Organ and tissue transplantation extends a lifeline to patients across the globe. But access to this therapy of last resort is restricted by many barriers: access to health care in the first place, particularly to such high-tech procedures, limited by inequities in geography, gender, race/ethnicity or economic status, among others. Access is further influenced by health system organization; its human and material resources; cultural norms and religious beliefs; corruption and organ trafficking; and degree of public education, social cohesion and political will of governments.
Taken together, these factors make organ donation and transplantation one of the most complex health issues countries face, Cuba included. And the chain leading to successful outcomes is long and delicate, fraught with ethical, legal and medical dilemmas. Nephrologist Alexander Mármol, director of the Ministry of Public Health’s National Donation and Transplant Coordinating Office (ONCDT) notes that donors represent the first and vital link. “Without donors, there can be no transplants. You can have the greatest surgical team in the world, but they cannot fabricate an organ. The donors and their families are the real heroes.”
Experts such as Dr José García Buitrón, vice president of Spain’s Donation and Transplant Institute, share this view: “Donation is the key, and donation requires social commitment. Society’s role in this case—to return health to someone who is sick—is one health professionals are called upon to play with most illnesses. But in the case of transplants, society as a whole must do this…people…because they are the ones who donate.”[1]
He comes from the country with the highest per capita rate of donors and transplants in the world, even amidst budgetary cutbacks. Its deceased organ donor rate was 36 per million population (pmp) in 2014, with 4360 transplants performed.[2] This is far and away above other European countries, such as France at 26 pmp, or the United States at 27. And when it comes to developing countries, the figures plummet, with overall donors at 8 per million inhabitants in Latin America and even fewer for Africa, where data is too scarce to hazard a guess, but where chronic diseases—and thus transplant needs—are rising the fastest.[3]
Results: Organization is Key
Dr Rafael Matesanz, director of Spain’s National Transplant Organization (ONT), has analyzed the secrets of his country’s success: starting with the willingness of people to donate, the keys are precision organization of donation–transplantation–followup; professional teams that have mastered process, technology and technique; transplant coordinators in each participating hospital; and coordination conducted within a public health framework to avoid what he calls the “uncontrollably” complex web of private clinics and insurance companies in places like Germany, where donation rates have continued to fall.[2,3]

Dr Mármol: “Donors and their families are the real heroes.” / E. Añé
Cuba is following the Spanish path with increasingly positive results, applying some adjustments for both legal and cultural reasons. For example, while in Spain consent for deceased-patient donation is presumed (although Dr Matesanz says in practice, families decide), Dr Mármol explains that in Cuba, patient and family decision is required by law, and in fact, written permission must be notarized and included in the patient’s clinical record.
However, application of other educational and organizational norms shared with Spain are bringing results, the donor rate increasing from 8.0 pmp in 2013 to 14.3 in 2015.[4] This placed Cuba’s rates fourth in Latin America in 2014.[2,4] Interestingly, all regions of the country (eastern, central and western) are represented among provinces with the highest rates (Table 1).
As is the case globally, in Cuba, more kidney transplants have been performed than for any other organ, the first in 1970 (Tables 2 and 3). Later, other organs (as well as tissues such as cornea and hematopoietic cells, not covered in this article) were also included as soon as organization, training and technologies permitted. Multi-organ transplants have also been performed (including lung and pancreas, with other organs).
Ninety two percent of transplanted kidneys have come from deceased donors; as chronic disease deaths increase as a percentage of total deaths, kidneys and other organs from these patients are transplanted more frequently. Thus, the age of donors for all solid organs is also increasing: in 2013, the average organ donor age was 43.8 years (6.7% over 60 years of age), up to 47.3 in 2015 (13.8% over 60).[4]
Table 1: Deceased donor rates by province, Cuba (2013–2015)

Source: Mármol[4]
pmp: per million population
anew provinces created in August, 2010, Artemisa with parts of formerly larger Pinar del Río Province
bSpecial Municipality
Legal, Ethical & Organizational Framework
Various instruments define legal terms and ethical boundaries for organ transplantation in Cuba. For example a 2001 resolution formalizes the mandate that brain death, clinically determined by at least three physicians, be required for a patient to be considered for deceased organ donation. In these cases, as mentioned, the family makes the final decision to donate, expressed in successive interviews and in writing. They may revoke their decision at any time prior to surgery. The principle, as noted by Dr Mármol, is that “it is better to lose a donor than create a greater problem with and for the family, which must bear the burden of this decision.” Even so, Cuba’s 13% rate of permission denial is low compared to many other countries.[4]
Table 2: Milestones in solid organ transplantation, Cuba

Sources: Mármol, Villamil, Alonzo, Abdo[4–7]
CIMEQ: Medical–Surgical Research Center
HDCQHA: Hermanos Ameijeiras Clinical–Surgical Teaching Hospital
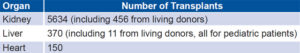
Table 3: Main solid-organ transplants in Cuba through March 2016
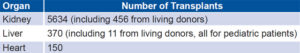
Sources: Mármol, Villamil[4,5]
Dr Mármol considers one reason for the low rate is the confidence families have that everything possible has been done to save their relative’s life. A family receives regular reports on its critically ill member, often many times daily, and thus is well aware of the care received prior to death. As is internationally stipulated, the physicians who sign the death certificate are never the same as the transplantologists. If a transplant occurs, anonymity is maintained between donating family and patient recipient.
As indicated by Spain’s evaluation of its own results, organization is vital for a successful transplant. In Cuba’s case, says Dr Mármol, this not only involves a highly trained multidisciplinary team of specialists, but also accreditation of hospitals and transplant coordinating units in the ones that most often care for critically ill patients. Thus, 51 hospitals in Cuba participate in the transplant network. Of these, 32 have transplant coordinating units (established in 2013) to assist in more efficient donor detection and recipient matching processes. Each unit is headed by an intensive care specialist, and includes one nurse and one psychologist. Such units have been flagged by Spain as essential to positive outcomes. Ten of the 32 hospitals are accredited to perform transplants (distributed across the country in the provinces of Santiago de Cuba, Holguín, Camagüey, Villa Clara and Havana).
Reporting to Dr Mármol’s ONCDT, coordinating centers in 5 geographical regions make up the core of Cuba’s transplant network, which covers all 15 provinces and the Isle of Youth Special Municipality. But this is only part of the story, insists Dr Mármol: successful transplant requires not only participation of health services, but also intersectoral collaboration to speed the organs to their destination in time, in optimal condition, and to ready the potential recipient and their family.
Matching: The Case of Kidney Transplants
A computerized algorithm analyzes the best match between a potential recipient and donor kidney, applying a mix of criteria to maximize the chance of compatibility and success. This includes HLA (human leucocyte antigen) testing, performed on kidney and recipient at the Cellular Immunology Center’s laboratory, complemented by a battery of other health indicators and tests validated by established protocols in conformity with international standards.[8] Then, since 1998, a centralized computer at the national Nephrology Institute goes to work to identify the best matches.
“Of the 3025 patients in dialysis, about 450 are on the transplant list, determined mainly by their overall health,” says Dr Mármol, who notes that waiting time is usually two to three years after beginning dialysis, but it can be more. “The algorithm not only helps us ensure the best compatibility between organ and recipient,” he says, “and also rules out bias.” Nevertheless, there are two exceptions: priority is given to children recipients for any kidney from a person under 40 years of age, as well as to ‘emergency zero’ patients whose lives are in immediate danger.
Once a match is established, the teams in donor and receptor hospitals swing into action, through their respective coordinating units and the national center, to minimize the time the kidney is ischemic, and thus maximize chances of successful transplant. Once the transplant is completed, and the patient released from the hospital, he or she is followed up locally by specialists and neighborhood family doctors and nurses. They also receive immunosuppressants “free of charge for life,” indicates Dr Mármol, who says the National Health System (NHS) spends about US$5 million annually on immunosuppressant medications for all transplanted patients (now living, approximately 1500), the amount spent on insulin for all of Cuba’s diabetics.”
Survival rates for patients with kidney transplants are 80% at 1 year, 50% at 5 years, below rates for high-income countries but improving over time, says Dr Mármol. Increasing five-year survival rates is important, as well as the total number of patients receiving transplants, since annual mortality for patients in dialysis is 18%.
He emphasizes the strict controls in place and the fact that all transplants are performed in NHS hospitals: “Here no one disappears from organ trafficking. People know that. It’s a transparent process, and people are aware of that, too.” Foreign patients may receive transplants only from living donors, and then only from other foreigners. In other words, Cuban organs are not used in foreign patients.
Challenges remain, primarily material in nature and affected by the US embargo, including importation of materials for molecular biology tests and opportunities for scientific exchange and training. Dr Mármol also says more and better public education about the importance of donating would make a difference in the program and make more transplants possible. Finally, the program as a whole faces out-migration of highly-trained personnel.
Liver, Living and Deceased Donors for Pediatric Cases
The first living-donor transplant in Cuba was of a kidney in 1979, becoming more routine a few years later. For much of this time, the practice was permitted only among close relatives (first-degree consanguinity). In 2015, given technological and organizational development, greater transplant needs and the fact that planning, speed and prognosis improve when living donors can be identified, Cuban law was changed to permit transplants involving spouses, unrelated children of recipient spouses, and up to fourth-degree blood relatives. These new “Regulations for Donation and Transplant of Organs and Tissues from Living Donors” cover the gamut of ethical and procedural requirements in these cases, with special attention given to confirming motivations of living donors, as well as fulfilling their rights and health care needs.[9,10]
Liver transplantation is particularly sensitive—a life-and-death matter, since there is no replacement therapy such as dialysis. When it comes to children, this becomes more sensitive still. Until the unit was established at Havana’s William Soler Pediatric University Hospital, Cuban children requiring liver transplants were taken to Spain, where the Cuban surgical team has also received training at La Paz Children’s Hospital in Madrid.
Havana’s 22-bed service, headed by Dr Ramón Villamil, is a mix of high-tech surgery suites, patient rooms carefully monitored for infection, and hallways dotted with posters of Cuban cartoon characters. There is also a recreation room, where I found three-year-old Leino Fabián Díaz, playing with his grandmother Marta Toranzo, who rotates with Leino’s mother, a store clerk, and father, a self-employed baker, as the boy’s in-hospital companion. Six days after his operation, she says his hyperactivity and other symptoms have all but disappeared. Leino’s condition also illustrates the service’s importance for children other than those needing transplants, his requiring surgical resolution of a congenital Abernethy malformation, the first case in Cuba. “The breadth of our team’s experience has saved many children,” says Dr Villamil.

Leino Fabián and his grandmother with Dr Villamil / E. Añé
Transplantation remains the unit’s core. Dr Villamil notes the service’s creation—involving years of preparation and training— and its connection to the national transplant network have made it possible for the team to transplant 68 patients since 2005 (54 receiving one organ, 13 receiving 2, and 1 receiving 3, for a total of 83 transplants). Patient ages range from 11 months to 18 years of age, and 28 were ‘emergency zero’ patients, requiring urgent transplant. These urgent cases put added stress on the team and its multisector allies, since a liver, even refrigerated, can only be deprived of oxygen for a few hours (cold ischemic time) before transplant, notes Dr Villamil.
And in acute situations, a living donor often becomes a must. Fortunately, liver compatibility relies primarily on blood group and a healthy donor and liver. However, Dr Villamil emphasizes that living-donor transplants bring their own complications, not the least of which is carefully ascertaining donor motivation, eligibility (including minimum age of 18 and health status) and followup care. “We have adapted UNOS (United Network of Organ Sharing, used in the USA), a national registry to manage our waiting list in real time, and our registry is always available for auditing,” says Dr Villamil. “We don’t go looking for donors, and when families propose donors, we take special care. We do have cases where we have had to protect proposed donors from family coercion.” The hospital’s Ethics Committee is required to emit an official document, indicating the donor is clinically appropriate, has gone through all four phases of evaluation (including psychological and psychiatric) and has provided written informed consent.

Dr Villamil (left) with part of his clinical-surgical team: “teamwork is essential.” / E. Añé
“Our goal is to preserve the donor’s health, giving them the best of care to avoid complications,” says Dr Villamil, noting that help comes from the liver itself, capable of regenerating sections extracted for transplant. But he adds that the vast majority of those willing to donate are not able to do so because other physical conditions, such as hypertension and smoking, put them at risk for extraction. In most cases, a cadaveric liver is first offered (if available), and final determination to recommend transplant to parents requires consensus of three liver-transplant teams (two adult and one pediatric), according to specific protocols.
For Cuban children in need of liver transplant, the most common reasons are cirrhosis, acute liver failure and other rarer diseases, some seen for the first time in Cuba, such as hepatopulmonary syndrome. Dayexi Guerra, 11, was transplanted due to a congenital condition; Pedro Fonseca, 14, due to cirrhosis. He was admitted for followup accompanied by his grandmother, who says his transplant has been “life changing” for her grandson, expected to live a normal life if he continues to take his immunosuppressants and is careful about infections.
In fact, Dr Villamil has cited nonadherence in patients reaching their teen years as one of the biggest problems facing the pediatric liver transplant program. “They see they are doing fine, so they first ‘forget’ to take their medications; they’re also more independent of parental controls and have other priorities. At first, nothing happens, but then they crash. We have lost patients this way.” Thus, local followup by specialists and family doctor–nurse teams becomes even more important, as well as by the service itself until patients reach 18, when their cases are transferred to adult care.
The results of the pediatric liver transplant service, expressed in the Kaplan-Maier model, show 89.3% survival at one year, 72.7% at two years and 70.1% at five years. In highly developed countries and programs, one-year survival is over 90%. Promising for Cuban patients is the fact that survival rates continue to improve: from 2006 to 2010, one-year survival was 71%, but from 2011 to 2015, it had increased to 90%. And average length of patient hospital stay, once 30 days, has been reduced to 15.
Reflections
While Cuba’s results are heartening, especially the increase in donor willingness and survival rates, as well as lifetime no-cost care for recipients and living donors, more use of media could increase public awareness and sensitivity to this rising need. Spain’s contribution, and that of Dr Rafael Matesanz who will retire shortly as head of its National Transplant Organization, deserve enormous credit for not only providing a model national program for Cuba and the world, but also training for transplant teams globally—aiming to revert the sobering reality that only 10%–12% of people who need transplants actually receive this lifesaving care.
References

- Céspedes Hernández L, Fariñas Acosta L. Granma dialoga con el profesor y cirujano español José García Buitrón en el marco del Curso Intermedio en Coordinación de Trasplantes, desarrollado en el hospital Hermanos Ameijeiras de la capital. Granma [Internet]. 2015 May 4 [cited 2016 Apr 1]. Available from: http://www.granma.cu/2015-05-04/una-sabia-decision. Spanish.
- The World Transplant Registry, which manages the Spanish ONT, says 118,117 transplants were performed worldwide in 2014, an increase of 3%. 2015 Sep 1 [cited 2016 Apr 2]. Available from: http://www.lamoncloa.gob.es/lang/en/gobierno/news/Paginas/2015/20150901-world-transplant.aspx
- Badcock J. How Spain Became the World Leader in Organ Donations. Newsweek [Internet]. 2015 Feb 11 [cited 2016 Apr 1]; [about 7 screens]. Available from: http://www.newsweek.com/2015/02/20/spain-has-become-world-leader-organ-donations-305841.html
- Data provided by Dr Alexander Mármol to the author, based on records of the Ministry of Public Health’s ONCDT. 2016 Mar 31.
- Information provided to the author by Dr Ramón Villamil, Chief of the Hepatobiliary and Transplant Service, William Soler University Pediatric Hospital, Havana. March 30, 2016, from hospital records.
- Alfonzo JP. Four Decades of Kidney Transplantation in Cuba. MEDICC Rev [Internet]. 2013 Jan [cited 2016 Apr 3];15(1):23–8. Available from: http://www.medicc.org/mediccreview/index.php?issue=23&id=289&a=vahtml
- Abdo AA. Trasplantes de órganos en Cuba: reseña histórica. Infomed [Internet]. Havana: Ministry of Public Health (CU); c2016 [cited 2016 Apr 16]. Available from: http://www.sld.cu/sitios/trasplante/verpost.php?blog=http://articulos.sld.cu/trasplante&post_id=16&tipo=1&opc_mostrar=2_&n=dbd. Spanish.
- See http://www.sld.cu/sitios/trasplante/ for further details.
- Ministry of Justice (CU). Gaceta Oficial No. 33 Extraordinaria. 17 Sept 2015. Ministerio de Salud Pública Resolución No. 857. Gaceta Oficial de la Repú-blica de Cuba [Internet]. 2015 Sep 17 [cited 2016 Mar 30]. Havana: Ministry of Justice (CU). 5 p. Available from: http://files.sld.cu/trasplante/files/2015/10/gaceta_go_x_33_20156.pdf. Spanish.
- Ministry of Justice (CU). Gaceta Oficial No. 43 Extraordinaria. 23 Dic 2015. Ministerio de Salud Pública Resolución No. 979. Gaceta Oficial de la República de Cuba [Internet]. Havana: Ministry of Justice (CU). Available from: http://www.gacetaoficial.cu/pdf/GO_X_43_2015.rar. Spanish.