, imposing considerable burden not only on individuals and families but also on medical and social services. By 2030, years of potential life lost (YPLL) to cardiovascular diseases (CVD) are expected to increase by 20% over the year 2000 in the United States, 30% in Portugal, 64% in Brazil, 57% in China, and 95% in India.[4]
Data for Latin America are sparse. CVDs overall were the first cause of death in Mexico until 1997, with IHD the most prevalent type.[13,14] In Costa Rica, CVDs have been the leading cause of death since 1970, accounting for 33% of all deaths, 48% of them from AMI,[15] similar to patterns in other countries of the region.[16] AMI causes some 8% of deaths in Chile, primarily striking men aged ≥45 years and women aged ≥60 years.[17] In Brazil, AMI causes one third of deaths from coronary heart disease, the leading cause of death.[18] In Venezuela, AMI mortality rates have been rising since 1959, and today AMI is the second leading cause of death after violence.[19,20]
In Cuba, infectious diseases dominated the mortality picture in the 1960s,[21] but between 1970 and 2008 IHD has been the leading cause of death; with AMI the most common underlying cause of IHD deaths.[22] In 2010, it constituted 42.7% of IHD cases and had the highest case-fatality rate.[22] In that year, 7022 people died of AMI, 81.4% of them aged ≥60 years,[21] representing 7.7% of all deaths in Cuba.[23]
Changes instituted in Cuban health services to address AMI included the 1997 creation of the Integrated Medical Emergency System (SIUM, the Spanish acronym),[24,25] a specialized service at the municipal and provincial level. At the primary care level, SIUM is based in the urgent care polyclinics, a subset of the community-based polyclinics equipped to handle more serious medical emergencies for geographically-defined populations. Each of these has an intensive care unit and an ambulance coordinating center. The provincial subsystem includes a coordinating center for dispatching intensive-care ambulances. A third subsystem operates through hospital emergency services.[24,25]
SIUM has contributed to a progressive decline in mortality from coronary events: prior to the creation of SIUM, 19.6% of heart attack and angina patients spontaneously presenting at a hospital died. However, only 6.8% of patients die who first have been seen in a community health facility and subsequently transferred to hospital by emergency ambulance.[24,25] In one hospital in Havana, AMI case fatality went from 16.1% before SIUM to 13.1% after.[24] The introduction of thrombolytics in all urgent care polyclinics has also contributed to reducing complications and deaths.[25]
Despite such improvements, AMI remains the leading specific underlying cause of death in Cuba.[22] AMI epidemiology is complex, and the lack of a national AMI registry makes research challenging, resulting in lack of population-level studies published in the past decade to shed light on Cuba’s AMI mortality.
Understanding the geographic and demographic distribution of major diseases is important for detecting trends to alert health authorities to situations posing population health risks. Although mortality denotes AMI’s end result, rather than risk of occurrence, it is universally available and so is widely used for geographic comparisons and assessment of temporal trends. Hence this study, whose objective was to describe AMI mortality in Cuba in the decade 1999–2008.
METHODS
A descriptive study was conducted of all deaths in persons aged ≥25 years in Cuba from 1999 through 2008, where underlying cause was diagnosed as AMI. AMI was defined according to the 9th revision of the International Classification of Diseases for 1999–2007 and the 10th revision for 2008; there was no difference in classification of AMI between the two revisions.[26,27] Death certificate was issued by a physician in all cases.
Study variables These included age: as a continuous variable and by group aged 25–34, 35–44, 45–54, 55–64, 65–74, 75–84 and ≥85 years; sex: male or female; place (jurisdiction) of death—all provinces in Cuba (then 14) and the Isle of Youth Special Municipality; site of death—hospital emergency room, hospital (inpatient), out of hospital (another medical facility, home, other and unknown); and time—by year and period (1999–2003 and 2004–2008).
Data source The mortality database of the Ministry of Public Health’s National Statistics Division (DNE–MINSAP, the Spanish acronym) was used.[28]
Data processing and analysis Data were processed with SAS 9.1.3 and EViews 2.0.[29] Absolute frequencies were tabulated, and percentages and rates calculated as summary measurements for qualitative variables. Crude and age- and sex-specific annual mortality rates per 100,000 population were calculated for comparisons, as well as five-year provincial rates. All rates were directly standardized to the 1981 Cuban census population.
Ethical considerations Data were taken from DNE–MINSAP registries and databases without using or divulging identities of the deceased. The study was approved by the Cardiology and Cardiovascular Surgery Institute ethics committee.
RESULTS
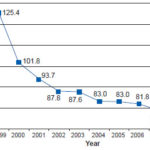
During the period 1999–2008, 145,808 people aged ≥25 years suffered an AMI, 75,572 of whom died, 44,679 men (59.1%) and 30,893 women (40.9%), for a male: female ratio of 1.45. The age-standardized mortality rate was 100.3 per 100,000 population for the decade studied and the case-fatality rate was 51.8%. AMI mortality rates fell over the decade, from a high of 125.4 per 100,000 population in 1999 to 82.8 per 100,000 population in 2008, a net decline of 34% (Figure 1).
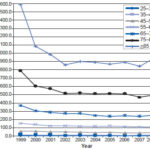
Average age at death was 71.6 years, with a standard deviation of 13.8. AMI mortality rates increased with age. All age groups followed a pattern of highest mortality rate in the initial year of the series and a steep drop in the early years, leading to a plateau or slighter decline. In all age groups except the one aged 25–34 years, there was a slight increase in the mortality rate in the last year of the series (2008), most pronounced in the group aged ≥85 years (Figure 2).
Figure 1: Age-adjusted acute myocardial infarction mortality rates in population aged ≥25 years, Cuba (1999–2008)
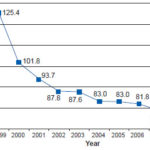
Source: National Statistics Division, Ministry of Public Health, Havana
Figure 2: Acute myocardial infarction mortality rates by age group, Cuba 1999–2008
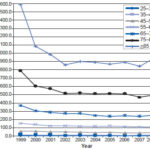
Source: National Statistics Division, Ministry of Public Health, Havana
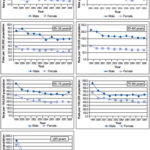
While overall AMI mortality risk increased with age in both sexes, lower rates were always observed in women. However, the gap between male and female mortality rates grew narrower with age, all but disappearing at the upper limit of life span (Figure 3).
Figure 3: Acute myocardial infarction mortality rates by sex and age, Cuba, 1999–2013
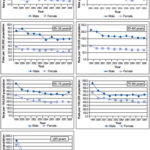
Source: National Statistics Division, Ministry of Public Health, Havana
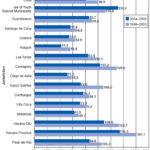
The AMI age-standardized mortality rate per 100,000 population fell by 17.3% between the two five-year periods considered. All jurisdictions had lower rates in the second period, except the Isle of Youth Special Municipality. In 2004–2008, the provinces of Havana, Havana City and Camagüey and Isle of Youth Special Municipality reported the highest mortality rates, while the provinces of Holguín, Ciego de Ávila and Granma had the lowest (Figure 4).
There was a shift in distribution of site of death between the two time periods; the majority in both periods were out of hospital, increasing from 54.9% in 1999–2003 to 58.2% in 2004–2008. There was also an increase in the percentage of in-hospital deaths between the same periods (16.9% in 1999–2003, 25.4% in 2004–2008). There was a decrease in the proportion of emergency room deaths (28.3% in 1999–2003, 15.4% in 2004–2008).
DISCUSSION
AMI has been the leading specific cause of death in Cuba for over 40 years, responsible for 75% of deaths from CVD, which itself causes more than one in every five deaths in Cuba.[22,28] The situation is similar to that of developed and some developing countries.[30,31]
The decline in AMI mortality rates in Cuba during the study period may have been influenced by a series of measures instituted from the primary care level up: use of SIUM advanced mobile life support units with personnel trained to manage AMI (providing clear advantages for patients transported, since the majority reach hospital stabilized and with a positive diagnosis of heart attack, saving time); the equipping of selected community-based polyclinics with advanced emergency services; opening of polyclinic intensive care units for early treatment of patients; and expanded use of systemic coronary thrombolysis in primary care, helping reduce lethal complications.[23]
A 33% reduction in AMI mortality rates was observed in Argentina over 14 years (52 per 100,000 population vs. 35 per 100,000 population in 1990 and 2004, respectively),[32,33] possibly attributable to secondary prevention, along with optimization of resources and deployment of new therapies. However, reduced mortality rates documented by the Argentine Cardiology Society were not accompanied by declines in in-hospital mortality, which remained high and substantially unchanged.[34] Explanations posited for Argentina are also valid for Cuba, where incidence rates have not changed appreciably over the decade we studied, remaining at approximately 1.2 per 100,000 population throughout,[35] strengthening the inference that AMI mortality declines observed are due to improved treatment, with a consequent marked reduction in case fatality rates.[36]
The fact that achievement of universal, free access to highly qualified medical care—key to Cuba’s public health approach to chronic non-communicable diseases—has reduced AMI case- fatality rates without a corresponding reduction in incidence[37] highlights an important area for increased efforts in primary prevention: incidence can only be reduced by reducing cardiovascular risk factors in the population. We must also keep in mind that reduced case fatalities also means increasing numbers of AMI survivors at high risk of suffering a second event.
Figure 4: Acute myocardial infarction mortality rates by province*, Cuba, 1999–2008
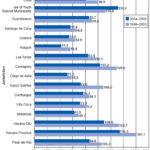
* Including Isle of Youth Special Municipality / Source: National Statistics Division, Ministry of Public Health, Havana
The two principal multicenter collaborative studies, MONICA[38,39] and Atherosclerosis Risk in Communities (ARIC),[40] differ in their conclusions about the importance of changes in treatment and risk factor modification in the observed reduction in AMI mortality rates. MONICA investigators concluded that mortality reductions observed between 1985 and 1994 were fundamentally due to reduced incidence, i.e., better primary prevention,[38,39] while ARIC researchers in the United States attributed these results to improved patient survival due to better treatment.[40] The MONICA project in the United States attributed approximately 25% of reduced heart disease mortality to primary prevention, 29% to secondary prevention and 43% to improved treatment.[41] Clearly, all phases of intervention need to be considered to address the problem of AMI mortality: notwithstanding improvements in AMI treatment and serious efforts at primary prevention, AMI continues to cause millions of deaths worldwide.[3,42,43]
In our study, as in other countries, men had higher AMI mortality rates then women, a pattern similar to that of European countries such as Greece and Finland.[8,44] In some countries—for example, Spain[45] and areas of the Americas and the Caribbean[15,31]—the male:female ratio is smaller, but male rates are still higher.[2,3] In some developed countries, the ratio is about 4:1.[1] In 2005, AMI accounted for 68.3% of all deaths from heart disease in the United States, the percentage 50% higher in men than in women[4]—values that are not substantially different from those obtained in this study.
Despite declining mortality rates, absolute numbers of AMI deaths continue to rise because of population aging, one of the most significant demographic and social consequences of declining fertility and increased life expectancy.[12,22] We found that AMI mortality rates increased with age, independent of sex, which may be explained in part by its association with atherosclerosis and numerous age-related risk factors.[45,46] The steep increase in AMI mortality rates with age has been observed previously in Cuba[22] and Spain.[47] The average age at AMI observed here is similar to that seen elsewhere in the Americas and the Caribbean.[15,31]
In Cuba, heart disease mortality rates in men start to increase steadily from age 35 years,[21] becoming the leading cause of death in men aged ≥45 years (only reaching that status in women two decades later), consistent with international reports.[5,7,15,47] Higher male mortality rates may reflect in part higher incidence because of risk factors that are more common in men, such as tobacco and alcohol use.[46,48]
Out-of-hospital deaths remain a significant problem. It was observed that in both periods more than half the AMI fatalities occurred before reaching hospital, patients succumbing in places where they could not receive the care needed to survive. There was an increase in the proportion of out-of-hospital mortality in the second five-year period analyzed, exceeding reports from elsewhere in the Americas; in the United States an estimated 47% of AMI deaths occur before the patient reaches emergency services[5] and in Chile, up to 30% of patients with AMI die before receiving medical attention.[17] This could be due to insufficient awareness of AMI symptoms, leading to postponed seeking of medical attention. Research at the primary care level would help focus efforts to educate the public on AMI symptoms and what to do when they occur. Heightened public awareness could help reduce deaths that happen before seeking medical attention, but it is also necessary to understand whether there are access issues that influence this delay.
Figure 5: Proportion of acute myocardial infarction deaths by site and fi ve-year period, Cuba, 1999–2008

Source: National Statistics Division, Ministry of Public Health, Havana
Although overall AMI mortality decreased, the proportion of deaths occurring in-hospital increased; this was primarily due to a halving of the emergency room case fatality rate (21.9% in 1999–2003 to 10.6% in 2004–2008), only partially offset by a slight increase in the in-hospital case fatality rate (from 16.8% in 1999–2003 to 19.7% in 2004–2008).[36] The latter increase is only to be expected with a decrease in emergency room mortality, since whether or not a patient survives depends inter alia on complications arising within the first few hours of the event, extent of infarction, and degree of myocardial dysfunction. The earlier the patient receives medical attention, the more likely such complications will appear after the patient has already been hospitalized.
In addition, an AMI mortality increase is seen in persons aged >65 years, who have accumulated more life-threatening risk factors. Despite improvements in medical care (early reperfusion, percutaneous thrombolysis and interventions such as coronary angioplasty), treatment delays still occur throughout the country, exacerbating deterioration in myocardial function and hence, disability and death.[49,50]
In recent years, the Cuban emergency care system has taken steps—both in hospital settings and in the rest of the system—to reduce AMI case-fatality rates and mortality. SIUM mobile acute coronary care units mentioned above have helped speed patients to health centers where they can receive immediate thrombolytic treatment, thereby reducing mortality.[24] Thrombolytic treatment for AMI improves quality of life after an acute episode.[51] Thus, use of domestically-manufactured recombinant streptokinase for AMI has led to a radical change in patient outcomes and opens up new prospects for treatment of other cardiovascular disorders. It is most effective within the first 114 minutes of the ischemic event,[24,51,52] but studies of intravenous thrombolysis in Havana City have found that fewer than 50% of AMI patients receive thrombolytic treatment,[53] revealing scope for more attention to this therapy for improving survival.
We have encountered two constraints related to information in our study. The first is that, due to the lack of an AMI registry in Cuba, it was impossible to examine sociodemographic and clinical variables in depth. The second is that summary data on death site available from our sources did not permit disaggregation to explore all variables of interest, which would have contributed to a better understanding of this aspect. Nevertheless, the study yielded important data on the extent of AMI mortality in Cuba and the need for continued efforts to reduce its impact. We recommend that further studies be conducted to monitor trends and assess the potential role of primary health care in reducing AMI mortality, as well comparative evaluations of in-hospital protocols and their application.
CONCLUSIONS
Acute myocardial infarction remains a critical health problem in Cuba, although mortality rates decreased until the end of the decade analyzed, increasing slightly in 2008. Registration of all AMI cases is needed, as well as cardiovascular risk assessments to identify at-risk individuals and studies of out-of-hospital mortality and quality of medical care for AMI, to help elucidate possible causes of Cuba’s high AMI mortality. Campaigns to raise public awareness of AMI symptoms could also help further reduce AMI mortality.