The National Immunization Program (NIP) begun in 1962 has considerably reduced the infectious disease burden in Cuba over the years, especially among children. The Ministry of Public Health estimates that some 560,000 children would have contracted these diseases, some with fatal outcomes, had it not been for the aggressive vaccination strategy begun 45 years ago and developed since then.[1]
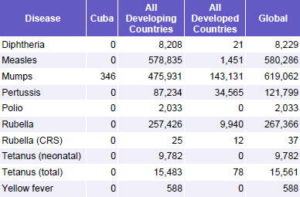
Fast-forwarding to 2006, Cuba is among the countries with the best indicators for vaccine-preventable diseases (Table 1).
Table 1: Reported Cases of Vaccine-Preventable Diseases
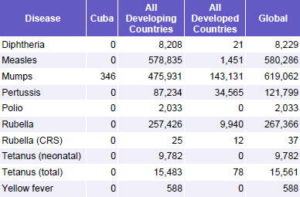
Source: WHO Vaccine-Preventable Diseases: Monitoring System, 2006 Global Summary
Noteworthy among the diseases eliminated or considerably reduced in Cuba:
Elimination of diseases: poliomyelitis (1962); diphtheria (1979); measles (1993); pertussis (1994); and rubella (1995).
Elimination of severe clinical forms: neonatal tetanus (1972); tuberculous meningitis in children aged <1 year (1997).
Elimination of serious complications: congenital rubella syndrome (1989); post-mumps meningoencephalitis (1989).
Diseases that no longer constitute a health problem (rates <0.1 per 100,000 pop.): tetanus (since 1987); Haemophilus influenzae type b (since 2003); typhoid fever (since 2005); mumps.
Reduction of morbidity and mortality by >95%: meningococcal disease (since 2002); hepatitis B (since 2003); parotiditis (since 2004).[1]
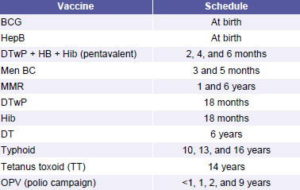
The current vaccine schedule targets all Cuban children for immunization against 13 diseases with 11 vaccines, eight of which are produced by the country’s Scientific Pole (See Feature: Cuba’s Biotechnology Revolution). The most recent change in the schedule occurred in 2006, with the introduction of the Cuban-manufactured pentavalent vaccine (including DTwP, HepB, and Hib). Since 2003-2004, when Cuba was faced with shortages of imported DTwP vaccines (due to shipments of lots that did not meet Cuban quality control standards), all but MMR (measles, mumps, and rubella), OPV (oral polio vaccine), and BCG (Bacille Calmette-Guérin for TB) have been made in Cuba.
It is worth noting that all children in Cuba are vaccinated against hepatitis B and meningococcal meningitis (BC), with vaccines developed in Cuba; the latter is the only internationally marketed vaccine available for serogroup B meningococcus (See Original Article: Cuban Meningococcal BC Vaccine: Experiences & Contributions from 20 Years of Application).
Table 2: Vaccination Schedule: Cuba, 2007
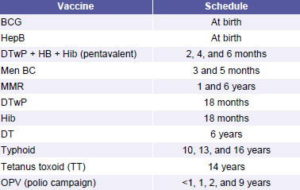
Source: Galindo MA. Programa Nacional de Inmunización, Cuba. PowerPoint presentation at FINSA, November 2006, Havana
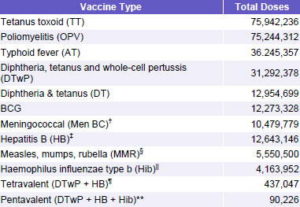
The Public Health Ministry reports that some 277 million doses of vaccines have been administered (1962 to 2006). See Table 3.
Vaccination Strategies
The National Immunization Program is guided by four tenets, aimed at total coverage of children and at-risk populations, which coincide with guidelines and recommendations of the World Health Organization (WHO) and the Pan American Health Organization (PAHO).[2]
- Vaccination efforts encompass total population (equity)
- Vaccination is integrated into primary health care services
- The program relies on active community participation
- Vaccination is free of charge
Table 3: Total Doses Administered by Vaccine Type in Cuba 1962 to 2006*
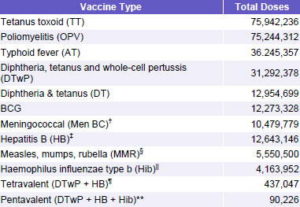
* Provisional
† Vaccination began in 1988; ‡ Vaccination began in 1992; § Vaccination began in 1986; || Vaccination began in 1999; ¶ Vaccination began in 2005, substituted with pentavalent in late 2006; ** Vaccination began in 2006
Source: Statistical Yearbook, 2006. Ministry of Public Health, Cuba
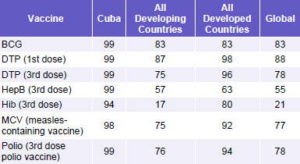
Table 4: Percentage of Target Population Vaccinated*, WHO-UNICEF Coverage Estimates
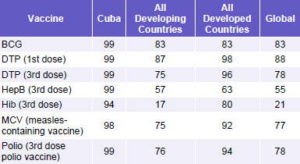
*Target population in Cuba’s case is all children ≤16 years | Source: WHO Vaccine-Preventable Diseases: Monitoring System, 2006 Global Summary
Application of these strategies has yielded the following coverage results, compared to other parts of the world:
Cuba’s immunization program has been evaluated twice by PAHO’s teams of experts (most recently in 2004) under the organization’s Expanded Program on Immunization (EPI). EPI teams assess a number of variables including a program’s reach, organization, and functionality, coverage rates, equity, as well as overall impact and monitoring.
In Fall 2004, a team of 14 experts headed by Dr Jon Kim Andrus of the Immunization Unit of PAHO’s Family and Community Health division traveled to Cuba. The EPI team reviewed policies, planning, and records at the national level; they also went to six Cuban provinces and their municipalities to review records, implementation, and impact. There, they interviewed not only health professionals, but parents too, to ascertain awareness about vaccination. The conclusions, according to Dr Lea Guido, WHO-PAHO Representative in Cuba, were that the program:
- Has had an important impact, eliminating several diseases and controlling others
- Has had an impact at the level of the public health system itself
- Is participatory
- Has a high level of organization
- Is known and understood not only by health professionals, but also by the general public, who in turn become spokespeople for broader education on the subject
“The conclusions of the report,” said Dr Guido, “note that the assessment also provided a learning experience for PAHO staff, and especially for those participating in the evaluation, since this vaccination program is exemplary in relation to other countries in the Third World, and also developed countries, because of its characteristics and its health impact.”[3]
Dr Guido also described several recommendations for Cuban health authorities contained in the EPI evaluation:
1. Make greater efforts to publish about the program in scientific journals, particularly regarding its strategies, lessons learned, and impact.
2. Carry out a feasibility study on the introduction of disposable syringes (including cost-benefit and disposal options).
3. Continue to defend the achievements of the program and results that are meaningful for Cuba and the Americas as a whole.[3]
These recommendations and other program needs have prompted health authorities to undertake several specific projects to buttress the NIP’s quality, continued impact, and sustainability. These include:
- A project funded by The Global Alliance for Vaccines and Immunization (GAVI) is under way (2006 to 2008) to guarantee safe injections by providing disposable syringes and safety boxes, plus incineration containers for their disposal. The project covers vaccination for all children aged ≤2 years for three years, after which the Cuban Public Health Ministry has committed to take over procurement.
- Modernization of the cold chain throughout all 14 provinces is in process, with the installation of new climate-controlled warehouses in all provinces, and new refrigeration capacities in all 494 vaccination sites around the country, over a three-year period.
International Implications of the Cuban Program
The presence of some 30,000 Cuban health professionals abroad, the majority staffing primary care facilities in public health systems in the developing world, has contributed to increased safety and coverage of vaccination drives in dozens of countries. A case in point is Haiti, where some 500 Cuban physicians are posted mainly in rural settings. From 1999 to 2001, in the midst of a major outbreak of measles, Haitian health authorities and PAHO organized an unprecedented vaccination campaign, which involved Cuban experts and their physician network, as well as UNICEF, the European Union, USAID, and Canadian and French aid agencies, among others. The initiative concentrated on measles and polio immunization, and later included other vaccine-preventable diseases.
“Coordinated by the Haitian Ministry of Health and with additional technical expertise,” noted Dr Guido, who was the WHO-PAHO representative in Haiti at the time, “a national house-to-house vaccination program was organized to control the epidemic…The Cubans’ willingness to cooperate, working with others, was an important element. That, plus the presence of Cuban doctors in the most remote and difficult places. [They] are in every municipality, every corner, and so could even vaccinate beyond the campaign itself, making it part of their healthcare routine.”[3]
Foreign students in Cuba – numbering some 24,000 in medicine alone – also receive full physical examinations and the following vaccinations: MMR (single dose); HepB (3 doses); TT (2 doses); and Men BC (2 doses).
For a historical review of immunization in Cuba, see: MEDICC Review. 2004;6(2). Available at: http://www.medicc.org/publications/ medicc_review/1004/index.html.
References
- Galindo, MA. Programa Nacional de Inmunización, Cuba. PowerPoint presentation at FINSA, November 2006, Havana.
- World Health Organization. Challenges in global immunization and the global immunization vision and strategy 2006-2015. Weekly Epidemiological Record. 2006;81(19):190-5.
- Interview with Lea Guido, MD, WHO-PAHO representative in Cuba, by Gail Reed, December 15, 2004, for a forthcoming book on the Cuban health system.