ABSTRACT
Introduction Cardiovascular morbidity and mortality increase in women after menopause. Various scoring models assess qualitative risk of cardiovascular disease. The Framingham Heart Study global risk score is among the most widely used.
Objective Determine level of coronary heart disease risk among women aged ≥60 years in a Havana health catchment area (geographic area whose residents are served by the Mártires del Corynthia Polyclinic, in the Plaza de la Revolución municipality of Havana).
Methods A descriptive, cross-sectional study was conducted in 2006. Universe: all women (3,396) aged ≥60 years in the catchment area, attended at the primary care level by the Polyclinic and 42 neighborhood family doctor-and-nurse offices. Equal probability sample: 1,082 women meeting the inclusion criteria, chosen through single-stage cluster sampling considering a <10% error margin for estimates for this parameter, a 95% confidence interval (CI) and a design effect of 1.5. Absolute frequencies and percentages were calculated to summarize the qualitative data obtained. Results were presented as tables.
Results The most common cardiovascular risk factors found in this study were: physical inactivity, 74.9%; hypertension (HTN), 70.6%; abdominal obesity, 53%; reported family history of coronary heart disease (CHD), 41.8%; diabetes mellitus (DM), 21.8%; and cigarette smoking, 17.2%. Scoring according to number of risk factors present in each individual, 79.3% of these women fell into the high- or moderate-risk categories.
Conclusion The large number of women categorized as high- or moderate-risk for coronary heart disease in this population emphasizes the need for preventive actions aimed at reducing these figures.
Keywords Cardiovascular diseases, vascular diseases, ischemic heart disease, coronary heart disease, postmenopause, woman, aged, risk factors, risk assessment, hypertension, high blood pressure, lifestyle, diabetes mellitus, obesity, abdominal adipose tissue, body mass index, physical inactivity, tobacco use
INTRODUCTION
In Cuba, heart disease has been the number one cause of death for over 40 years. In 2005, mortality from heart disease was 188.9 per 100,000 population; and 1,121.9 per 100,000 population for persons aged ≥60 years. Among women aged ≥60 years, mortality was 1,124.9 per 100,000 population.[1]
The same year, Havana registered the highest rate of heart disease mortality among Cuban provinces; and of these deaths, 72% were the result of coronary heart disease (CHD).[1] International studies indicate that this figure could be reduced through effective preventive measures aimed at promoting healthy lifestyles and reducing risk factors for cardiovascular disease (CVD).[2,3]
In 2001, among Havana residents aged ≥60 years, the most prevalent noncommunicable chronic diseases diagnosed at the primary care level were: hypertension (HTN) at 509.6 per 1,000 population, diabetes mellitus (DM) at 103.7, and coronary heart disease(CHD) at 86.4. The rates were higher among women. [4] In 2005, DM prevalence among Havana women aged 60-64 years was 178.0 per 1,000 population, and for those aged ≥65 years, 132.4; HTN prevalence was 612.7 and 465.8, respectively for the same age groups.[1]
Several epidemiological studies over the last 20 years have revealed a correlation between atherosclerosis and factors such as physical inactivity, stress, HTN, DM, obesity, hypercholesterolemia and tobacco use, among others, of which these have been defined as coronary heart disease risk factors. Simultaneous presence of various risk factors have a multiplying effect; therefore, an individual with several moderate-risk factors may be at a higher risk of developing CHD than a person with a single high-risk factor.[5,6-10]
A multiple-cause descriptive model is useful for health authorities to identify high- and moderate-risk populations and, thus, to devise more effective intervention strategies. The Framingham Heart Study model is among the most widely used to calculate cardiovascular risk. The terms ‘coronary heart disease risk’ and ‘cardiovascular risk’ generally are used interchangeably given the high correlation between the two. Global cardiovascular risk (GCR) is defined as the probability of suffering a cardiovascular event within the next 10 years. Two methods are used to calculate GCR: qualitative and quantitative.[6-11]
Determining GCR is crucial to focus CVD prevention efforts on the highest risk groups.[3,8] The World Health Organization (WHO) has urged new epidemiological research on the influence of coronary risk factors on patterns of cardiovascular morbidity and mortality, as the basis for modification of these patterns.[2]
According to the Framingham data, most coronary events occur after 65 years of age, particularly among women. The risk of dying from cardiovascular disease (CVD) at the age of 60 is almost the same for women and for men; however, at older ages the risk is higher among women than men.[12]
Of all Havana municipalities, Plaza de la Revolución has one of the highest CVD mortality rates. According to the 2005 Health Situation Assessment of Plaza de la Revolución Municipality (unpublished report, Plaza de la Revolución Municipal Health Department), the male/female CVD mortality ratio shows proportionately more women aged ≥60 years dying from this cause. In the health area served by the Mártires del Corynthia Polyclinic, cardiovascular disease has become a major health problem. Universal primary care facilities in this health area serve a total population of 24,280 (including children, adults and the elderly). Of these 11,327 (46.7%) are male and 12,933 (53.3%) female. A total of 5,981 people are aged ≥60 years, constituting 24.3% of the area’s population; of the elderly, 2,480 are men and 3,396 women.
No previous study has been conducted to determine cardiovascular risk among the population of this municipality, nor is there a commonly used risk scoring for Cuban women of geriatric age.
The objective of this 2006 study was to ascertain total cardiovascular risk among women aged ≥60 years in the health catchment area served by the Mártires del Corynthia Polyclinic; and this study is the first to assess the magnitude of coronary risk factors in older Cuban women.
MATERIALS AND METHODS
A descriptive, cross-sectional study was conducted in 2006 among the female population aged ≥60 years living in the health catchment area served by the Mártires del Corynthia Polyclinic in Havana’s Plaza de la Revolución municipality.
Universe All women (3,396) aged ≥60 years in the health catchment area attended at the primary care level by the Polyclinic and 42 neighborhood family doctor-and-nurse offices. (In Cuba’s primary care system, a community-based polyclinic directs the work of several dozen family doctor-and-nurse offices charged with health promotion, and with disease prevention, diagnosis, and follow-up within a specific geographically defined population.)[ 13]
Sample The required sample size was 1,191 women aged ≥60 years. A total of 1,082 women (90.8% of the required sample) were interviewed, prior written informed consent. Those with coronary heart disease (CHD) diagnosis were excluded. The sample was calculated based on the least prevalent risk factor – that is, DM (18% of the female population aged ≥60 years) – in the health area. Calculating an error margin of <10% in estimates for this parameter, with a 95% confidence interval (CI), n=794 was multiplied by a design effect of 1.5. The sample was chosen through single-stage cluster sampling. Family doctor-and-nurse offices were selected by simple random sampling.
Inclusion criteria Women aged ≥60 years residing in the selected health area.
Exclusion criteria Women with mental or physical disabilities or limiting chronic diseases that prevented them from communicating with researchers or traveling to places where the study’s anthropometric measurements were taken; women previously diagnosed and under treatment for coronary heart disease (CHD); women who described CHD symptoms during the interview and were referred to the health area’s cardiologist to confirm diagnosis; or those who did not consent to participate.
Variables Used Socio-demographic variables: age, including both calendar age and age group (60-69, 70-79, ≥ 80); skin color as assessed by interviewer (white, black or mixed), employment status (employed, retired, housewife), marital status (single, married, widowed, divorced) and educational level completed (primary school, secondary school, high school, technical school or university).
Coronary risk factors: Cigarette smoking (tobacco use up to one-year prior to the interview); physical inactivity, defined by the individual’s level of physical activity; hypertension (HTN)(women who referred hypertension and were on antihypertensive medications, or whose blood pressure measured ≥140/90 mmHg, determined with Korotkoff auscultation method)[12,13]; family history of coronary heart disease in father or mother, with early onset of CHD (before 65 years in the mother and before 55 in the father); diabetes mellitus (DM) as referred by participants, treated with insulin or oral hypoglycemic medication; and abdominal obesity (waist circumference of >88 cm).
Global cardiovascular risk (GCR): Based qualitative assessment using a modified Framingham score. While the Framingham uses only low- and high-risk categories, for the purpose of our study, individuals were classified as low (0-1 risk factors), moderate (2-3 risk factors) or high (4-6 risk factors) cardiovascular risk. We also considered abdominal obesity, physical inactivity and cardiovascular family history as risk factors. The presence of DM alone in an individual rated her as high risk, since DM is a powerful cardiovascular risk predictor in women, increasing by 3 to 7 times the chances of developing coronary heart disease.
Techniques and Procedures Information was obtained from primary and secondary sources. A structured survey questionnaire was applied by a physician previously trained for this purpose, once written informed consent was obtained from each participant.
Each subject’s blood pressure was measured twice, at a 20-minute interval, with a calibrated aneroid sphygmomanometer. Average blood pressure was calculated and hypertension considered at ≥140/90 mmHg.[14-16]
Data Processing The information obtained from the survey was introduced into a database developed for the study, using Microsoft Excel 2000. Absolute frequencies and percentages were determined to summarize qualitative data, using the SPSS 13.0 program. Results were presented in tables.
RESULTS
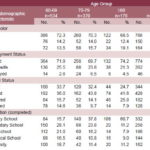
As shown in Table 1, nearly half the women in the study sample were aged 60-69 years, constituting the largest age group, followed by those 70-79 years. Given that older age groups present higher mortality, it was expected that women aged 60-69 would be the most represented in the sample. The majority of women in the sample (71.0%) were white.
Most of the women were retired, in each age group and in the sample as a whole, with 4.3% of the total still working. Taking into account the high employment rates among Cuban women, and that their legal retirement age is 55, it was not surprising to find that over two-thirds of the women in the sample were retired.
Table 1: Distribution of Sample by Socio-demographic Characteristics and Age Group
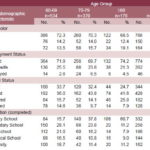
Source: Study survey, Mártires del Corynthia Polyclinic, Plaza de la Revolución municipality, Havana, 2006.
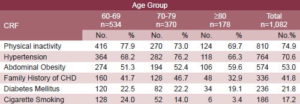
Table 2: Distribution of Sample by Coronary Risk Factor (CRF) and Age Group
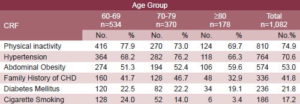
Source: Study survey, Mártires del Corynthia Polyclinic, Plaza de la Revolución municipality, Havana, 2006.
Over one-third of participants were married. As to education, the highest levels were found in the 60-69 age group, where more than half were technical, mid-level and higher education graduates. These women’s childhood and adolescent years coincided with the social changes that occurred in Cuba after 1959, facilitating greater access to study at all levels.
Table 2 shows risk factors most frequently found in this female population, both in general and by age group. These were, in order of importance: physical inactivity, hypertension, abdominal obesity and a family history of CHD.
Physical inactivity is common among older age groups, although as age advances, slightly more women exercised. Hypertension rates were high, recorded in four of five women in the 70-79 age group. Smoking decreased with age. DM was much more frequent in these older age groups, much more so than in younger women,[1] an influential factor in higher CHD risk in the elderly.
Central obesity was present in over 50% of the study sample, ascending with age, values reaching almost 60% among women aged >80 years. High frequency of CHD history among first-degree relatives contributed significantly to risk in the study sample.
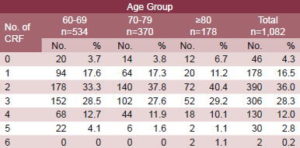
Table 3 indicates presence of multiple cardiovascular risk factors among these older women: two or more were present in nearly 80% of the sample.
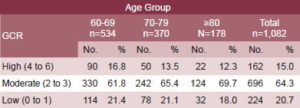
Table 4 reveals that some 80% of these older women studied, as a whole and in the various age groups, were classified in the high and moderate cardiovascular risk categories.
DISCUSSION
Some of the socio-demographic features of the study population coincided with what we expected to find, such as the proportion of retired women, given that they may retire at 55 in Cuba.
Prevalence of hypertension: Our study corroborates results from authors such as Valdés Pacheco and Mosca in Cuba and elsewhere, who have reported high prevalence (over 60%) of HTN among women aged ≥60 years.[17- 20] Our findings also coincide with the Second National Survey on Risk Factors and Chronic Diseases in the Cuban population, which reported HTN prevalence above 60% among persons aged ≥60 years.[21] Hypertension is the most important risk factor among the elderly for strokes and cardiovascular events and is considered a worldwide problem. When HTN is managed properly, the risk of a cardiovascular event decreases considerably.[17-20] A meta-analysis[19] (nine prospective studies of 420,000 individuals with no history of cardiac infarction or stroke who were followed up for 10 years) showed that the relative risk of developing CHD was 5 to 6 times higher among individuals with a DBP mean value of 105 mmHg than among those with a DBP mean value of 76 mmHg. Many studies have demonstrated that HTN behaves as a risk factor, independent of vascular disease, and is most prevalent in Western societies.[23-30] Overall, HTN can be considered a major risk factor for cardiovascular morbidity and mortality.[27]
HTN prevalence increases with age.[25-28] During adult years, it is more frequent among men, but several studies have shown that, in persons aged >60, the pattern is reversed, and in those aged >70, HTN is more common among women. In one study in Argentina, HTN prevalence was over 65% in population aged >60 years, and was particularly frequent in the 65-74 age group.[29] Data presented by Baena, Contin and Banegas confirm this high prevalence in other countries,[23,30,31] prompting us to consider control of hypertension at the primary care level essential to diminish rising cardiovascular risk with age.
Table 3: Distribution of Sample by Number of Coronary Risk Factors (CRF) and Age Group
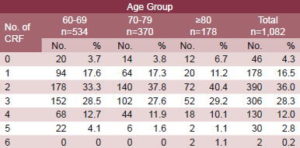
Source: Study survey, Mártires del Corynthia Polyclinic, Plaza de la Revolución municipality, Havana, 2006.
Table 4: Distribution of Sample by Global Cardiovascular Risk (GCR) and Age Group
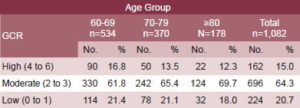
Source: Study survey, Mártires del Corynthia Polyclinic, Plaza de la Revolución municipality, Havana, 2006.
Prevalence of smoking: Our findings are similar to those reported in the international medical literature, which also suggests lower prevalence among older women. This lower prevalence is attributed to several factors, including the fact many never started smoking, influenced by the social norms of their earlier years.[32] In our study, women aged >80, who were adolescents in the 1930s, apparently did not acquire the habit, which became more socially acceptable among women after World War II. Prevalence among women who were adolescents in the 1940s was somewhat higher, and that among the younger group, who were adolescents in the 1950s, higher still with 24% of women reported as smokers.[33,34]
Conclusive evidence points to the benefits of quitting smoking. This risk factor is the chief preventable cause of cardiovascular disease morbidity and mortality. It accounts for 50% of all preventable deaths and for 29% of those caused by coronary heart disease.[34,35] According to Hennekens et al., quitting smoking reduces coronary event incidence by up to 50% among low-risk populations.[34]
Results from Serrano et al.[35] corroborate the importance for coronary patients of quitting tobacco use and the need for intervention programs to help those patients with greater nicotine dependence to quit and maintain abstinence, considering the great morbidity and mortality implications for patients who continue to smoke. In recent years, treatment for smoking cessation has relied more on pharmacological aspects and on multi-faceted programs in which the role of health professionals is crucial.
Prevalence of diabetes mellitus: DM rates in our study were higher than those described by other Cuban authors such Valdés
Pacheco et al.[17] in their study on CHD prevalence and risk factors (reporting 14% DM in geriatric women). As already stated, DM is a strong predictor of cardiovascular risk in women, multiplying by three to seven times the likelihood of developing CHD; and compared to a multiplier of two to three times for men.[36] Diabetic patients are at high risk for developing CVD, and their mortality risk is similar to that of those with a diagnosed cardiovascular condition. This is due to the greater prevalence of other risk factors in this population and the effect of diabetes itself on macro- and microcirculation.[37,38] Furthermore, diabetic patients are more likely to develop an acute coronary syndrome or even “silent” sudden death.
Abdominal obesity: Its distribution among the sample could be linked to disorders in fat metabolism and changes in postmenopausal fat distribution, which leads to abdominal adipose tissue accumulation in women. The concept of abdominal obesity is important due to its link with increased cardiovascular risk. It is defined by waist circumference >102 cm in men or >88 cm in women.[39] According to authors such as Lakka, Kanaya and Larson,[39-41] abdominal obesity is a more precise and easily measurable predictor for CHD.
Physical inactivity: Among older women served by the Mártires del Corynthia Polyclinic, inactivity was less frequently a problem as age advance. This might be explained by the fact that generally, as women assimilate their age, they take on activities customary to older age, including seniors’ clubs and neighborhood grocery shopping. In this way, they make walking part of their daily physical activity. Studies by Alexander et al. and Dubach in the USA[42,43] confirm the overall benefits of physical activity to reduce CHD risk, even when 60% of US adults do not exercise regularly. Estimates suggest that physically inactive people are approximately twice as likely to develop CHD or to die from it than active ones.[44]
In the case of CHD, moderate physical activity seems to produce great health benefits. Authors such as Manson et al.[45] have shown that walking is associated with better blood pressure control in persons over 60. Thus, at least for this subgroup of individuals among whom most CHD cases are found, data supports walking as good for the heart. In the United States, population attributable risk is estimated at approximately 35% for physical activity and CHD risk, meaning that if inactive persons achieved a moderate level of physical activity, CHD events in total population would theoretically be reduced by 35%.[46] Cardiovascular and general health benefits of exercise should be emphasized in public messages, and health professionals should recommend physical activity to patients in our clinical practice.
The results of this study, where 2-3 risk factors were found in more than half of the older women studied, are similar to those obtained by Nigro et al.[47] in their study on cardiovascular risk factors among elderly women in Córdoba, Argentina. They found high frequency of risk factors among older women, in half of whom at least two were present.
The distribution of global cardiovascular risk (GCR) suggests why cardiovascular disease morbidity and mortality continue to be high in Cuba, particularly among older women.
Scientists today believe that the synergistic activity of several risk factors in the same individual contributes more to CHD than the effect of any single risk factor. This activity then determines the real risk for participants in our study over the next 10 years. [6-10,48]
Stratifying risk is essential to determine follow-up frequency as well as treatment regimen and intensity. Risk should be stratified in categories that permit adoption of adequate therapeutic strategies adapted to the needs and level of risk of each patient.[2,47,49]
The absence of adequate cardiovascular risk assessment may result in unnecessary and inappropriate medication and clinical controls that diminish patients’ quality of life and imply a costly burden for the public health system. The numerical quantification of risk and its clinical consequences constitutes information that should be provided to patients to improve effectiveness of preventive actions.
CONCLUSIONS
High prevalence in this sample of women aged ≥60 years with moderate or high risk of developing a cardiovascular disease within the next 10 years makes this population group an important target for preventive actions to reduce risk, particularly at the primary care level.
The quantitative total cardiovascular risk for this population group should be determined, and follow-up provided according to risk categories. Preventive actions, especially for high and moderate cardiovascular risk groups, should be implemented, as well as pharmacological and other treatment as clinically necessary. Lifestyle changes should be encouraged, particularly physical activity.
Cardiovascular risk for this population should be further studied according to socio-demographic variables such as skin color, employment status, marital status, and educational level.
References

- Ministerio de Salud Pública (MINSAP), Dirección Nacional de Estadísticas. Anuario Estadístico de Salud 2005. La Habana: MINSAP;2006.
- World Health Organization (WHO). Prevention of cardiovascular disease. Guidelines for assessment and management of cardiovascular risk. Geneva: WHO;2007.
- Fox CS, Evans JC, Larson MG, Kannel WB, Levy D. Temporal trends in coronary heart disease mortality and sudden cardiac death from 1950 to 1999: The Framingham Heart Study. Circulation. 2004;110:522-527.
- Ministerio de Salud Pública (MINSAP), Dirección Nacional de Estadísticas. Temas Estadísticas de Salud. La Habana: MINSAP (CU); 2002.
- Stamler J. The Marked Decline in Coronary Heart Disease Mortality. Rates in the United States, 1968-1981. Summary of Findings and Possible Explanations. Cardiology. 1985;72:11-22.
- Ferguson JL, Beckett GJ, Stoddart M, Wacqer SW, Fox KA. Myocardial information redefined: The new ACC/ESC definition, based on cardiac troponin, increases the apparent incidence of information. Heart. 2002 Oct;88(4):343-347.
- Wilson P, D’Agostino R, Jevy D. Prediction of coronary heart disease using risk factors categories. Circulation. 1999;97:1837-47.
- Dawler TR. The Framingham Study: Risk factors and coronary disease. Cambridge: Harvard University Press; 2000.
- Anderson KM, Wilson PW, Kannel WB, Odell PM. An updated coronary risk profile. A statement for health professionals. Circulation. 2001;83:356- 62.
- Wood D. Prevention of coronary heart disease in clinical practice. Recommendation of the Second Joint Task Force of European and other Societies on coronary prevention. Eur Heart J. 2002;19:1434-46.
- Marrugat J, Solanas P, D’Agostino R. Estimación del riesgo coronario en España mediante la ecuación de Framingham calibrada. Rev Esp Cardiol. 2003;56(03):253-61.
- National Cholesterol Education Program (NCEP). Adult Treatment Panel III. JAMA. 2001;285:2486- 97.
- Ministerio de Salud Pública (MINSAP), Dirección Nacional de Atención Ambulatoria. Programa de Atención Médica Integral a la Familia. La Habana: MINSAP;1987:3-4.
- Kannel WB. Cardiovascular Risk Factors in the Elderly: The Framingham Study. Brit Med J. 2000;8:565-75.
- Ministerio de Salud Pública (MINSAP). Comisión Técnico Asesora de Hipertensión Arterial. Programa para la Prevención, Detección, Diagnóstico y Tratamiento de la Hipertensión Arterial. La Habana: MINSAP (CU); 2004.
- Joint National Committee. The sixth report of the Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure. Arch Intern Med. 1997;157:2413-16.
- Valdés Pacheco E, Morrees Abella A, Alonso Díaz NL. Prevalencia y factores de riesgo de cardiopatía isquémica. Rev Cubana Med Gen Integr. 1998;14(6):590-94.
- Mosca L, Grundy SM, Judelson D, King K, Limacher M, Oparil S, et al. Guide to preventive cardiology in women. Circulation. 1999;99:2480-4.
- Mosca L, Appel LJ, Benjamin EJ, Berra K, Chandra- Strobos N, Fabunmi RP, et al. Evidencebased guidelines for cardiovascular disease prevention in women. Circulation. 2004;109:672-93.
- Mosca L, Ferris A, Fabunmi R, Robertson RM. Tracking women’s awareness of heart disease. An American Heart Association National Study. Circulation. 2004;109:573-9.
- Instituto Nacional de Higiene, Epidemiología y Microbiología (INHEM). II Encuesta Nacional de Factores de Riesgo de Enfermedades Crónicas no Transmisibles en Cuba. Informe de Trabajo. La Habana: INHEM (CU); 2002.
- MacMahon S, Peto R, Cutler J, et al. Blood pressure, stroke, and coronary heart disease. Prolonged differences in blood pressure: Prospective observational studies corrected for the regression dilution bias. Lancet. 1995;335:765- 70.
- Baena Díez JM, Del Val García JL, Tomás Peregrina J, Martínez Martínez JL, Martín Peñacoba R, González Tejón I, et al. Epidemiología de las enfermedades cardiovasculares y FR en atención primaria. Rev Esp Cardiol. 2005;58:367-73.
- Prospective Studies Collaboration. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903-13.
- Pineda Cuenca M, Custardoy Olavarrieta J, Andreu Ortiz MT, Ortiz Arroniz JM, Cano Montoso JG, Medina Ferrer E, et al. Estudio de prevalencia de factores de riesgo cardiovascular en un área de salud. Aten Primaria. 2002;30:207-13.
- Segura Fragoso A, Rius Mey G. Factores de riesgo cardiovascular en una población rural de Castilla-La Mancha. Rev Esp Cardiol. 1999;52:577-8.
- Franklin SS, Larson MG, Khan SA, Wong ND, Leip EP, Kannel WB, et al. Does the relation of blood pressure to coronary heart disease risk change with aging? The Framingham Heart Study. Circulation. 2001;103:1245-9.
- Puras A, Sanchos C, Artigao LM, Divison JA. Prevalence, awareness, treatment, and control of hypertension in a Spanish population. Eur J Epidemiol. 1998;14:31-6.
- Nigro D, Vergonttini JC, Kuschnir E, et al. Epidemiología de la hipertensión arterial en la ciudad de Córdoba, Argentina. Rev Fed Arg Cardiol. 1999;28: 69-75.
- Contin M, Burges G, Soris J, Batista. HTA: Incremento esperanza de vida. Hipótesis. Rev Cubana Med. 2001;40(2):103-8.
- Banegas R, Rodríguez-Artalejo F, Ruilope LM, Graciani A, Luque M, De la Cruz-Troca JJ, et al. Hypertension magnitude and management in the elderly population of Spain. J Hypertens. 2002;20:2157-64.
- Nerín I. El tabaquismo en la mujer: una atracción fatal. Arch Bronconeumol. 2005;41:360-2.
- Jane M, Saltó E, Pardell H, Tresserras R, Guayta R, Taberner JL, et al. Prevalencia del tabaquismo en Cataluña, 1982-1998: una perspectiva de género. Med Clin (Barc). 2002;118:81-5.
- Hennekens CH. Increasing burden of cardiovascular disease: current knowledge and future directions for research on risk factors. Circulation. 1998;97:1095-102.
- Serrano M, Madoz E, Ezpeleta I, San Julián B, Amézqueta C, Pérez-Marco JA, et al. Abandono del tabaco y riesgo de nuevo infarto en pacientes coronarios: estudio de casos y controles anidados. Rev Esp Cardiol. 2003;56:445-51.
- Sánchez-Recalde A, Kaski JC. Diabetes mellitus, inflamación y aterosclerosis coronaria: perspectiva actual y futura. Rev Esp Cardiol. 2001;54:751-63.
- Nathan D, Meigs J, Singer D. The Epidemiology of Cardiovascular Disease in Type 2 Diabetes Mellitus: How Sweet It Is or Is It? Lancet. 1997;350 (Suppl):1-32.
- Smith SC Jr, Clark LT, Cooper RS, Daniels SR, Kumanyika SK, Ofili E, et al. American Heart Association; Obesity, Metabolic Syndrome, and Hypertension Writing Group. Discovering the Full Spectrum of Cardiovascular Disease. Minority Health Summit 2003. Report of the Obesity, Metabolic Syndrome, and Hypertension Writing Group. Circulation. 2005;111:134-9.
- Lakka HM, Lakka TA, Tuomilehto J, Salonen JT. Abdominal obesity is associated with increased risk of acute coronary events in men. Eur Heart J. 2002;23:706-13.
- Kanaya AM, Vittinghoff E, Shlipak MG, Resnick H.E, Visser M, Barrett-Connor DE. Association of total and central obesity with mortality in postmenopausal women with coronary heart disease. Am J Epidemiol. 2003;158:1161-70.
- Larson B, Svardsudd K, Wilhelmsen L, Bjorntorp P. Abdominal adipose tissue distribution, obesity, and risk of cardiovascular disease and death. BMJ 1984;288:1401-04.
- Alexander NB, Galecki AT, Grenier ML. Task specific resistance training to improve the ability of activities of daily living-impaired older adults to rise from a bed and from a chair. J Am Geriatr Soc. 2002;49:1418-27.
- Dubach P. Exercise training in chronic heart failure: why, when and how. Swiss Med Wkly 2001;131(35-36):510-4.
- Bijnen FC, Caspersen DJ, Mosterd WL. Physical Inactivity as a Risk Factor for Coronary Heart Disease: A WHO and International Society and Federation of Cardiology Position Statement. Bull World Health Org. 1994;72:1-4.
- Manson JE, Hu FB, Rich-Edwards JW, Colditz GA, Stampfer MJ, Willett WC, et al. A prospective study of walking as compared with vigorous exercise in the prevention of coronary heart disease in women. N Engl J Med. 1999;341:650-8.
- Macera CA, Hootman, JM, Sniezek, JE. Major public health benefits of physical activity. Arthritis Rheum. 2003;49(1):122-128.
- Nigro MB, Herrera HL, García G, Raviolo L, Ledesma RE. Evaluación de factores de riesgo cardiovascular en mujeres de la tercera edad. Rev Fed Arg Cardiol. 2005;34: 358-365.
- Grundy S, Bazarre T, Cleeman J, D’Agostino R, Hill M, Houston-Miller N, et al. Prevention Conference V: Beyond secondary prevention: identifying the patient for primary intervention: medical office assessment. Writing Group. Circulation. 2000;101:E3-E11.
- Alvarez Cosmea A. Las tablas de riesgo cardiovascular. Una revisión crítica. Medifam. 2001;11(3).
THE AUTHORS
Nurys B. Armas Rojas (Corresponding Author: nurysarmas@infomed.sld.cu), specialist in hygiene and epidemiology, adjunct researcher, Preventive Cardiology Department. Institute of Cardiology and Cardiovascular Surgery (ICCCV), Havana, Cuba.
Yesenia de la Caridad Hernández Álvarez, specialist in hygiene and epidemiology, National Institute of Hygiene, Epidemiology and Microbiology (INHEM), Havana, Cuba.
Alfredo F. Dueñas Herrera, specialist in cardiology, associate researcher, ICCCV, Havana, Cuba.
Reynaldo de la Noval García, specialist in cardiology, adjunct researcher, ICCCV, Havana, Cuba.
Antonio Castillo Guzmán, specialist in health administration, ICCCV, Havana, Cuba.
Submitted: October 24, 2007 Approved: February 12, 2008